Translate this page into:
2. Pedunculated lesion over lower back
Correspondence Address:
S Chidambara Murthy
Departments of Dermatology and Venereology, S. N. Medical College and HSK Hospital and Research Centre, Bagalkot - 587 102
India
| How to cite this article: Chidambara Murthy S, Udagani M M. 2. Pedunculated lesion over lower back. Indian J Dermatol Venereol Leprol 2004;70:325-327 |
 |
 |
 |
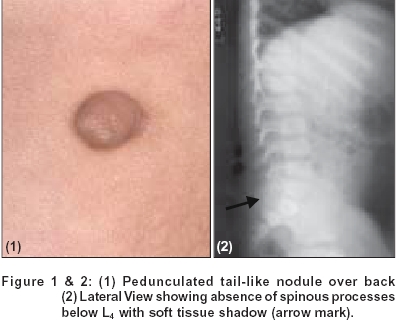 |
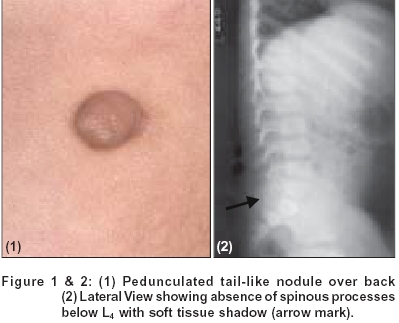
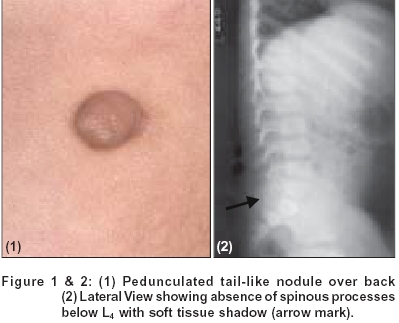
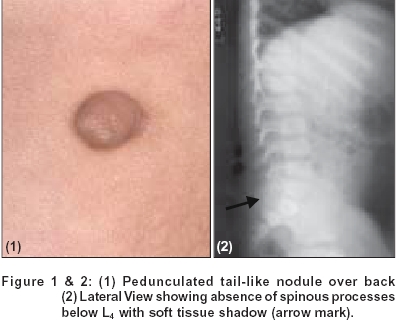
A seven year boy presented with asymptomatic pedunculated lesion over the lower back since birth. He had loss of sensation with recurrent ulcers over the left leg and foot for the last three years. He also had urinary and fecal incontinence. There was no history of hypopigmented patches, spinal injury, drug intake, diabetes or tuberculosis. Family history was unremarkable. Clinical examination revealed a pedunculated nodule overlying L4-5 region [Figure - 1], with a soft swelling underneath it, along the left paravertebral column. Cough impulse was present. A lateral X-ray of the spine is seen in [Figure - 2].
What is your diagnosis?
Answer to Quiz No. 2
Diagnosis: Spinal dysraphism with tail-like projection
DISCUSSION
The patient also had three trophic ulcers over the sole of left foot with multiple atrophic scars over left leg. Nervous system examination showed loss of sensation for pain, touch and temperature below L1. Motor system examination showed mild wasting of muscles of left thigh and leg. Knee and ankle jerks were diminished on left side. Anal sphincter was lax. Routine hematological and urine examinations were normal. Blood VDRL was non reactive. Serology for HIV 1 and 2 was negative. Blood glucose, liver function tests and renal parameters were normal. X-ray L-S spine showed spina bifida below L4. X-ray left foot showed partial resorption of 3rd, 4th and 5th phalanges. Ultrasound abdomen was normal. MRI showed tethered cord with myelomeningocele.
Spinal dysraphism refers to incomplete fusion or malformations of structures in the dorsal midline of the back, particularly congenital abnormalities of the vertebral column and the spinal cord.[1] The term therefore includes spina bifida and other abnormalities such as those in which cutaneous ectoderm is carried deeply, causing dermoid cysts or dermal sinuses to form.[2] A polygenic mechanism including genetic factors is implicated as causative.[3] High risk cutaneous markers for spinal dysraphism include atypical dimples, hemangiomas, upraised lesions (i.e. masses, tails and hairy patches) and multiple cutaneous stigmata.[4] Occult spinal dysraphism may occur in 20% of all individuals of which only a small percentage will have a significant associated neurological defect.[3] Occult spinal dysraphism is associated with cutaneous signs in more than 50% of instances.[1]
The age of onset of neurologic symptoms in occult spinal dysraphism ranges from birth to 76 years, the average being three years.[1] Myelomeningocele is the most serious form of spina bifida, while occulta the least. Lesions preventing the ascent of the cord which occurs during normal growth, can lead to undue traction on the lower end of the cord and cauda equina with resultant neuro-trophic changes.[2] Urinary or fecal incontinence, recurrent urinary infections, muscle atrophy, foot deformities, weakness, pain or decreased sensation may eventually develop. Magnetic resonance imaging (MRI) is the best investigational tool[5] although X-ray, ultrasound can be used for screening. Early detection and surgical intervention can prevent the disabling irreversible neurological deficits.
| 1. |
Tavafoghi V, Ghandchi A, Hambrick GW Jr, Udverhelyi GB. Cutaneous signs of spinal dysraphism. Report of a patient with a tail like lipoma and review of 200 cases in the literature. Arch Dermatol 1978;114:573-7.
[Google Scholar]
|
| 2. |
Archer CB. The skin and the nervous System. In: Champion RH, Burton JL, Burns DA, Breathnach sm, editors. Text book of Dermatology 6th Ed. Oxford: Blackwell Science Ltd.; 1998. p. 2773-83.
[Google Scholar]
|
| 3. |
Atherton DJ. Naevi and other developmental defects. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Text book of Dermatology 6th Ed. Oxford: Blackwell Science Ltd.; 1998. p. 519-616.
[Google Scholar]
|
| 4. |
Kriss VM, Desai NS. Occult spinal dysraphism in neonates: Assessment of high-risk cutaneous stigmata on sonography. Am J Roentgenol 1998;171:1687-92.
[Google Scholar]
|
| 5. |
McAtee-Smith J, Hebert AA, Rapini RP, Goldberg NS. Skin lesions of the spinal axis and spinal dysraphism. Fifteen cases and a review of the literature. Arch Pediatr Adolesc Med 1994;148:740-8.
[Google Scholar]
|
Fulltext Views
4,891
PDF downloads
2,263





