Translate this page into:
Telogen effluvium
Correspondence Address:
Chander Grover
420-B, Pocket 2, Mayur Vihar, Phase 1, Delhi - 110 091
India
| How to cite this article: Grover C, Khurana A. Telogen effluvium. Indian J Dermatol Venereol Leprol 2013;79:591-603 |
Abstract
Telogen effluvium (TE) is one of the most common causes of diffuse nonscarring hair loss. In its acute form, it generates a lot of anxiety in the patient, which can be significantly allayed with a confident diagnosis. In its more chronic form, however, the hair loss may go unnoticed for long periods of time. Here in, the dermatologist's role in differentiating it from the more common patterned hair loss is significant. Differentiating TE from other causes of diffuse nonscarring hair loss can indeed be a daunting task and TE is often used as a waste basket diagnosis. A number of factors have been implicated in the causation of TE, however, clear evidence in their support is lacking. The role of stress as a causative factor as well as the result of hair loss needs to be adequately understood. This review aims at summarizing our current level of knowledge with respect to this very common cause of hair loss. An attempt is made to help the readers reliably differentiate TE from other causes of diffuse nonscarring hair loss. The possible causative factors, pathogenetic mechanisms, clinical presentation, and possible treatment options are discussed.Introduction
Hair loss or alopecia is a very common complaint. However, a rational and comprehensive classification system of various causes based on etiopathogenetic principles is still lacking. [1] Alopecia can be divided into disorders where either hair growth cycle is abnormal or the hair follicle is damaged. [2] This article reviews telogen effluvium (TE), one of the most common cause of alopecia, with regards to its pathogenesis, clinical findings, and current options of treatment.
Definition
Diffuse cyclical hair loss (DCHL) was the initial term used to describe discrete transitory episodes of reversible, diffuse hair shedding, improving with corticosteroids. [3] The term TE was first coined by Kligman to describe increased shedding of normal club hairs, with the hypothesis that irrespective of the cause, the follicle tends to behave in a similar fashion by undergoing a premature termination of anagen, precipitating telogen. [2],[4] It is an abnormality of hair cycling [5] occurring as a reaction pattern to various physical or mental stressors. [6] The degree of effluvium depends on the severity and duration of exposure, rather than on the type of agent. [7] Unexplained individual variations in susceptibility could also be responsible. [8]
TE is caused by any disruption of hair cycle resulting in increased, synchronized telogen shedding. [9] Headington described five functional types of TE. [10] Whiting described chronic telogen effluvium (CTE) as a primary, idiopathic entity. [11] Gilmore and Sinclair suggested that CTE may be secondary to a reduction in the variance of anagen representing a distinct functional type. [3]
Epidemiology
As most of the cases of TE are subclinical, its true incidence or prevalence is largely unknown. [5],[12] Among those seeking treatment, women are over-represented, probably due to unawareness or underreporting in males. ATE can occur in either sex if the proper inciting conditions occur. However, as hormonal changes in the postpartum period are a common cause of TE, women may have a greater tendency to experience this condition. In addition, women tend to find the hair shedding more troublesome than men do; thus, more women seek medical attention for the condition. It is estimated that telogen gravidarum (TG) affects one-third to one-half of women following childbirth. The effect of age is also unclear, with elderly women being reported to be more susceptible to acute telogen effluvium (ATE) following high fever, surgical trauma, severe hemorrhage, or immense psychological stress. In children, TE has been reported to be responsible for only a minority of cases with hair loss (2.7%). [13]
For reasons that are unclear, CTE seems to affect only women. [11] This fact is also borne out in a study on a population of squirrel monkeys (Saimiri boliviensis boliviensis) in a breeding facility, which showed only females to be affected. [14] A randomly selected sample of 100 female and 10 male animals revealed a normal hair coat in 35 female monkeys and all 10 male animals in spite of the fact that there were no statistically significant differences in body weight, hemoglobin, blood urea nitrogen, serum glucose, liver aspartate amino-transaminase, or free thyroxine levels. [14] The findings on histopathology were consistent with CTE. CTE also appeared to be an age-related problem in this population. [14] In humans as well, CTE is a problem in middle-aged women. It usually affects women aged 30-60 years and starts abruptly with or without a recognizable initiating factor. It may be distinguished from classic ATE by its long fluctuating course and from androgenetic alopecia (AGA) by its clinical and histologic findings. [11]
Etiopathogenesis
The normal hair follicle activity is cyclical, consisting of anagen (hair growth phase); catagen (involution phase); telogen (dormant phase); and exogen (release phase occurring in late telogen or early anagen). [8] A telogen hair remains in its follicle for up to 4-6 weeks after the onset of anagen. This cycle results in the replacement of every hair on the scalp every 3-5 years, with individual follicles undergoing 10-30 such cycles in a lifetime. [5],[15]
While follicles undergo individual cyclical activity, the entire follicular population on the scalp, simultaneously undergoes another cyclical activity, which may be synchronous (all neighboring hair grow and are shed together within an anatomical region) or asynchronous. In humans, synchronous hair growth disappears in childhood. [1] An average normal scalp has 100,000 hairs, with approximately 86% being in anagen, 1% in catagen, and 13% in telogen. [16],[17] With TE, the ratio shifts to 70% anagen and 30% telogen, with daily shedding of up to 300 hairs. [17] However, it must be kept in mind that the degree of disability due to hair loss varies widely from patient to patient and does not always accord with the objective assessment of hair shedding. [18] The underlying mechanisms for this common endpoint of telogen shedding may be entirely different in different cases. Headington described five functional types of TE. [10]
- Immediate anagen release occurs when follicles are stimulated to leave anagen and enter telogen prematurely, resulting in increased TE 2-3 months later. [10] This can be seen with physiologic stress, severe illness, or drug-induced hair loss. The reversal of stress is associated with resumption of normal cycle
- Delayed anagen release is due to prolongation of anagen resulting in delayed but synchronous onset of heavy telogen shedding. The most common example is TG, where anagen prolongation occurs under the effect of pregnancy hormones. A similar state occurs after discontinuation of contraceptive pill. [19],[20] Postpartum, the hormonal drive is removed and many hairs shift to telogen, resulting in increased shedding 3-4 months later [19],[21]
- Immediate telogen release generally occurs with drug-induced shortening of telogen leading to follicles reentering anagen prematurely. Hence, a massive release of club hairs (exogen) occurs as is seen when starting therapy with minoxidil
- Short anagen syndrome is characterized by an idiopathic shortening of anagen duration, leading to persistent telogen hair shedding. [10] This mechanism is considered responsible for majority of cases with CTE with mild persistent hair loss and inability to grow the hair long [3]
- Delayed telogen release is characterized by a prolonged telogen and delayed transition to anagen. It occurs in animals with synchronous hair cycles but may be responsible for seasonal hair loss in humans. [10]
Gilmore and Sinclair extensively studied the follicular dynamics of CTE and suggested that it is a distinctive pathological state, secondary to a reduction in the variance of anagen, representing a possible sixth functional type of TE. [3] This means to say that although the average length of anagen may remain the same (unlike AGA), the increased hair shedding is because of the fact that the variation of anagen length across all follicles (maximum to minimum) tends to reduce in CTE. The trigger for this persistent change in follicular dynamics is unknown. [3]
Follicular stem cell apoptosis induction has also been implicated in the pathogenesis of TE with HIV-1 viral protein R being proposed as an inductor. [22] Diffuse alopecia occurs in almost 7% of HIV-1-infected patients with TE being the main diagnosis. Scalp biopsies from these patients revealed apoptosis of follicular stem cells at the bulge region. [22]
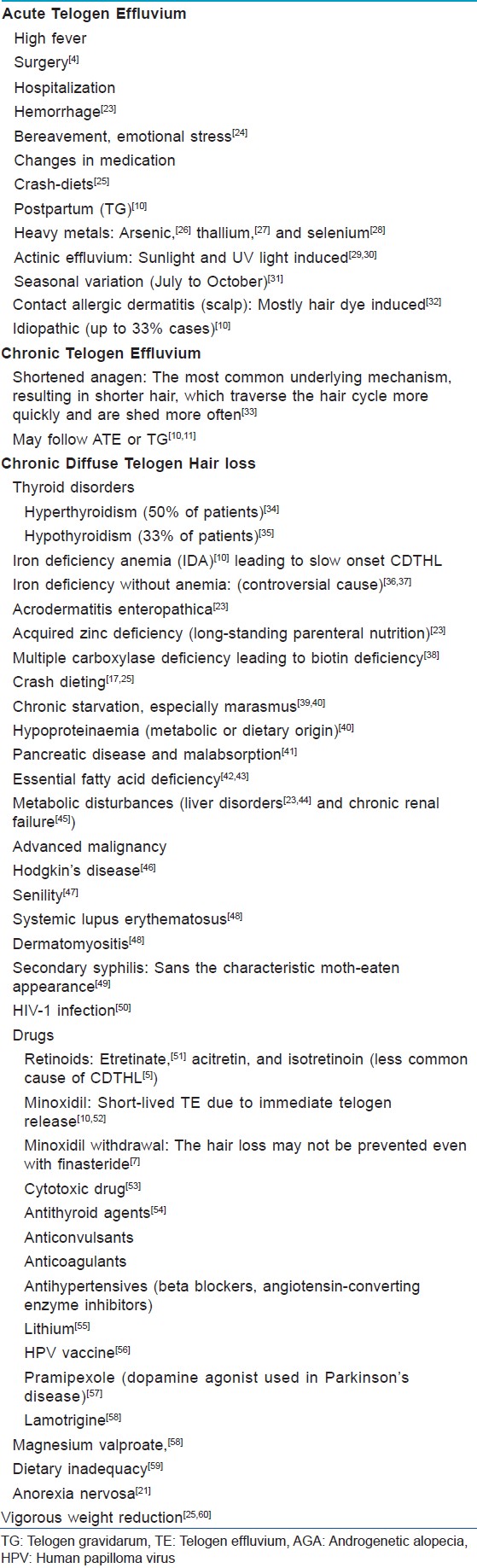
For ease of comprehension, various underlying triggers possibly leading to telogen hair shedding (ATE, CTE, or chronic diffuse telogen hair loss [CDTHL]) are summarized in [Table - 1]. [Table - 2] summarizes the most relevant investigations for a case with ongoing telogen hair loss.

Acute telogen effluvium
ATE was first described as an acute onset scalp hair loss occurring 2-3 months after a triggering event, which could be unidentifiable in up to 33% cases. [5],[10] The important causes are summarized in [Table - 1]. The functional mechanism of shedding in majority of these cases is immediate anagen release. [10] TG (ATE seen 2-5 months after childbirth) is a distinctive form associated with pregnancy and childbirth. [10],[21] A seasonal increase in TE is a frequent complaint, however, it has not been reliably evaluated scientifically. Piérard-Franchimont and Peérard found an increased frequency of TE between July and October. [31] They proposed that it could be an actinic effluvium, a summer effect possibly ultraviolet (UV) light induced, manifesting itself in autumn, in predisposed individuals. [31] More scientifically validated studies are needed to help validate this issue. The possible role of photoexposure/sunlight in the pathogenesis of AGA has also been proposed by Trueb. [29] The author proposed various possible mechanisms, which could apply equally well for TE. The production of porphyrins by Propionibacterium sp. in the pilosebaceous duct leading to oxidative tissue injury and follicular microinflammation; keratinocyte response to physicochemical stress from ultraviolet radiation (UVR); irritant and pollutant-induced radical oxygen species and nitric oxide; or release of proinflammatory cytokines damaging follicular stem cells could be responsible. [29] Transmission electron microscopy of hair exposed to sunlight indicates alteration of cell components and damage occurring in cuticle as well as cortex. [30] Other changes include formation of carbonyl groups, cystine destruction, modification of the proteins obtained by reduction of the disulfide bonds, losses in mechanical strength, and discoloration. [30] However, how much of this is actually responsible for increased telogen hair loss is not scientifically proven.
Patients generally present with complaints of increased hair loss while washing or brushing. [33] They may even bring in bags of shed hair to demonstrate the quantity of loss [Figure - 1]. They are often very anxious that they will go bald if this continues. Few may have noticed bitemporal thinning. [33] Shorter, regrowing frontal hair may be seen in patients with resolving effluvium. Pertinent questions about the onset and possible triggering events may be fruitful. On examination, there is an essentially normal scalp with complete absence of inflammatory signs or follicular miniaturization. The trichogram reveals an increase of telogen hairs (>25%). [1]
 |
| Figure 1: A 28-year-old female complaining of heavy hair loss for the past one month. However, an essentially normal visible hair density and a normal scalp can be appreciated. Patient is demonstrating the amount of hair lost in one comb |
ATE usually remits within few months in 95% of cases. A small proportion of TG cases may experience persistent, episodic shedding as some follicles may not revert to an asynchronous growth pattern. [8],[10] A full recovery may also be compromised in senile women due to the concurrence of AGA and aging of follicles. [78] In addition, ATE not remitting for prolonged periods may actually be early AGA or diffuse alopecia areata. [79] Moreover, on many occasions, an episode of ATE may unmask an underlying AGA [Figure - 2].
 |
| Figure 2: A 54-year-old female complaining of increased hair loss and thinning for the past 2 months. The scalp shows visible hair thinning with a broad parting (suggestive of FPHL). Simultaneously, temporal thinning of hair with shorter regrowing frontal hair can be appreciated (suggestive of acute telogen effluvium) |
Chronic telogen effluvium
CTE is a primary, idiopathic condition affecting middle-aged women, which needs to be differentiated from CDTHL secondary to organic causes and AGA. It presents as TE lasting more than 6 months, without any widening of central part or follicular miniaturization. [8] The disorder appears to be distinct from ATE because of its prolonged, fluctuating course. [8] Although, some cases of CTE may follow ATE with a known trigger, in most cases a specific trigger cannot be identified. [5] The telogen hair shedding seen in CTE could be a result of almost any of the functional types described earlier. However, a shortening of anagen is the mechanism most commonly involved. [10]
Clinical features include an insidious onset and a fluctuating course lasting for several years. It typically affects middle-aged women who are grossly disturbed due to an overall decrease in their hair length as well as volume. [80],[81] However, on examination, the hair appears normal in thickness, with shorter regrowing hairs in the frontal and bitemporal areas. Few patients may have a marked bitemporal recession [Figure - 3] and [Figure - 4], [Figure - 5]. Hair pull test is commonly positive.
 |
| Figure 3: Bitemporal thinning of hair in a female 4 months postpartum (telogen gravidarum). Minimal regrowing frontal hair can also be seen |
 |
| Figure 4: A 36-year-old female with complaints of increased hair fall for the past many years. Temporal thinning with a marked regrowth of smaller hair can be appreciated |
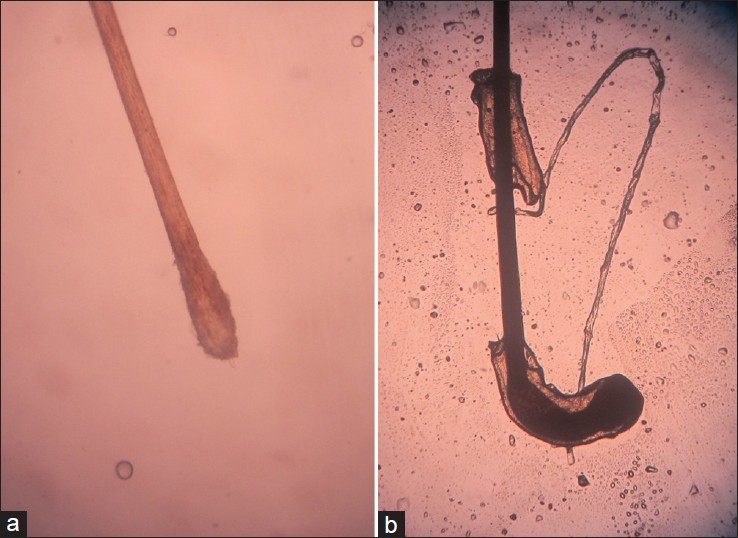 |
| Figure 5: Hair microscopy. (a) A telogen hair follicle with a non-pigmented cornified and rounded up bulb. No attached root sheath seen (b) An anagen hair follicle with a darkly pigmented, somewhat distorted and malleable, elongated bulb. The attached root sheath can be appreciated |
A diagnosis of CTE requires exclusion of other causes of CDTHL with the help of a thorough history and full clinical examination. The routine work-up includes full blood count, and thyroid function tests. Syphilis serology, antinuclear antibody (ANA) titer, serum zinc levels, and other investigations may be performed, if indicated. [80]
The important differential to be entertained is AGA. [82] Histological differentiation is possible [Table - 2] on the basis of follicular miniaturization, the hallmark of AGA. A T: V ratio of less than 4:1 is considered pathognomonic of AGA, whereas a ratio greater than 8:1 indicates CTE. [70],[83] A biopsy of CTE will show an anagen: telogen ratio (A: T) of 8:1 compared with 14:1 from normal scalp. [84] Sinclair et al. evaluated 600 women presenting with chronic diffuse telogen hair shedding with little or no reduction of visible hair density. Of these, 60% were found on scalp biopsy to have hair miniaturization consistent with a diagnosis of AGA and 40% had CTE. [70]
Although it is widely believed to be a self-limited disease, the natural history remains poorly characterized. [5],[85] Harrison and Sinclair reported that biannual repeat scalp biopsy done on women originally diagnosed with CTE have led to subsequent reclassification as AGA in a substantial number of cases, [5] albeit the follow-up time was relatively short. Whether there is an actual increased incidence of AGA in women with CTE compared with the normal population is unknown. Sinclair et al. followed up five women with telogen shedding for over 7-8 years. Of these, only one was reclassified as AGA, 18 months into follow-up on the basis of histopathological evidence. The others continued to have fluctuating hair loss over the years, without an overall reduction in scalp hair density. [85] This longitudinal study clearly shows that CTE is a distinct clinical and histological entity, and not a prodrome to AGA. CTE may have a favorable prognosis despite ongoing hair fall with only a minimal reduction in average long-term hair volume. [86] The condition could spontaneously resolve after a decade or so. [85]
Chronic diffuse telogen hair loss
CDTHL refers to telogen hair shedding, longer than 6 months, secondary to a variety of organic causes. To be a true cause of CDTHL, the relationship between the trigger and the TE must be reversible and reproducible. The requirement of proof includes exclusion of other known causes of shedding in particular AGA, reversal of effluvium following correction of causative factor, and relapse on rechallenge. [5]
Causes of CDTHL are summarized in [Table - 1]. Prominent ones include thyroid disorders, profound iron deficiency anemia (IDA), acrodermatitis enteropathica, and malnutrition. [23] CDTHL seen in thyroid disorders is generally reversible when euthyroid state is restored, except in long-standing hypothyroidism where hair follicles may have atrophied. [35],[86] Thyroid peroxidase antibodies have been demonstrated in a significant percentage of TE patients. [87]
Profound IDA (one of the most common nutritional deficiency worldwide) can cause CDTHL as telogen follicles fail to reenter anagen. [10] Follicular matrix cells are among the most rapidly dividing cells and hence, are exquisitely sensitive to any minor decrease in iron availability (cofactor in DNA synthesis). [88] This can generally be corrected by iron replacement. However, the relationship of hair loss with iron deficiency without anemia or only mild anemia is more complex and controversial. [36] Several studies have examined this relationship with some suggesting that iron deficiency even in the absence of IDA may lead to hair loss. A more definitive study, found neither increased incidence of iron deficiency in 77 women with CDTHL nor any decrease in shedding with effective iron therapy. [77] In an excellent review by Trost et al., insufficient evidence was found for either recommending universal screening for iron deficiency or for iron supplementation in hair loss with absence of IDA. [36] The decision to do either, should be based on clinical judgment. However, the treatment for hair loss is enhanced when patients maintain a serum ferritin concentration greater than 70 ng/mL. [36] A diagnosis of iron deficiency is based on hemoglobin concentration (routine but not reliable test) or serum ferritin concentration (confirmatory for iron deficiency). [3] Serum ferritin concentration of 10-15 ng/mL is mostly used as a cut-off for diagnosing iron deficiency. However, a cut-off of 41 ng/mL yields a sensitivity of 98% and a specificity of 98%. [89] Interestingly, serum ferritin may be elevated in anemia of chronic disease. [90] Hence, additional tests of iron status including erythrocyte zinc protoporphyrin concentration, transferrin concentration, serum iron concentration, and transferrin saturation may be required. The cause of iron deficiency must also be identified to ensure effective management.
Zinc deficiency can lead to a severe CDTHL. [23],[91] However, CDTHL alone, with no other symptoms or signs is never due to dietary zinc deficiency. [5] Any correction of a subclinical zinc deficiency may not help. Infants with acrodermatitis enteropathica or multiple carboxylase deficiency with CDTHL, can be helped with dietary supplementation of zinc or biotin, respectively. [88] Diet has an important role to play in TE. [59] Rigorous dietary restriction or crash dieting (<0.8 g/kg protein and 1200 Kcal/d) can lead to inadequate supply to the hair matrix and precipitate telogen hair loss. [25],[60] Chronic starvation especially marasmus causes a diffuse telogen hair loss often accompanied by hair shaft abnormalities. [92] Hypoproteinemia of metabolic as well as dietary origin can cause hair loss. Pancreatic disease and other forms of malabsorption also cause a diffuse telogen hair loss, [23] as does the essential fatty acid deficiencies seen in prolonged parenteral nutrition and hypervitaminosis A. [42],[43]
Although many drugs have been implicated in causing TE there are no controlled studies examining possible causal relationship. [93] Drugs can induce hair loss by inducing an abrupt cessation of mitotic activity (anagen effluvium) or by precipitating follicles into premature rest (TE). [7] Drug-induced CDTHL, usually starts 6-12 weeks after instigation of treatment and is progressive while the drug is continued. [94],[95] The most common implicated mechanism is immediate anagen release. [10] If a particular drug is suspected, testing involves suspending its use for at least 3 months. Regrowth following discontinuation and recurrence on re-exposure to the drug helps conclude a causal role of the drug. [5] Many drugs, reported in literature, may not fulfill the above criteria. It may recur with chemically unrelated drugs, suggesting that true cross reactivity is rare, and individual susceptibility exists to drug-induced CDTHL. The effect may be dose-related as with retinoids (Cause a telogen anchorage defect and reduce the duration of anagen). Cytotoxic drug-induced hair loss has been classically ascribed to anagen effluvium (loss of fractured hairs). However, conflicting views have been reported with Bleiker et al. suggesting that the effluvium comprises of a mixture of tapering telogen hairs and fractured hairs, and may be regarded as a variant of the conventional TE. The term ′atrophic TE′ has been used to describe this phenomenon. [53]
Psychosocial impact
Physicians should be careful not to underestimate the emotional impact of hair loss. [24],[55] It provokes anxieties and distress more profound than its objective severity would appear to justify. For some patients, the burden of hair loss may be comparable to more severe chronic or life-threatening diseases. [95],[96] Conversely, emotional stress is commonly attributed as a cause of TE at several levels. [97],[98],[99] Thus, stress may act as a primary inducer; an aggravating factor (in hair loss due to primary endocrine, toxic, metabolic, or immunological causes); or be a response to hair loss (contributing to aggravation and inducing a self-perpetuating vicious circle). [24] Stress is likely a negative hair growth modulator with possibly profound effects in humans. [100],[101] The catagen-inducing and hair-damaging proinflammatory mediators possibly involved are substance P (SP); corticotrophin releasing hormone; central hypothalamic stress hormone, and stress associated nerve growth factor (NGF). [100],[101],[102],[103],[104],[105],[106],[107],[108],[109]
The hair follicle acts as a prominent source as well as peripheral target organ for many bioregulatory molecules recognized as mediators of stress responses. [98],[99],[102],[103],[104],[107],[110] Catecholamines, prolactin, and NGF, the three classical bioregulators of systemic stress response, are known to modulate hair cycle. [110] The follicle itself can generate stress mediators; express receptors and thus, be directly involved in the local modulation of systemic stress response, acting as a part of "skin stress system." [110] Specific SP receptor (NK 1) antagonist have been shown to reverse stress-induced hair growth inhibition and follicle damage seen in mice. [102],[103],[108] Based on this, NK1 antagonists were proposed as a potential new class of antidepressive drugs. [108] Aprepitant is the only available molecule from this group and has already been studied and tried in migraine, asthma, nausea, inflammatory bowel syndrome, urinary incontinence, anxiety, and depression, but has not been tried in CTE per se. [109] Besides SP, other neurotransmitters, neuropeptides, neurohormones, and neurotrophins are being considered as potential local or systemic mediators of stress-induced hair growth inhibition.
Diagnostic approach
Although hair loss seems to be a daunting disorder to evaluate, breaking down the history, examination, and discussion into digestible parts makes the experience easy. [111] These patients often are the most appreciative lot when they are simply helped through their frustrations. Chartier et al. described the "SOAP" pattern for differentiating four common causes of diffuse nonscarring alopecia. [112] S (subjective complaints) in the form of loss of excessive hair, clogging shower drain or comb, points toward TE as a cause. The patient should be asked about specific triggers 2-5 months before the onset. The duration of shedding and its course (improving or waxing and waning) should be evaluated. ATE is likely to be related to a specific event, whereas gradual, prolonged hair loss is more difficult to assess. O (objective features) may be totally absent or there may be diffuse overall thinning with normal part width. Short frontal hairs and bitemporal thinning are important suggestive signs. Any evidence of erythema, scaling, inflammation; altered hair density or distribution; changes in shaft caliber, length, shape, or fragility may suggest other diagnoses. [112] A (assessment) should include relevant investigations as outlined in [Table - 2]. P (plan ) should be based on the diagnosis, as outlined in the treatment section.
A potentially important but ambiguous symptom associated with hair loss may be trichodynia. It refers to pain, discomfort, and/or paresthesia in the skin of the scalp or the hair. [113] Kivanç-Altunay et al. evaluated the presence of trichodynia in patients with TE or AGA, comparing it with controls and performing a psychiatric evaluation additionally. [113] Trichodynia was present in 29% patients with hair loss and 3.3% controls (P < 0.0001). It was more frequent in TE patients as compared with those with AGA (P < 0.0071). However, it often coexisted with psychopathologic findings. [113] Baldari et al. reported trichodynia to be significantly more prevalent in patients with TE and TE along with AGA (P < 0.001) as compared with any other diagnoses. They proposed that trichodynia is almost exclusively seen in patients with active TE and spares those in remission and may be a marker of an active inflammatory peripilar process (similar to alopecia areata [AA]). [114]
Differential diagnoses
Early female AGA can be difficult to distinguish from CTE and CDTHL as discussed earlier. The differentiating feature can be the chronic and relapsing hair loss with generally incomplete recovery. A well-directed punch biopsy can usually clarify the diagnosis. [3]
Alopecia areata incognito is a poorly characterized variant of AA characterized by an acute diffuse hair thinning. The differential diagnosis with TE and diffuse AA may be difficult. It presents with an intensely positive pull test and trichodynia but with minimal, if any rarefaction of hair. [112] Exclamation mark hairs are rarely observed. This pattern of AA incognito presents with localized hair thinning without bald spots. Histopathology is typical of AA with peribulbar lymphocytic infiltrates. [112]
Psychogenic pseudoeffluvium is included as a body dysmorphic disorder (Dysmorphophobia), the central criterion being an excessive preoccupation with a deficit/disfiguration in physical appearance, which either does not exist at all or is only extremely slight. [115] This leads to marked limitations in social, professional, and also functional areas. Women aged between 35 and 50 and men aged less than 35 years are affected. As an essential criterion, the clinical examination shows no pathological findings or only minimal variation from normal. [115] Hence, with an objectively normal TE, there may exist a psychogenic pseudoeffluvium (as a body dysmorphic disorder). Not all patients with TE have psychogenic pseudoeffluvium because the increased telogen count and hair loss is objectively measurable. However, the minority, who are concerned out of proportion with their hair loss, can be said to be suffering from this disorder. [115] Similarly nihilodermia refers to difficult patients without objective findings but with recurrent symptoms and stubborn demand for medical examination. [116] It is a primary emotional disorder, but patients usually strictly deny a psychosocial aspect and expect purely somatic treatment. One of its common clinical pattern is psychogenic pseudoeffluvium. [116]
Investigations
It is optimal to follow established guidelines for considering and excluding the chief causes of TE. [6] Using pattern recognition and focusing on pathogenetic principles, [6] appropriate diagnostic procedures can be chosen and used as summarized in [Table - 2].
Treatment
Treatment for TE is primarily reassurance and counseling. If attempts at identifying a specific cause have been fruitful, one should correct them. An expectant management and observation are usually appropriate as shedding is expected to cease within 3-6 months and thereafter recovery should be complete. [17],[84]
Patient′s frustrations should be addressed [117] and an assurance that TE will not lead to baldness is helpful. Frustration generally arises from the inability to comprehend that a completely healthy person can still have hair loss; that hair loss could be a result of untreated medical concerns; and that mixed forms of hair loss can exist. [111] Women undergoing chemotherapy form an important group who may benefit from psychological counseling. [118] The patient usually would have searched the internet, seen several hairstylists, and potentially consulted more than one physician. [111] One has to deal with many myths and misinformation surrounding hair loss. The patient needs a brief discussion explaining the diagnosis and treatment options. Being a cosmetic concern, the degree of disability due to hair loss varies widely. [111] Psychosocial counseling has been claimed to be the best treatment as it is the safest and least invasive way to address the psychosocial impact. [84] Hair regrowth being slow (1 cm per month); the patient should be counseled to have appropriate expectations .
Based on the pathogenesis of TE, potential therapeutic options include inhibition of catagen (so as to prolong anagen); induction of anagen in telogen follicles; or inhibition of exogen (to reduce hair shaft shedding). [6] Neither of the currently available Food and Drug Administration (FDA) approved standard hair drugs (finastetride and minoxidil) are highly efficient catagen inhibitors or anagen inducers. [6] However, what can assuredly be done is the exclusion of catagen-inducing drugs (beta-blockers, retinoids, anticoagulants, or antithyroid drugs) or catagen-inducing endocrine disorders (thyroid dysfunction, hyperandrogenism, or hyperprolactinemia). Substitution therapy for catagen promoting deficiencies like those of iron, zinc, estradiol, or proteins can also be initiated. [84],[119]
At this time, there are no proven vitamins or supplements for any form of hair loss. [111] If there is a measurable deficiency such as IDA, then its replacement may help. However, a balanced diet and stable body weight are most important measures. Biotin supplementation has been shown not to affect TE. [111] Controlled studies regarding efficacy of replacement of iron or thyroxine on the outcome of TE, are also lacking, although some benefit has been claimed. [5] It has been suggested that maintaining serum ferritin above 40 ng/dL [119] (70 ng/dl by some authors [36] ) helps reverse hair loss. An adequate dietary intake and, if required, oral ferrous sulfate, 300 mg (60 mg elemental iron) taken 3-4 times daily is a widely accepted and cost effective initial therapy. [117],[120],[121] It should lead to rise in hemoglobin concentration by 2 g/dL in 3-4 weeks. [121],[122] In cases with poor response, causes like poor compliance, misdiagnosis, malabsorption, coexisting anemia, and continued blood loss should be assessed. [121],[122] Iron supplementation needs to be continued for 3-6 months until iron stores are replenished. [120],[121],[122],[123] Unnecessary long-term iron supplementation can lead to iron overload. [123] The proposed role of antioxidants or other supplements has not been proven by any creditable evidence. Green tea (containing polyphenolic compounds) has been reported to improve patchy hair loss in mice. [124] However, no controlled studies are available in humans.
TE often uncovers female pattern hair loss (FPHL), bringing the patient in for shedding and thinning on the crown. [111] This is the most common combination of hair loss and should be addressed with reassurance if the telogen is still occurring, followed by examination 6 months later for improvement. Treatment of FPHL can be started if hair loss has not started to improve by the 6-month follow-up. [125]
A novel cosmetic treatment for thinning hair in TE has been reported by Davis et al. [126] It comprises of a leave-on technology combination (caffeine, niacinamide, panthenol, dimethicone, and an acrylate polymer [CNPDA]), which significantly increases the diameter of individual, existing terminal scalp hair fibers by 2-5 μm, yielding an increase in the cross-sectional area of approximately 10%. Beyond the diameter increase, the CNPDA-thickened fibers demonstrated the altered mechanical properties characteristic of thicker fibers and better ability to withstand force without breaking. [126] However, its efficacy in TE remains to be established.
No specific therapeutic intervention, which could prevent stress-induced premature onset of catagen, is currently available for stress-induced TE. [127] Topical minoxidil could be a reasonable candidate drug in this category as it is known to prolong anagen. [128] In addition, in vivo studies in mice have demonstrated that minoxidil can downregulate stress-induced hair growth inhibitory and catagen promoting changes along the "brain-hair axis." [102],[103] Its clinical efficacy in humans with respect to TE remains to be investigated. In addition, stress-coping strategies may help, however, controlled data in this respect is lacking. Complex, comprehensive, and careful management beyond drug prescription in order to alleviate clinical symptoms and the concomitant psychological implications may go a long way in helping the patients. [24]
Conclusion
TE is a common cause of diffuse hair loss. ATE can usually be diagnosed on history and examination. It is a self-limiting event and hence, observation until spontaneous resolution is generally professed. Further investigations may be required only when the shedding is severe or prolonged. A diagnosis of CTE warrants ruling out other causes of CDTHL, including AGA, drug-induced hair loss, IDA, hypo- and hyperthyroidism, and chronic diseases. An effective differentiation from AGA can guide appropriate choice of long-term therapy. Possible treatment options for TE, especially the chronic form, are not many. The outcomes have improved as we have gained more knowledge about the factors that control hair follicle cycling. Ongoing clinical and basic research has the potential to improve our understanding of this very common disorder, even further.
| 1. |
Wiedemeyeer K, Schill WB, Loser C. Diseases on hair follicles leading to hair loss part I: Nonscarring alopecias. Kinmed 2004;3:209-14.
[Google Scholar]
|
| 2. |
Thiedke CC. Alopecia in women. Am Fam Physician 2003;67:1007-14.
[Google Scholar]
|
| 3. |
Gilmore S, Sinclair R. Chronic telogen effluvium is due to a reduction in the variance of anagen duration. Australas J Dermatol 2010;51:163-7.
[Google Scholar]
|
| 4. |
Kligman AM. Pathologic dynamics of human hair loss. I. Telogen effuvium. Arch Dermatol 1961;83:175-98.
[Google Scholar]
|
| 5. |
Harrison S, Sinclair R. Telogen effluvium. Clin Exp Dermatol 2002;27:389-5.
[Google Scholar]
|
| 6. |
Paus R, Olsen EA, Messenger AG. Hair growth disorders. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller As, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. USA; The McGraw-Hill Companies Inc.; 2008. p. 753-77.
th ed. USA; The McGraw-Hill Companies Inc.; 2008. p. 753-77.'>[Google Scholar]
|
| 7. |
Tosti A, Misciali C, Piraccini BM, Peluso AM, Bardazzi F. Drug induced hair loss and hair growth. Drug Saf 1994;10:310-7.
[Google Scholar]
|
| 8. |
Messenger AG, de Berker DA, Sinclair RD. Disorders of Hair. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of Dermatology. 8 th ed. UK: Blackwell Publishing Ltd; 2010. p. 66.27-66.
th ed. UK: Blackwell Publishing Ltd; 2010. p. 66.27-66.'>[Google Scholar]
|
| 9. |
de Berker D. Clinical relevance of hair microscopy in alopecia. Clin Exp Dermatol 2002;27:366-72.
[Google Scholar]
|
| 10. |
Headington JT. Telogen effluvium. New concepts and review. Arch Dermatol 1993;129:356-63.
[Google Scholar]
|
| 11. |
Whiting DA. Chronic telogen effluvium: Increased scalp hair shedding in middle-aged women. J Am Acad Dermatol 1996;35:899-906.
[Google Scholar]
|
| 12. |
Sinclair RD, Banfield CC, DDawber RP. Diffuse hair loss. In: Sinclair RD, Banfield CC, Dawber RP editors. Handbook of diseases of the hair and scalp. UK: Blackwell Science Ltd; 1999. p. 64-74.
[Google Scholar]
|
| 13. |
Nnoruka EN, Obiagboso I, Maduechesi C. Hair loss in children in South-East Nigeria: Common and uncommon cases. Int J Dermatol 2007;46(Suppl 1):18-22.
[Google Scholar]
|
| 14. |
Horenstein VD, Williams LE, Brady AR, Abee CR, Horenstein MG. Age-related diffuse chronic telogen effluvium- type alopecia in female squirrel monkeys (Saimiri boliviensis boliviensis). Comp Med 2005;55:169-74.
[Google Scholar]
|
| 15. |
Kligman AM. The human hair cycle. J Invest Dermatol 1959;33:307-16.
[Google Scholar]
|
| 16. |
Olsen E. Androgenetic alopecia. In: Disorders of hair growth. New York, NY: McGraw-Hill, Inc; 1994. p. 257-83.
[Google Scholar]
|
| 17. |
Shapiro J. Diseases of the hair. In: Raykel R, editor. Conn's current therapy. Philadelphia, Pa: WB Saunders; 1996. p. 739-41.
[Google Scholar]
|
| 18. |
Messenger A. Hair loss. Clin Exp Dermatol 2002;27:357.
[Google Scholar]
|
| 19. |
Dawber RP, Connor BL. Pregnancy, hair loss, and the pill. Br Med J 1971;4:234.
[Google Scholar]
|
| 20. |
Griffiths WA. Diffuse hair loss and oral contraceptives. Br J Dermatol 1973;88:31-6.
[Google Scholar]
|
| 21. |
Strumia R. Dermatologic signs in patients with eating disorders. Am J Clin Dermatol 2005;6:165-73.
[Google Scholar]
|
| 22. |
Barcaui CB, Gonçalves da Silva AM, Sotto MN, Genser B. Stem cell apoptosis in HIV-1 alopecia. J Cutan Pathol 2006;33:667-71.
[Google Scholar]
|
| 23. |
Dawber RPR, Simpson NB, Barth JH. Diffuse alopecia: Endocrine, metabolic and chemical influences on the follicular cycle. In: Dawber RP, editor. Diseases of the Hair and Scalp. Oxford: Blackwell Science; 1997. p. 123-50.
[Google Scholar]
|
| 24. |
Hadshiew IM, Foitzik K, Arck PC, Paus R. Burden of hair loss: Stress and the underestimated psychosocial impact of telogen effluvium and androgenetic alopecia. J Invest Dermatol 2004;123:455-7.
[Google Scholar]
|
| 25. |
Goette DK, Odom RB. Alopecia in crash dieters. JAMA 1976;235:2622-3.
[Google Scholar]
|
| 26. |
Smith AG. Drug induced disorders of hair and nails. Adverse Drug React Bull 1995;173:655-8.
[Google Scholar]
|
| 27. |
Wirth H, Dunsing W, Gloor M. Telogen effluvium following application of selenium disulfide in the guinea pig. Hautarzt 1980;31:502-4.
[Google Scholar]
|
| 28. |
Center for Disease Control and Prevention (CDC). Thallium poisoning from eating contaminated cake--Iraq, 2008. MMWR Morb Mortal Wkly Rep 2008;57:1015-8.
[Google Scholar]
|
| 29. |
Trüeb RM. Is androgenetic alopecia a photo aggravated dermatosis? Dermatology 2003;207:343-8.
[Google Scholar]
|
| 30. |
Braida D, Dubief C, Lang G. Photoageing of hair fiber and photoprotection. Skin Pharmacol 1994;7:73-7.
[Google Scholar]
|
| 31. |
Piérard-Franchimont C, Peérard GE. L'effluvium télogène actinique: Une facette de la chronobiologie humaine. Int J Cosmet Sci 1999;21:15-21.
[Google Scholar]
|
| 32. |
Tosti A, Piraccini BM, van Neste DJ. Telogen effluvium after allergic contact dermatitis of the scalp. Arch Dermatol 2001;137:187-90.
[Google Scholar]
|
| 33. |
de Berker D. Clinical relevance of hair microscopy in alopecia. Clin Exp Dermatol 2002;27:366-72.
[Google Scholar]
|
| 34. |
Rook A. Endocrine influences on hair growth. Br Med J 1965;1:609-14.
[Google Scholar]
|
| 35. |
Church RE. Hypothyroid hair loss. Br J Dermatol 1956;77:661-3.
[Google Scholar]
|
| 36. |
Trost LB, Bergfeld WF, Calogeras E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol 2006;54:824-44.
[Google Scholar]
|
| 37. |
Olsen EA. Iron deficiency and hair loss: The jury is still out. J Am Acad Dermatol 2006;54:903-6.
[Google Scholar]
|
| 38. |
Williams ML, Packman S, Cowan MJ. Alopecia and periorificial dermatitis in biotin-responsive multiple carboxylase deficiency. J Am Acad Dermatol 1983;9:97-103.
[Google Scholar]
|
| 39. |
Chen W, Yang CC, Todorova A, Al Khuzaei S, Chiu HC, Worret WI, et al. Hair loss in elderly women. Eur J Dermatol 2010;20:145-51.
[Google Scholar]
|
| 40. |
Bradfield RB, Bailley MA. Hair root response to protein under nutrition. In: Montagna, W, Dobson RC, editors. Advances in Biology of the Skin. Vol. 9. Hair Growth. Oxford: Pergamon Press; 1968. p. 109-11.
[Google Scholar]
|
| 41. |
Wells G. Skin disorders in relation to malabsorption. Br Med J 1962;2:937-43.
[Google Scholar]
|
| 42. |
Skolnik P, Eaglstein WH, Ziboh VA. Human essential fatty acid deficiency. Arch Dermatol 1977;113:939-41.
[Google Scholar]
|
| 43. |
Stimson WH. Vitamin A intoxication in adults; report of a case with a summary of the literature. N Engl J Med 1961;265:369-73.
[Google Scholar]
|
| 44. |
Starzel TE, Putman CW, Groth CG, Corman JL, Taubman J. Alopecia ascites and incomplete regeneration after 85-95% liver resection. Am J Surg 1975;129:587-8.
[Google Scholar]
|
| 45. |
Scoggins RB, Harlan WR. Cutaneous manifestations of hyperlipidaemia and uraemia. Postgrad Med 1967;41:357-8.
[Google Scholar]
|
| 46. |
Klein AW, Rudolf RI, Leydon JJ. Telogen effluvium as a sign of Hodgkin's disease. Arch Dermatol 1973;108:702-3.
[Google Scholar]
|
| 47. |
de Berker DA, Messenger AG, Sinclair RD. Disorders of hair. In: Burns DA, Breathnach SM, Cox N, Griffiths CE, editors. Rook's textbook of dermatology. London, England: Blackwell Science; 2004. p. 63.31-6.
[Google Scholar]
|
| 48. |
Dawber RP, Simpson NB. Hair and scalp in systemic disease. In: Dawber RP, editor. Diseases of the Hair and Scalp. Oxford: Blackwell Science; 1997. p. 483-527.
[Google Scholar]
|
| 49. |
Kennedy C. Syphilis presenting as hair loss. Br Med J 1976;2:854.
[Google Scholar]
|
| 50. |
Barcaui CB, Gonçalves da Silva AM, Sotto MN, Genser B. Stem cell apoptosis in HIV-1 alopecia. J Cutan Pathol 2006;33:667-71.
[Google Scholar]
|
| 51. |
Gupta AK, Goldfarb MT, Ellis CN, Vorhees JJ. Side-effect profile of acitretin therapy in psoriasis. J Am Acad Dermatol 1989;20:1088-93.
[Google Scholar]
|
| 52. |
Bardelli A, Rebora A. Telogen effluvium and minoxidil. J Am Acad Dermatol 1989;21:572-3.
[Google Scholar]
|
| 53. |
Bleiker TO, Nicolaou N, Traulsen J, Hutchinson PE. 'Atrophic telogen effluvium' from cytotoxic drugs and a randomized controlled trial to investigate the possible protective effect of pretreatment with a topical vitamin D analogue in humans. Br J Dermatol 2005;153:103-12.
[Google Scholar]
|
| 54. |
Pearce SH. Spontaneous reporting of adverse reactions to carbimazole and propylthiouracil in the UK. Clin Endocrinol (Oxf) 2004;61:589-94.
[Google Scholar]
|
| 55. |
Mounsey AL, Reed SW. Diagnosing and treating hair loss. Am Fam Physician 2009; 80:356-62.
[Google Scholar]
|
| 56. |
Tuccori M, Pisani C, Bachini L, Pardini M, Mantarro S, Antonioli L, et al. Telogen Effluvium following Bivalent Human Papilloma virus Vaccine Administration: A Report of Two Cases. Dermatology 2012;224:212-4.
[Google Scholar]
|
| 57. |
Katz KA, Cotsarelis G, Gupta R, Seykora JT. Telogen effluvium associated with the dopamine agonist pramipexole in a 55-year-old woman with Parkinson's disease. J Am Acad Dermatol 2006;55(5 Suppl):S103-4.
[Google Scholar]
|
| 58. |
Patrizi A, Savoia F, Negosanti F, Posar A, Santucci M, Neri I. Telogen effluvium caused by magnesium valproate and lamotrigine. Acta Derm Venereol 2005;85:77-8.
[Google Scholar]
|
| 59. |
Kaimal S, Thappa DM. Diet in dermatology: Revisited. Indian J Dermatol Venereol Leprol 2010;76:103-15.
[Google Scholar]
|
| 60. |
Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol 2002;27:396-404.
[Google Scholar]
|
| 61. |
Van Neste MD. Assessment of hair loss: Clinical relevance of hair growth evaluation methods. Clin Exp Dermatol 2002;27:358-65.
[Google Scholar]
|
| 62. |
Kullavanijaya P, Gritiyarangsan P, Bisalbutra P, Kulthanan R, Cardin CW. Absence of effects of dimethicone-and non-dimethicone shampoos on daily hair loss rates. J Soc Cosmet Chem 1992;43:195-206 .
[Google Scholar]
|
| 63. |
Guarrera M, Semino MT, Rebora A. Quantitating hair loss in women: A critical approach. Dermatology 1997;194:12-6.
[Google Scholar]
|
| 64. |
Piérard GE, Piérard-Franchimont C, Marks R, Elsner P, for the EEMCO group (European Expert Group on Efficacy Measurement of Cosmetics and Other Topical Products). EEMCO guidance for the assessment of hair shedding and alopecia. Skin Pharmacol Physiol 2004;17:98-110.
[Google Scholar]
|
| 65. |
Shapiro J, Wiseman M, Lui H. Practical management of hair loss. Can Fam Physician 2000;46:1469-77.
[Google Scholar]
|
| 66. |
Hoffmann R. TrichoScan. Combining epiluminescence microscopy with digital image analysis for the measurement of hair growth in vivo. Eur J Dermatol 2001;11:362-8.
[Google Scholar]
|
| 67. |
Rushton DH, De Brouwer B, De Coster W, Van Neste D. Comparative evaluation of scalp hair by phototrichogram and unit area trichogram analysis within the same subjects. Acta Derm Venereol (Stockh) 1993;73:150-3.
[Google Scholar]
|
| 68. |
Blume U, Ferracin I, Verschoore M, Czernielewski JM, Schaefer H. Physiology of the vellus hair follicle: Hair growth and sebum excretion. Br J Dermatol 1991;124:21-8.
[Google Scholar]
|
| 69. |
Van Neste DJ, Rushton DH. Hair problems in women. Clin Dermatol 1997;15:113-25.
[Google Scholar]
|
| 70. |
Sinclair R, Jolley D, Mallari R, Magee J. The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair in loss Women. J Am Acad Dermatol 2004;51:189-99.
[Google Scholar]
|
| 71. |
Eudy G, Solomon AR. The histopathology of noncicatricial alopecia. Semin Cutan Med Surg 2006;25:35-40.
[Google Scholar]
|
| 72. |
Frieden L, Price V. Androgenetic alopecia. In: Thiers B, Dobson R, editors. Pathogenesis of skin disease. New York: Churchill Livingstone; 1986. p. 41-55.
[Google Scholar]
|
| 73. |
Whiting DA. Update on chronic telogen effluvium. Exp Dermatol 1999;8:305-6.
[Google Scholar]
|
| 74. |
Miteva M, Tosti A. Dermatoscopy of hair shaft disorders. J Am Acad Dermatol 2013;68:473-81.
[Google Scholar]
|
| 75. |
Ross EK, Vincenzi C, Tosti A. Videodermatoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol 2006;55:799-806.
[Google Scholar]
|
| 76. |
Rakowska A, Slowinska M, Kowalska-Oledzka E, Olszewska M, Rudnicka L. Dermatoscopy in female androgenic alopecia: Method standardization and diagnostic criteria. Int J Trichol 2009;1:123-30 .
[Google Scholar]
|
| 77. |
Sinclair R. There is no clear association between low serum ferritin and chronic diffuse telogen hair loss. Br J Dermatol 2002;147:982-4.
[Google Scholar]
|
| 78. |
Chen W, Yang CC, Todorova A, Al Khuzaei S, Chiu HC, Worret WI, et al. Hair loss in elderly women. Eur J Dermatol 2010;20:145-51.
[Google Scholar]
|
| 79. |
Wiedemeyeer K, Schill WB, LOser C . Diseases on hair follicles leading to hair loss part I: nonscarring alopecias. Skinmed 2004;3:209-14.
[Google Scholar]
|
| 80. |
Sinclair R. Diffuse hair loss. Int J Dermatol 1999;38(Suppl 1): 8-18.
[Google Scholar]
|
| 81. |
Rushton DH, Ramsey ID, James KC, Norris MJ, Gilkes JJ. Biochemical and trichological characterization of diffuse alopecia in women. Br J Dermatol 1990;123:187-97.
[Google Scholar]
|
| 82. |
Ludwig E. Classification of the types of androgenetic alopecia (common baldness) arising in the female sex. Br J Dermatol 1977;97:247-54.
[Google Scholar]
|
| 83. |
Whiting DA. Scalp biopsy as a diagnostic and prognostic tool in androgenetic alopecia. Dermatol Ther 1998;8:24-33.
[Google Scholar]
|
| 84. |
Whiting DA. Chronic telogen effluvium. Dermatol Clin 1996;14:723-31.
[Google Scholar]
|
| 85. |
Sinclair R. Chronic telogen effluvium: A study of 5 patients over 7 years. J Am Acad Dermatol 2005;52:12-6.
[Google Scholar]
|
| 86. |
Courtois M, Loussouarn G, Hourseau C, Grollier JF. Aging and hair cycles. Br J Dermatol 1995;132:86-93.
[Google Scholar]
|
| 87. |
Baldari M, Guarrera M, Rebora A. Thyroid peroxidase antibodies in patients with telogen effluvium. J Eur Acad Dermatol Venereol 2010;24:980-2.
[Google Scholar]
|
| 88. |
Fiedler VC, Gray AC. Diffuse alopecia: Telogen hair loss. In: Olsen EA, editor. Disorders of hair growth: Diagnosis and treatment. 2 nd ed. New York: McGraw-Hill; 2003. p. 303-20.
[Google Scholar]
|
| 89. |
Schrier SL. Causes and diagnosis of anemia due to iron deficiency. Available from: http://www.UpToDate.com. [Last accessed on 2005 Apr 18, last updated on 2003 Nov 6].
[Google Scholar]
|
| 90. |
Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med 2005;352:1011-23.
[Google Scholar]
|
| 91. |
Weismann K. Zinc metabolism and the skin. In: Rook AS, Savin JA, editos. Recent Advances in Dermatology. 5 ed. Inburgh: Churchill Livingstone; 1980. p. 109-29.
[Google Scholar]
|
| 92. |
Bradfield RB, Bailley MA. Hair root response to protein undernutrition. In: Montagna W, Dobson RC, editors. Advances in Biology of the Skin. Vol. 9. Hair Growth. Oxford: Pergamon Press; 1968. p. 109-11.
[Google Scholar]
|
| 93. |
Hordinsky MK. Medical treatment of noncicatricial alopecia. Semin Cutan Med Surg 2006;25:51-5.
[Google Scholar]
|
| 94. |
Brodin MB. Drug-related alopecia. Dermatol Clin 1987;5:571-9.
[Google Scholar]
|
| 95. |
Feidler VC Hafeez A. Diffuse alopecia. telogen hair loss. In: Olsen EA, editor. Disorders of Hair growth, diagnosis and treatment. New York: McGraw; 1994. p. 241-55.
[Google Scholar]
|
| 96. |
Cash TF. The psychology of hair loss and its implications for patient care. Clin Dermatol 2001;19:161-6.
[Google Scholar]
|
| 97. |
Bosse KA, Gieler U. Seelische Faktorenbei Haustkrankheiten: Beitra¨ gezurpsychosomatischen Dermatologie. Bern: Verlag Hans Huber; 1987.
[Google Scholar]
|
| 98. |
Botchkarev VA. Stress and the hair follicle: Exploring the connections. Am J Pathol 2003;162:709-12.
[Google Scholar]
|
| 99. |
Paus R. Stress, hair growth control and the neuro-endocrine immune connection. Allergol J 2000;9:611-20.
[Google Scholar]
|
| 100. |
Arck PC, Handjiski B, Kuhlmei A, Peters EM, Knackstedt M, Peter A, et al. Mast cell deficient and neurokinin-1 receptor knockout mice are protected from stress-induced hair growth inhibition. J Mol Med (Berl) 2005;83:386-96.
[Google Scholar]
|
| 101. |
Peters EM, Arck PC, Paus R. Hair growth inhibition by psychoemotional stress: A mouse model for neural mechanisms in hair growth control. Exp Dermatol 2006;15:1-13.
[Google Scholar]
|
| 102. |
Arck PC, Handjiski B, Hagen E, Joachim R, Klapp BF, Paus R. Indications for a''brain-hair follicle axis (BHA)'':Inhibition of keratinocyte proliferation and up-regulation of keratinocyte apoptosis in telogen hair follicles by stress and substance P. FASEB J 2001;15:2536-8.
[Google Scholar]
|
| 103. |
Arck PC, Handjiski B, Peters EM, Hagen E, Klapp BF, Paus R. Topical minoxidil counteracts stress-induced hair growth inhibition in mice. Exp Dermatol 2003;12:580-90.
[Google Scholar]
|
| 104. |
Arck PC, Handjiski B, Peters EM, Peter AS, Hagen E, Fischer A, et al. Stress inhibits hair growth in mice by induction of premature catagen development and deleterious perifollicular inflammatory events via neuropeptide substance P-dependent pathways. Am J Pathol 2003;162:803-14.
[Google Scholar]
|
| 105. |
Aoki E, Shibasaki T, Kawana S. Intermittent foot shock stress prolongs the telogen stage in the hair cycle of mice. Exp Dermatol 2003;12:371-7.
[Google Scholar]
|
| 106. |
Ito N, Ito T, Kromminga A, Bettermann A, Takigawa M, Kees F, et al. Human hair follicles display a functional equivalent of the hypothalamic-pituitary-adrenal axis and synthesize cortisol. FASEB J 2005;19:1332-4.
[Google Scholar]
|
| 107. |
Peters EM, Handjiski B, Kuhlmei A, Hagen E, Bielas H, Braun A, et al. Neurogenic inflammation in stress induced termination of murine hair growth is promoted by nerve growth factor. Am J Pathol 2004;165:259-71.
[Google Scholar]
|
| 108. |
Rupniak NM, Kramer MS. Discovery of the antidepressant and anti-emetic efficacy of substance P receptor (NK1) antagonists. Trends Pharmacol Sci 1999;20:485-90.
[Google Scholar]
|
| 109. |
Alvaro G, Di Fabio R. Neurokinin 1 receptor antagonists--current prospects. Curr Opin Drug Discov Devel 2007;10:613-21.
[Google Scholar]
|
| 110. |
Slominski A, Wortsman J, Luger T, Paus R, Solomon S. Corticotropin releasing hormone and proopiomelanocortin involvement in the cutaneous response to stress. Physiol Rev 2000;80:979-1020.
[Google Scholar]
|
| 111. |
McMichael A. Approach to office visits for hair loss in women. Cutis 2011;87:8-9.
[Google Scholar]
|
| 112. |
Chartier MB, Hoss DM, Grant-Kels JM. Approach to the adult female patient with diffuse non scarring alopecia. J Am Acad Dermatol 2002;47:809-18;quiz818-20.
[Google Scholar]
|
| 113. |
Kivanç-Altunay I, Savaº C, Gökdemir G, Köºlü A, Ayaydin EB. The presence of trichodynia in patients with telogen effluvium and androgenetic alopecia. Int J Dermatol 2003;42:691-3.
[Google Scholar]
|
| 114. |
Baldari M, Montinari M, Guarrera M, Rebora A. Trichodynia is a distinguishing symptom of telogen effluvium J Eur Acad Dermatol Venereol 2009;23:702-38.
[Google Scholar]
|
| 115. |
Harth W, Hermes B, Niemeier V, Gieler U. Clinical pictures and classification of somatoform disorders in dermatology. Eur J Dermatol 2006;16:607-14.
[Google Scholar]
|
| 116. |
Harth W, Hermes B, Seikowski K, Gieler U. Nihilodermia in psychodermatology. Hautarzt 2007;58:427-34.
[Google Scholar]
|
| 117. |
Adamson JW. Iron deficiency and other hypoproliferative anemias. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 16 th ed. New York: McGraw-Hill; 2005. p. 586-92.
th ed. New York: McGraw-Hill; 2005. p. 586-92.'>[Google Scholar]
|
| 118. |
Park J, Song KH, Nam KH. Circumscribed alopecia areata incognita. Australas J Dermatol 2013;54:52-4.
[Google Scholar]
|
| 119. |
Kantor J, Kessler LJ, Brooks DG, Cotsarelis G. Decreased serum ferritin is associated with alopecia in women. J Invest Dermatol 2003;121:985-8.
[Google Scholar]
|
| 120. |
Umbreit J. Iron deficiency: A concise review. Am J Hematol 2005;78:225-31.
[Google Scholar]
|
| 121. |
Schrier SL. Treatment of anemia due to iron deficiency. Available from: http://www.UpToDate.com. [Last accessed on 2005 Apr 18, last updated on 2001 Feb 27].
[Google Scholar]
|
| 122. |
Goddard AF, McIntyre AS, Scott BB. Guidelines for the management of iron deficiency anaemia. British Society of Gastroenterology. Gut 2000;46:1-5.
[Google Scholar]
|
| 123. |
Bottomley SS. Secondary iron overload disorders. Semin Hematol 1998;35:77-86.
[Google Scholar]
|
| 124. |
Esfandiari A, Kelly AP. The effects of tea polyphenolic compounds on hair loss among rodents. J Natl Med Assoc 2005;97:1165-9.
[Google Scholar]
|
| 125. |
Tosti A, Comacho-Martinez F, Dawber R. Management of androgenetic alopecia. J Eur Acad Dermatol Venereol 1999;12:205-14.
[Google Scholar]
|
| 126. |
Davis MG, Thomas JH, van de Velde S, Boissy Y, Dawson TL Jr, Iveson R, et al. A novel cosmetic approach to treat thinning hair. Br J Dermatol 2011;165(Suppl 3):24-30.
[Google Scholar]
|
| 127. |
Paus R, Cotsarelis G. The biology of hair follicles. N Engl J Med 1999 12;341:491-7.
[Google Scholar]
|
| 128. |
Buhl AE. Minoxidil's action in hair follicles. J Invest Dermatol 1989;92:315-20.
[Google Scholar]
|
Fulltext Views
37,585
PDF downloads
6,278





