Translate this page into:
Idiopathic acquired persistent true partial to total leukonychia
Correspondence Address:
Shehnaz Z Arsiwala
Dermatocosmetic and Laser Centre, Prince Aly Khan Hospital, Aga Hall Nesbit Road, Mumbai
India
| How to cite this article: Arsiwala SZ. Idiopathic acquired persistent true partial to total leukonychia. Indian J Dermatol Venereol Leprol 2012;78:107-108 |
Sir,
A 35-year-old healthy male patient presented to the clinic with a progressive and persistent total whitening of all the finger nails and the great toe nails since the age of 12 years. The nail changes were a cause of social embarrassments and cosmetic concern to him. Detailed history revealed that he was born out of a non-consanguineous marriage and his developmental milestones were normal. He had no significant childhood illnesses, trauma or surgery. He had no addictions. He was not on any medications, systemic or topical, and not exposed to any chemical agents. He generally used chappals as his daily footwear.
There was no family history of leukonychia or of any other dermatological illnesses.
The onset of leukonychia was at 12 years of age, started with finger nails, bilaterally symmetrical and progressed to involve, simultaneously and synchronously, the nail plates of all the finger nails (leukonychia totalis) and that of the great toe nails with no involvement of the remaining toe nails (leukonychia subtotalis). There was no clinical evidence of atopy, lichen planus, alopecia areata or psoriasis.
On examination, true leukonychia totalis of the finger nails and the great toe nails was seen. The nails were strikingly white, opaque with smooth surface and normal strength [Figure - 1] and [Figure - 2]. The nail bed, nail folds and the edges of the nails were normal. The teeth, eyes, hair, skin of the body and palms and soles showed no abnormality except for minimal xeroderma of the feet. The nails were repeatedly negative for fungus on scraping as well as fungal cultures.
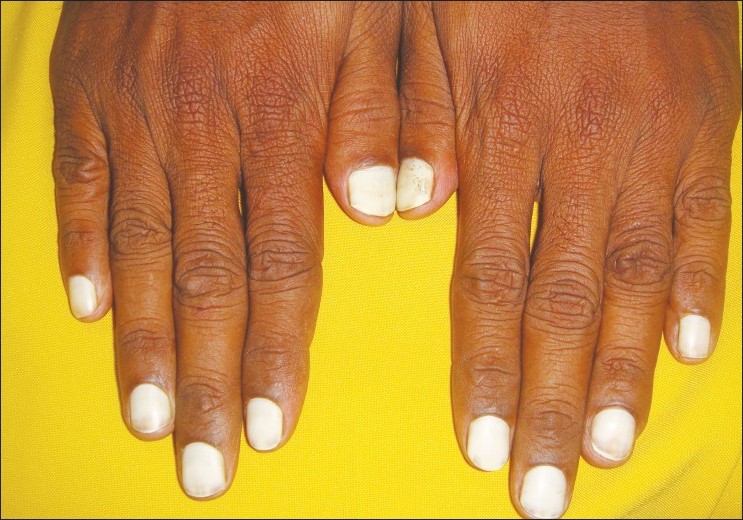 |
| Figure 1: Total leukonychia of the fingernails |
 |
| Figure 2: Total leukonychia of the fingernails and subtotal leukonychia of the toenails |
He had no features of peripheral neurovascular compromise or any other central nervous system disease.
The routine hemogram, urinalysis, liver function tests, renal function tests, total and differential proteins were within normal limits.
Leukonychia is a whitening of the nail plate. Mees in 1919 first described leukonychia as a finding associated with arsenic intoxication. [1]
Leukonychia can be a true leukonychia that involves the nail plate. In apparent (pseudo) leukonychia, there is involvement of subungual tissue due to onycholysis or subungual hyperkeratosis or pathology of matrix or nail bed instead of nail plate. [2]
The physiologic mechanism leading to this phenomenon is not very clear. Newton′s theory is proposed in explaining leukonychia. A white surface is apparent when it reflects the radiation of visible light. In true leukonychia, the origin of the white nail plate is in the matrix. As a result of abnormal matrix keratinization, persistent parakeratosis and keratohyaline granules in the nail plate, parakeratosis and dissociation of the keratin bundles may play a role in the modification of the solar light reflection by the ungual plates. Disorganization of the keratin fibrils leads to diffraction of light in parakeratotic cell and the nail plate appears opaque. True leukonychia may be total or subtotal or temporary or permanent. Partial leukonychia can be punctate, transverse and distal. [2]
Classification of true leukonychia [2] :
- Based on the distribution of white blotches, known as leukonychia punctata, leukonychia striata
- Leukonychia partialis or leukonychia totalis
- Idiopathic true leukonychia is a much rarer condition, with only a few reported cases till date.
The common causes of acquired leukonychia include the following [3] :
- Local trauma
- Exposure to extreme cold
- Disturbed nutrition
- Hepatic cirrhosis
Varied and diverse clinical syndromes have been described in association with total leukonychia, including leukonychia with palmoplantar keratoderma, pili torti, congenital hyperparathyroidism, hypoparathyroidism, onychorrhexis, cataracts and the LEOPARD syndrome. Total leukonychia has also been associated with peptic ulcer disease and cholelithiasis as well as with keratoderma and hypotrichosis. There are a number of autosomal dominantly inherited leukonychia syndromes, including leukonychia totalis in combination with kidney stone and sebaceous cysts, as well as leukonychia, with sensory-neural deafness and knuckle pads, known as the Bart-Pumphrey syndrome. No such associations were seen in the present case.
In 1998, Bongiorno reported a rare case of a 34-year-old patient with persistent, progressive, acquired leukonychia totalis and partialis. This case was the sixth patient with asymptomatic, idiopathic, white fingernails and toenails without a hereditary cause. [2]
Most of the true leukonychia cases are inherited. This case report did not link the inheritance of leukonychia with any of the above-mentioned syndromes. So far, only six cases of idiopathic, acquired, true total leukonychia were found in the literature. [2],[4],[5],[6],[7],[8]
This was a rare case of persistent progressive idiopathic acquired true leuchonychia totalis of the fingernails and great toenails of nonhereditary cause, and is the seventh case report in the world literature.
| 1. |
Mees RA. Een verschijnsel bij polyneuritis arsenicasa. Nederlands Tijdschrift voor Geneeskunde 1919;1:391-6.
[Google Scholar]
|
| 2. |
Bongiorno MR, Aricò M. Idiopathic acquired leukonychia in a 34-year-old patient. Case Report Med 2009;2009:1-3.
[Google Scholar]
|
| 3. |
Yoruk A, Yukselgungor H. Chemotherapy induced transverse leukonychia in children. Int J Dermatol 2003;42:468-9.
[Google Scholar]
|
| 4. |
Butterworth T. Leukonychia partialis: A phase of leukonychia totalis. Cutis 1982;29:363-4,367.
[Google Scholar]
|
| 5. |
Stewart L, Young E, Lim HW. Idiopathic leukonychia totalis and partialis. J Am Acad Dermatol 1985;13:157-8.
[Google Scholar]
|
| 6. |
Grossman M, Scher RK. Leukonychia: Review and classification. Int J Dermatol 1990;29:535-41.
[Google Scholar]
|
| 7. |
Claudel CD, Zic JA, Boyd AS. Idiopathic leukonychia totalis and partialis in a 12-year-old patient. J Am Acad Dermatol 2001;44:379-80.
[Google Scholar]
|
| 8. |
Park HJ, Lee CN, Kim JE, Jeong E, Lee JY, Cho BK. A case of idiopathic leuconychia totalis and partialis. Br J Dermatol 2005;152:401-2.
[Google Scholar]
|
Fulltext Views
4,189
PDF downloads
1,368





