Translate this page into:
Acute hemorrhagic edema of infancy: A report of two cases
Correspondence Address:
Atul Dongre
Department of Skin and VD, OPD No. 117, Seth GS Medical College and KEM Hospital, Parel, Mumbai - 400 012, Maharashtra
India
| How to cite this article: Dongre A, Adhe V, Kothari D, Kardekar S, Khopkar U. Acute hemorrhagic edema of infancy: A report of two cases. Indian J Dermatol Venereol Leprol 2012;78:121 |
Abstract
Acute hemorrhagic edema of infancy is one of the clinical forms of leukocytoclastic vasculitis seen in children. The condition runs a benign course. We report two male children who presented with upper respiratory tract infection followed by limb swelling and purpuric and ecchymotic lesions on the skin. Skin biopsy revealed leukocytoclastic vasculitis in both patients. In both cases, the lesions resolved completely without any sequelae.Introduction
Acute hemorrhagic edema of infancy (AHEI) is an uncommon form of leukocytoclastic vasculitis that affects children younger than 2 years of age. [1] Respiratory tract infections, immunization, and drug intake are considered as precipitating factors. AHEI is characterized by fever, ecchymotic/purpuric lesions, and edema on the extremities and/or face. On histopathology, the skin lesions show leukocytoclastic vasculitis. [2] The clinical features may be confused with Henoch-Schφnlein purpura, erythema multiforme, meningococcemia, and septicemia. In AHEI there is no internal organ involvement, and the disease runs a benign course with spontaneous resolution. The cutaneous findings are dramatic, both in appearance and rapidity of onset, and so may cause significant anxiety for parents as well as clinicians. We report these cases to increase awareness regarding this uncommon but benign form of leukocytoclastic vasculitis.
Case Reports
Case 1
A 2-year-old male child presented with multiple red-colored painful lesions over the face and extremities of 5 days′ duration. He had had symptoms of upper respiratory tract infection, swelling of the right foot, and fever 2 days prior to the eruption of the skin lesions. There was history of treatment for fever with an antipyretic agent prescribed by a general practitioner. The swelling on the right foot had increased to involve the right leg and thigh. Simultaneously, he had developed reddish lesions on the face and the upper and lower extremities. He had no complaints of diarrhea, joint pain, or abdominal pain. On examination, the child was a little irritable and feverish. There was diffuse tender edema over the right upper and lower extremities [Figure - 1],[Figure - 2],[Figure - 3]. Multiple petechiae, purpura, annular patches, and ecchymoses were observed on the lower extremities. Targetoid plaques were seen on the upper extremities. The face and ear lobes also showed purpuric and ecchymotic lesions. There were no lesions on the trunk and oral mucosa. His systemic examination and laboratory investigations, including hemoglobin, complete blood count, liver and renal function tests, and stool and urine examination, were normal. Skin biopsy showed neutrophilic infiltrate in the vessel walls, along with leukocytoclasia [Figure - 4]. There was no vacuolar interface at the dermoepidermal junction and no necrotic keratinocytes in the epidermis, which helped to rule out erythema multiforme. Direct immunofluorescence (DIF) examination did not reveal any deposition in the vessel wall. He was treated conservatively with antipyretics. All the lesions and the edema subsided within 2 weeks.
 |
| Figure 1: Case 1: Edema over the right lower extremity and petechiae, purpura, and ecchymotic lesions on both lower extremities |
 |
| Figure 2: Case 1: Purpura and ecchymoses on the face, lower eyelid, and ear lobe |
 |
| Figure 3: Case 1: Annular purpuric patches and targetoid lesions on the upper extremity |
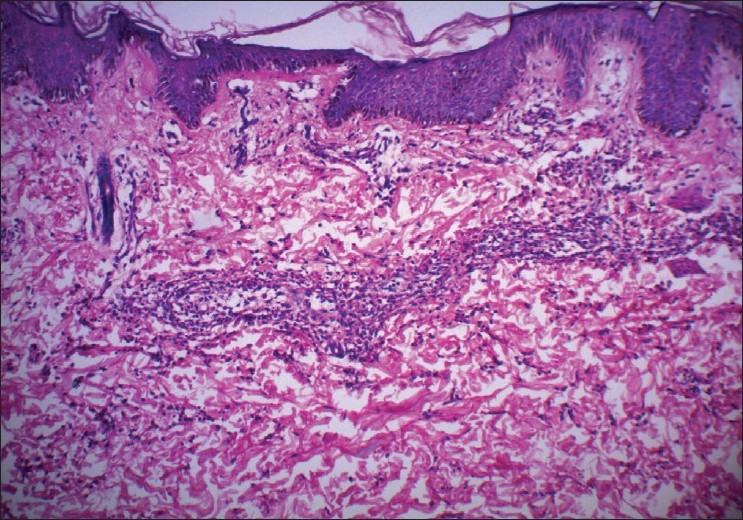 |
| Figure 4: Case 1: Neutrophilic infiltrate in the vessel wall and in the interstitium, along with nuclear dust (leukocytoclastic vasculitis) (H and E, ×20) |
Case 2
A 2-year-old boy was brought to the dermatology outpatient department with red lesions on the extremities and swelling on the right lower limb of 3 and 4 days′ duration, respectively. There was history of fever, cough, and cold prior to eruption of skin lesions and limb swelling. He had no history of abdominal pain, diarrhea, or urinary tract infection. He had received antipyretics for his fever from a private practitioner. On examination, the patient had diffuse nonpitting, nontender edema of the right lower limb, along with multiple purpuric patches and ecchymoses on the right thigh, buttocks, and both upper extremities [Figure - 5] and [Figure - 6]. The face, ears, and trunk were spared. His systemic examination and laboratory tests, including hemoglobin, complete blood count, liver and renal function tests, and stool and urine examination, were unremarkable. Histopathological examination of biopsy from the purpuric lesion showed features of leukocytoclastic vasculitis [Figure - 7]. DIF examination of skin biopsy could not be done due to financial constraints. He was managed symptomatically with antipyretics. Complete resolution of lesions was noted at the end of 10 days.
 |
| Figure 5: Case 2: Purpuric and ecchymotic patches on the right lower limb and diffuse edema |
 |
| Figure 6: Case 2: Large oval ecchymotic plaque on the posterior aspect of the arm |
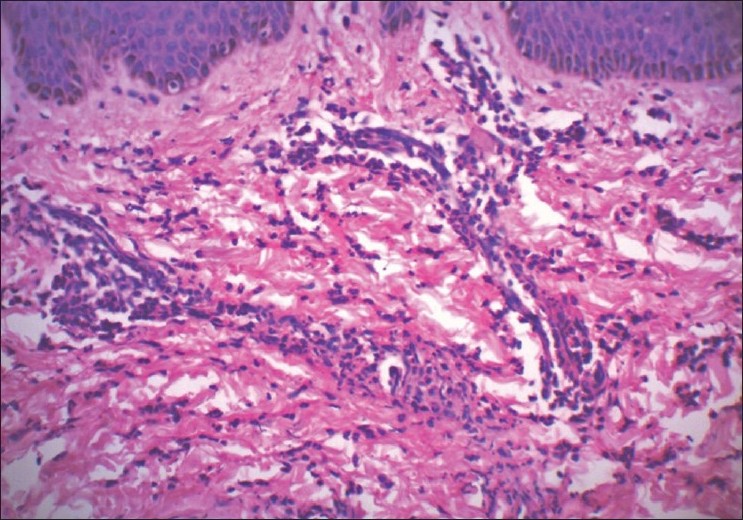 |
| Figure 7: Case 2: Leukocytoclastic vasculitis (H and E, ×25) |
Discussion
AHEI was first described by Snow in 1913. [1] AHEI is also known as Finkelstein disease or medallion-like purpura or infantile postinfectious iris-like purpura and edema. It is a benign, small-vessel leukocytoclastic vasculitis, which typically affects children below 2 years of age. [2]
It is an uncommon disease, characterized by acute onset of large purpuric and ecchymotic lesions on the extremities, face, and ears, along with edema over the extremities and/or face. The trunk is usually spared. Mucosal involvement is rare but has been reported. [3] The lesions present in various forms, which may include purpura, ecchymoses, annular lesions, and cockade or targetoid lesions. Skin lesions are often preceded by edema over the hands and feet. The edema may be tender and asymmetrical at the onset, and can later progress proximally. Edema may occur also on the face and is usually asymmetric. Edema has been consistently described in AHEI; however, there is no statistical data available about its asymmetric or symmetric presentation and also whether any specific factors are associated with asymmetrical edema. These eruptions are often associated with constitutional symptoms like fever and, rarely, joint pains and gastrointestinal symptoms. Despite the explosive onset of the skin lesions, the general condition of the patient remains good.
AHEI is more common in male children. [4] A case series and systematic review of 294 cases by Fiore et al. has reported the age of onset for AHEI to be 2 months to 5 years. [4] However, a case of congenital AHEI that was associated with maternal gastroenteritis 6 weeks before delivery has also been reported in literature. [5] An interesting case report by Lakshmi has described the occurrence of AHEI in an older female child of 5 years of age who presented with extensive truncal involvement, which is an uncommon clinical feature. [6]
The exact etiology of AHEI is unknown. Some authors consider it as an immune complex-mediated vasculitis. [7] Viral and bacterial infections, immunization, and drug intake have been reported as triggering factors for AHEI. [8] Upper respiratory tract infections are the most common type of infections which precedes the onset of AHEI. Cases of AHEI associated with diarrhea due to rotavirus infection have been reported. [9],[10]
The histopathology of purpuric lesions in AHEI is characterized by small-vessel leukocytoclastic vasculitis. Purpuric lesions in children can occur in conditions like Henoch-Schφnlein purpura (HSP), meningococcemia, septicemia, and purpura fulminans. Other differentials for AHEI include urticaria, Kawasaki disease, and erythema multiforme. Although, AHEI has very characteristic clinical features on the basis of which it can be easily distinguished from HSP, there are a few similarities between HSP and AHEI; for example, both are postinfectious sequelae, both have seasonal occurrence, both the conditions favor males, and both show leukocytoclastic vasculitis on histopathology. AHEI differs from HSP by its occurrence in children below 2 years of age, more rapid resolution of the lesions, negative staining for IgA on direct immunofluorescence (DIF), and lack of internal organ involvement.
Though the histopathological findings of HSP are similar to that of AHEI, the lack of vessel-wall staining for IgA on DIF is diagnostic for AHEI. However, IgA deposition can occasionally be found in cases of AHEI. Saraclar et al. has reported deposition of various immunoreactants, including fibrinogen, C3, IgG, IgM, IgA, IgE, and Clq, in the wall and around the small vessels on DIF. In their study IgA deposition was seen in 33% of cases with AHEI. [11] A few cases which appear to overlap with Schφnlein-Henoch purpura have been reported in literature. [12],[13] Some authors consider AHEI to be a purely cutaneous form of HSP, while others believe that AHEI should be regarded as a distinct clinicobiologic entity within the spectrum of leukocytoclastic vasculitis. [14] Although initially considered a variant of HSP, according to current concepts, AHEI is a separate entity because of the lack of (or infrequency of) both visceral involvement and IgA skin depositions on DIF; besides, AHEI has better prognosis as compared to HSP.
No specific treatment is required for AHEI. The role of corticosteroids in the management of AHEI is controversial. The disease runs a benign course and spontaneous resolution of lesions without any sequelae occurs within 2-3 weeks. Rarely, episodes of AHEI may recur. [12]
To summarize, we have described two typical cases of AHEI associated with upper respiratory tract infection in male children who presented with purpuric/ecchymotic lesions and asymmetrical edema of the extremities. Awareness about this uncommon but benign form of leukocytoclastic vasculitis will help to avoid unnecessary treatments, investigations, and anxiety for parents as well as clinicians.
| 1. |
Javidi Z, Maleki M, Mashayekhi V, Tayebi-Maybodi N, Nahidi Y. Acute hemorrhagic edema of infancy. Arch Iran Med 2008;11:103-6.
[Google Scholar]
|
| 2. |
Shah D, Goraya JS, Poddar B, Parmar VR. Acute infantile hemorrhagic edema and Henoch-Schönlein purpura overlap in a child. Pediatr Dermatol 2002;19:92-3.
[Google Scholar]
|
| 3. |
Krause I, Lazarov A, Rachmel A, Grunwald MM, Metzker A, Garty BZ, et al. Acute haemorrhagic oedema of infancy, a benign variant of leucocytoclasticvasculitis. Acta Paediatr 1996;85:114-7.
[Google Scholar]
|
| 4. |
Fiore E, Rizzi M, Ragazzi M, Vanoni F, Bernasconi M, Bianchetti MG, et al. Acute hemorrhagic edema of young children (cockade purpura and edema): A case series and systematic review. J Am Acad Dermatol 2008;59:684-95.
[Google Scholar]
|
| 5. |
Cunningham BB, Caro WA, Eramo LR. Neonatal acute hemorrhagic edema of childhood: Case report and review of the English-language literature. Pediatr Dermatol 1996;13:39-44.
[Google Scholar]
|
| 6. |
Lakshmi C, Srinivas CR. Urticarial vasculitis of infancy (acute hemorrhagic edema). Indian J Dermatol Venereol Leprol 2003;69:427.
[Google Scholar]
|
| 7. |
Roh MR, Chung HJ, Lee JH. A case of acute hemorrhagic edema of infancy. Yonsei Med J 2004;45:523-6.
[Google Scholar]
|
| 8. |
Da Silva Manzoni AP, Viecili JB, de Andrade CB, Kruse RL, Bakos L, Cestari TF. Acute hemorrhagic edema of infancy: A case report. Int J Dermatol 2004;43:48-51.
[Google Scholar]
|
| 9. |
Di Lernia V, Lombardi M, Lo Scocco G. Infantile acute hemorrhagic edema and rotavirus infection. Pediatr Dermatol 2004;21:548-50.
[Google Scholar]
|
| 10. |
Di Lernia V, Ricci C. Skin manifestations with Rotavirus infections. Int J Dermatol 2006;45:759-61.
[Google Scholar]
|
| 11. |
Saraclar Y, Tinaztepe K, Tuncer A. Acute hemorrhagic edema of infancy (AHEI)--A variant of Henoch-Schönlein purpura or a distinct clinical entity? J Allergy Clin Immunol 1990;86:473-83.
[Google Scholar]
|
| 12. |
Legrain V, Lejean S, Guillard JM, Battin J, Maleville J. Infantile acute hemorrhagic edema of the skin:Study of ten cases. J Am Acad Dermatol 1991;24:17-22.
[Google Scholar]
|
| 13. |
Shah D, Goraya JS, Poddar B, Parmar VR. Acute infantile hemorrhagic edema and Henoch-Schönlein purpura overlap in a child. Pediatr Dermatol 2002;19:92-3.
[Google Scholar]
|
| 14. |
Paradisi M, Annessi G, Corrado A. Infantile acute hemorrhagic edema of the skin. Cutis 2001;68:127-9.
[Google Scholar]
|
Fulltext Views
6,142
PDF downloads
2,673





