Translate this page into:
Unilateral linear punctate palmoplantar keratoderma
Correspondence Address:
Krishna Deb Barman
Department of Dermatology and Venereology, Maulana Azad Medical College and Associated Hospital, New Delhi - 110 002
India
| How to cite this article: Sharma S, Barman KD, Garg VK, Jain S. Unilateral linear punctate palmoplantar keratoderma. Indian J Dermatol Venereol Leprol 2012;78:85-88 |
Abstract
Punctate palmoplantar keratoderma (Brauer-Buschke-Fischer syndrome) is a rare entity. Among punctate keratoderma, the linear presentation is much rarer, and exact incidence is not known. Unilateral linear punctate palmoplantar keratoderma is not yet reported in the literature. Here we report a case 12-year-old child presented with asymptomatic linear punctate plaque on the left sole and hand; histology revealed hyperkeratotic epidermis without columns of parakeratosis or cornoid lamella.Introduction
Palmoplantar keratodermas are heterogeneous group of disorders characterized by abnormal keratinization of palmar and plantar skin. [1] Among which punctate palmoplantar keratoderma (PPPK) is much rarer with an estimated prevalence rate of 1.17/100,000. It is usually manifested bilaterally as asymptomatic, tiny, hyperkeratotic punctate papules/plaque on the palmoplantar surface. [2] The exact etiology of this disorder is not known, but a dual influence of genetic and environmental factors may trigger the disease. [2] Here, we report a case of unilateral linear PPPK for the first time.
Case Report
A 12-year-old male presented with asymptomatic linear thickening and yellowish discoloration of left sole and left palm since 7 years and 5 years, respectively. Lesions first appeared on the left heel as punctate small plaques that gradually extend in linear fashion up to the third and fourth toe over a period of 7 years. Two years later, similar kind of lesions appeared on the left hypo-thenar eminence which slowly progressed and extend to the base of left little finger. There were no similar lesions on any other part of the body, and the lesions were asymptomatic throughout the course of the disease.
Family members had no similar complaints, no history suggestive of any systemic involvement, prolonged drug intake, chronic weight loss, drug or food allergy, recurrent rhinitis, itching, and dry skin.
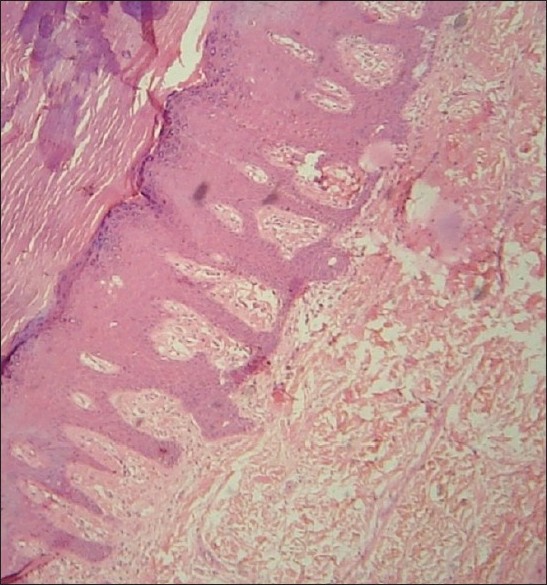
Clinical examination revealed a yellow-colored thick linear punctate plaque on the left sole extending from the central part of the heel up to the third and fourth toe with variable width ranging from 1 to 5 cm. The surface of the plaque had multiple punctums; on palpation lesion was firm, rough, and non-tender [Figure - 1]. Thickening and yellowish discoloration was more over pressure areas. Similar type of plaques with punctums ranging from 2 × 3 cm to 1 × 2 cm were present on the left palm extending from hypothenar eminence to the base of little finger [Figure - 1]. Right palm and right sole were normal.
Apart from these cutaneous clinical findings, rest of dermatological and systemic examinations were normal.
 |
| Figure 1: Localized plaques with punctums were present on the palmar surface of the left hand along with yellowish-colored thick linear punctate plaque on the left sole |
With these clinical findings, we had made the probable diagnosis of linear PPPK.
Patient routine investigation, stool for occult blood, chest X-ray, X-ray of left hand and feet, and ECG were within normal limit.
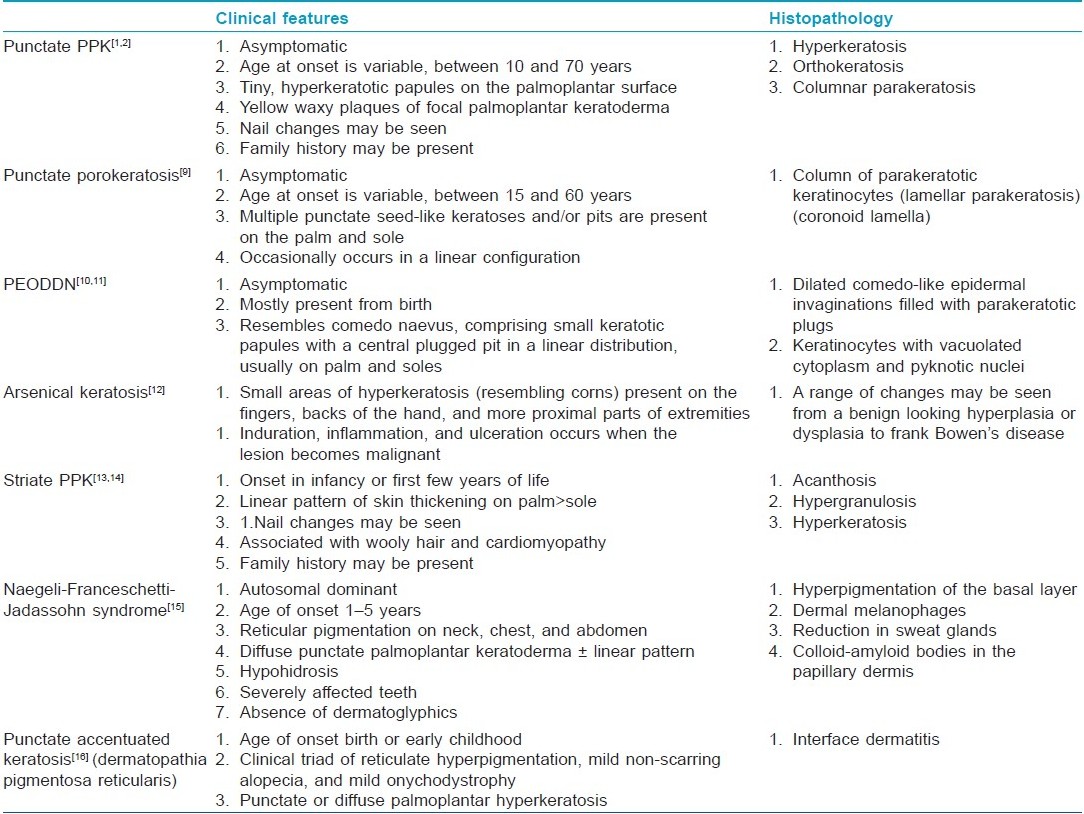
A 4-mm punch biopsy specimen from the left heel was sent to the department of pathology Maulana Azad Medical College, New Delhi, for histopathological examination, which revealed hyperkeratotic epidermis without any columns of parakeratosis or cornoid lamella [Figure - 2]. With these clinical findings and histopathological features, the final diagnosis was made linear PPPK.
 |
| Figure 2: Histopathologic examination revealed hyperkeratotic epidermis without columns of parakeratosis or coronoid lamella (H and E, ×10) |
Discussion
Palmoplantar keratodermas are heterogeneous group of disorders characterized by abnormal keratinization of palmar and plantar skin. [1] The palmoplantar keratodermas (PPKs) can initially be divided based on whether they are inherited or acquired. The inherited PPKs are further classified into three distinct types based on clinical pattern of epidermal involvement. The first is diffuse PPK, the second is focal PPK, and the third is punctate keratoderma. [3]
Incidence of various etiological factors causing hyperkeratosis of palms and soles in Indian patients is not known. Palmoplantar keratoderma is found to be more common in males (64.63%), with highest incidence in the age group of 11-20 years (32.92%). Occupation-wise manual workers such as laborers, farmers, and mechanical workers contributed to 48.16%, students 33.15%, and housewives 18.69%. [4]
Exacerbation of hyperkeratosis was seen in winter (41.46%), summer (20.73%), and autumn (19.51%). [4]
The exact etiology of this disorder is not known, but a dual influence of genetic and environmental factors may trigger the disease. [2] It has been described in few large autosomal dominant pedigrees. A genomewide scan was performed on an extended autosomal dominant pedigree, and linkage to chromosome 15q22-q24 was identified. [5] Martinez et al. [5] reported two new families with the same phenotype, which confirmed the mapping of the locus for punctate PPK to a 9.98-cm interval, flanked by markers D15S534 and D15S818.
Clinically, PPPK present as an asymptomatic, tiny, hyperkeratotic punctate papules on the palmoplantar surface. In PPPK, involvement is usually bilateral with no case unilateral linear PPPK reported in the literature. [2] Nail abnormalities in the form of longitudinal ridging, onychorrhexis, onychoschizia, trachyonychia, and notching can be seen. [6] Individual with PPPK lack associated systemic features; however, spastic paralysis, ankylosing spondylitis, facial sebaceous hyperplasia, and atopy have been reported. [2] An association with gastrointestinal and pulmonary malignancy is possible. [2],[7],[8] Because the affected individuals appear to be at increased risk of developing malignant conditions, a regular follow-up with thorough history taking and clinical examination is mandatory in cases of hereditary punctate PPK. [8]
Histopathological features of PPPK are hyperkeratotic epidermis without any columns of parakeratosis or elastorrhexis. Electron microscopy shows enlarged nucleoli with abundant tonofilaments in the basal cells and keratohyalin-like granules confined to the upper part of the stratum spinosum. [2]
In this case, we also find the similar histological findings. Due to non-availability, we cannot perform the electron microscopic examination of this case.
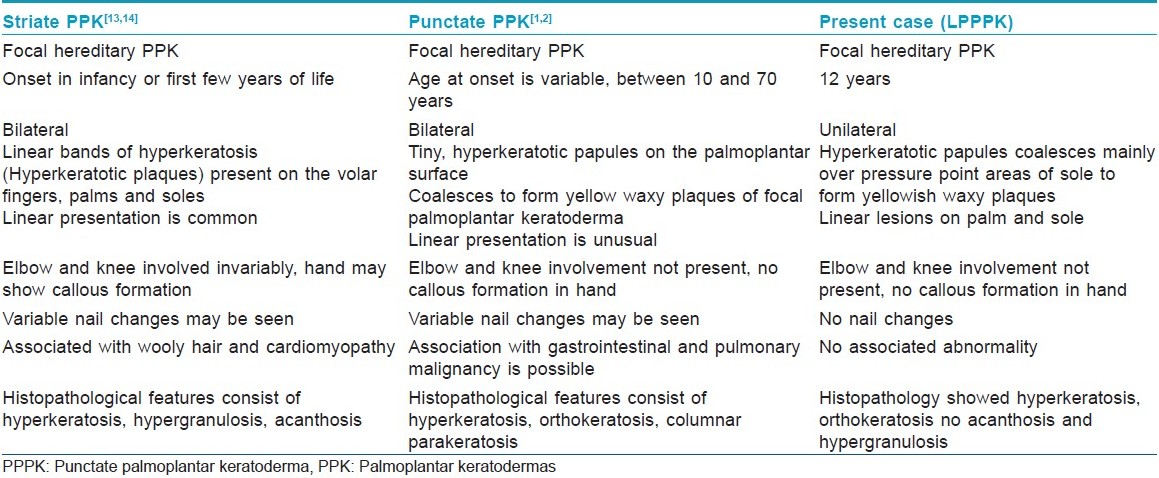
Our patient is also presented with an asymptomatic, tiny, hyperkeratotic punctate papules on the palmoplantar surface with unilateral left sole and left palm involvement without any associated diseases and we had made the differential diagnosis of linear PPPK, [1,2] linear punctate porokeratosis, [9] porokeratotic eccrine ostial and dermal duct naevus (PEODDN), [10],[11] arsenical keratosis, [12] striate PPK, [13],[14] Naegeli-Franceschetti-Jadassohn syndrome, [15] and punctate accentuated keratosis. [16]
Above differential had been ruled out by their classical clinical presentation and histopathological features [Table - 1] and [Table - 2]. [1],[2],[9],[10],[11],[12],[13],[14],[15],[16]
Treatment of keratodermas is generally symptomatic like saltwater soaks, paring, topical keratolytics to specific therapies such as systemic retinoids, psoralens and ultraviolet A (PUVA), and re-PUVA. [2],[8] When specific therapy does not works, then patient can be considered for reconstructive surgery with total excision of the hyperkeratotic skin followed by grafting. [2]
Lienemann et al. reported 95% improvement following 2-week course of intravenous 5-FU at 250 mg/m 2/day. [17]
| 1. |
Erkek E, Erdogan S, Tuncez F, Kurtipek GS, Bagci Y, Ozoguz P, et al. Type I hereditary punctate keratoderma associated with widespread lentigo simplex and successfully treated with low-dose oral acitretin. Arch Dermatol 2006;142:48.
[Google Scholar]
|
| 2. |
Oztas P, Alli N, Polat M, Dagdelen S, Ustün H, Artüz F, et al. Punctate palmoplantar keratoderma (Brauer-Buschke-Fischer syndrome). Am J Clin Dermatol 2007;8:113-6.
[Google Scholar]
|
| 3. |
Lee RA, Yassaee M, Bowe WP, William DJ. Keratosis palmaris et plantaris. e-Medicine. Available from: http://emedicine.medscape.com. [Last accessed on 2008 Jul 28].
[Google Scholar]
|
| 4. |
Mahajan PM, Gharpuray MB, Kulkarni V. Clinical and histopathological study of palmoplantar keratoderma. Indian J Dermatol Venereol Leprol 1994;60:258-61.
[Google Scholar]
|
| 5. |
Martinez-Mir A, Zlotogorski A, Londono D, Gordon D, Grunn A, Uribe E, et al. Identification of a locus for type 1 punctate palmoplantar keratoderma on chromosome 15q22-q24. J Med Genet 2003;40:872-8.
[Google Scholar]
|
| 6. |
Gupta R, Mehta S, Pandhi D, Singal A. Hereditary Punctate Palmoplantar Keratoderma (PPK) (Brauer-Buschke-Fischer Syndrome). J Dermatol 2004;31:398-402.
[Google Scholar]
|
| 7. |
Stevens HP, Kelsell DP, Leigh IM, Ostlere LS, MacDermot KD, Rustin MH. Punctate palmoplantar keratoderma and malignancy in a four-generation family. Br J Dermatol 1996;134:720-6.
[Google Scholar]
|
| 8. |
Nawaf AM, Joshi A, Osama NE. Punctate palmoplantar keratoderma (Buschke-Fischer-Brauer disease) with psoriasis: A rare association showing excellent response to acitretin. J Drugs Dermatol 2005;4:627-34.
[Google Scholar]
|
| 9. |
Rahbari H, Cordero AA, Mehregan AH. Punctate porokeratosis: A clinical variant of porokeratosis of Mibelli. J Cutan Pathol 1977;4:338-41.
[Google Scholar]
|
| 10. |
Valkas R, Abajo P, Fraga J, Aragues M, Garcia-Diez A. Porokeratotic eccrine ostial and dermal duct nevus of late onset: More frequent than previously suggested? Dermatology 1996;193:138-40.
[Google Scholar]
|
| 11. |
Jiminez J, Gomez I, Gonzalez C, Lopez J, Poblet E. Porokeratotic eccrine ostial and dermal duct nevus. Br J Dermatol 1995;132:490-1.
[Google Scholar]
|
| 12. |
Rahman MM, Chowdury UK, Mukherjee SC. Chronic arsenic toxicity in Bangladesh and West Bengal: A review and commentary. J Toxicol Clin Toxicol 2001;39:683-700.
[Google Scholar]
|
| 13. |
Whittock NV, Ashton GH, Dopping PJ. Striate palmoplantar keratoderma resulting from desmoplakin haploinsufficiency. J Invest Dermatol 1999;113:940-6.
[Google Scholar]
|
| 14. |
Kelsell DP, Leigh IM. Inherited keratodermas of palms and soles. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York NY: McGraw-Hill; 2007. p. 427-9.
th ed. New York NY: McGraw-Hill; 2007. p. 427-9.'>[Google Scholar]
|
| 15. |
Itin PH, Lautenschlager S, Meyer R, Mevorah B, Rufli T. Natural history of the Naegeli-Franceschetti-Jadassohn syndrome and further delineation of its clinical manifestations. J Am Acad Dermatol 1993;28:942-50.
[Google Scholar]
|
| 16. |
Rustad OJ, Vance JC. Punctate keratoses of the palms and soles and keratotic pits of the palmar creases. J Am Acad Dermatol 1990;22:468-76.
[Google Scholar]
|
| 17. |
Lienemann AO, Colucci VJ, Jones MS, Trauscht JM. Treatment of palmoplantar keratoderma with continuous infusion 5-fluorouracil. Cutis 2004;73:303-8.
[Google Scholar]
|
Fulltext Views
4,747
PDF downloads
2,376





