Translate this page into:
Can highly active antiretroviral therapy unmask leprosy? A case of type 1 lepra reaction in a HIV-seropositive patient
Correspondence Address:
G Raghurama Rao
Surya Skin Care and Research Center, # 15-1-2, Gopal Sadan, Naoroji Road, Maharanipeta, Visakhapatnam - 530 002, Andhra Pradesh
India
| How to cite this article: Rao G R, Amareswar A, Sandhya S. Can highly active antiretroviral therapy unmask leprosy? A case of type 1 lepra reaction in a HIV-seropositive patient. Indian J Dermatol Venereol Leprol 2012;78:101-103 |
Sir,
The natural course of leprosy coinfected with HIV is not clearly understood. Contrary to earlier speculations, to date, HIV infection has not been reported to increase susceptibility to leprosy or to have a significant effect on the pathogenesis. In contrast, initiation of Highly Active Antiretroviral Therapy (HAART) has been reported to be associated with activation of subclinical Mycobacterium leprae infection and exacerbation of existing leprosy lesions. [1] Majority of the reported cases in the literature have been borderline tuberculoid (BT) leprosy, with type 1 reaction as a manifestation of IRIS. [2] We have come across one case of type 1 lepra reaction in a HIV-seropositive individual as an exacerbation of previously unnoticed leprosy after 18 months of HAART.
A 26-year-old HIV-seropositive woman who has been on HAART (AZT+3TC+NVP) for the last 18 months presented with painless, erythematous, indurated plaque of 7 x 3 cm and a satellite lesion of 2 x 2 cm over the left cheek since ten days [Figure - 1]. All sensations were impaired over the lesions. The left greater auricular nerve and other peripheral nerves were not thickened and non-tender. There were no regional lymphadenopathy and no hypopigmented anesthetic patches elsewhere over the body. She observed two asymptomatic vague hypopigmented patches over her left cheek four months ago for which she did not seek any medical advice. Since ten days, both the patches suddenly became inflamed, edematous, and elevated, which attracted her attention for medical advice. Her CD4+ cell count was 340 and her initial CD4+ cell count was 154 at the time of starting HAART 18 months ago. HIV RNA PCR (RNA Viral Load) was not done. A 3-mm punch biopsy from the skin lesion revealed nodular tuberculoid granulomatous inflammation centered around neurovascular bundles involving most of the dermis. The granuloma consists of lymphocytes, numerous epitheloid cells, occasional plasma cells, and several foreign body and Langhans giant cells. The dermoepidermal junction was infiltrated by the infiltrate in several foci. Presence of dense infiltrate of lymphocytes with small amount of lymphocytic nuclear dust was suggestive of type 1 reaction [Figure - 2]. Fite-Faraco staining revealed no bacilli. A diagnosis of BT leprosy in type 1 reaction was made on the basis of clinical and histopathological features. The patient was asked to continue HAART and in addition anti-leprosy treatment (dapsone 100 mg PO daily, clofazimine 100 mg PO daily, and rifampicin 600 mg PO once monthly) was started. As there were no signs of neuritis, systemic steroids were not given. After 6 months of therapy, complete regression of the lesions was observed and the treatment was continued for another 6 months and there were no new lesions during the follow-up period of one year.
 |
| Figure 1: Borderline tuberculoid leprosy in type 1 reaction |
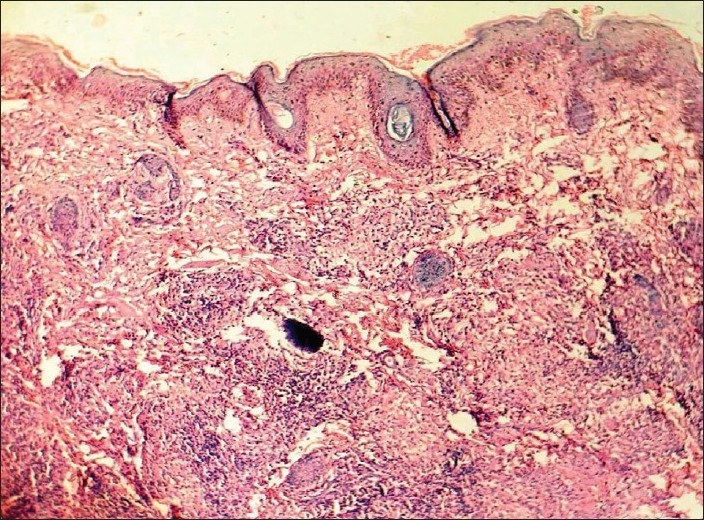 |
| Figure 2: Nodular tuberculoid granuloma with small amount of lymphocytic nuclear dust (H and E, ×10) |
The relation between leprosy and HIV infection is an enigma and the interactions between these infections have not been elaborately studied. [3] Most of the reports of HIV and leprosy coinfections are associated with BT leprosy, usually presenting as type 1 reaction, as a component of IRIS. [2] But in this case, a question arises whether the type 1 reaction is a part of IRIS, or a subclinical leprosy that has become overt due to immune restoration by HAART. Our case does not conform to the known pattern of IRIS, [2],[4] as the clinical lesions exacerbated after 18 months of starting HAART. The initial two vague hypopigmented patches may be of indeterminate variety and with a slow restoration of cell-mediated immunity, these lesions might have transformed into BT Hansens with a mild type 1 reaction. We presume that the subclinical, unnoticed leprosy patches in our case became overt in the form of reaction due to gradual immune restoration induced by HAART as evidenced by slow increase in the CD4+cell count. Supporting our hypothesis, Couppie et al.[5] determined the adjusted hazard ratio for a new diagnosis of leprosy in those receiving HAART for 3 months or more over HIV-infected untreated patients to be 18.5 (95% CI: 1.6 - 217; P = 0.02). Similarly, Sarno et al.[1] also found that the initiation of HAART was associated with a new diagnosis of leprosy (P = 0.001). Talhari et al.[6] also observed two cases of AIDS who had unmasking of multibacillary disease as upgrading reactions.
Therefore, the exacerbations or reactions of leprosy coinfected with HIV are not necessarily due to IRIS, but they can occur independently as a natural course of the disease or HAART itself may act as a trigger to unmask the underlying subclinical infections. We suggest that the criterion for the diagnosis of IRIS may need some modifications, especially with the timing of occurrence of reactions.
| 1. |
Sarno EN, Illarramendi X, Nery JA, Sales AM, Gutierrez-Galhardo MC, Fernandes Penna ML, et al. HIV-M. leprae interaction: Can HAART modify the course of leprosy? Public Health Rep 2008;123:206-12.
[Google Scholar]
|
| 2. |
Deps PD, Lockwood DN. Leprosy presenting as immune reconstitution inflammatory syndrome: Proposed definitions and classification. Lepr Rev 2010;81:59-68.
[Google Scholar]
|
| 3. |
Ustiantowski AP, Lawn SD, Lockwood DN. Interactions between HIV and leprosy: A paradox. Lancet Infect Dis 2006;6:350-60.
[Google Scholar]
|
| 4. |
Deps PD, Lockwood DN. Leprosy occurring as immune reconstitiution syndrome. Trans R Soc Trop Med Hyg 2008;102:966-8.
[Google Scholar]
|
| 5. |
Couppie P, Domergue V, Clyti E, Guedj M El, Vaz T, Sainte-Marie D, et al. Increased incidence of leprosy following HAART initiation: A manifestation of the immune reconstitution disease. AIDS 2009;23:1599-600.
[Google Scholar]
|
| 6. |
Talhari C, De Lima Ferreira LC, Araujo JR,Talhari AC, Talhari S. Immune reconstitution inflammatory syndrome or upgrading type 1 reaction? Report of two AIDS patients presenting a shifting from borderline lepromatous leprosy to borderline tuberculoid leprosy. Lepr Rev 2008;79:429-35.
[Google Scholar]
|
Fulltext Views
3,786
PDF downloads
3,091





