Translate this page into:
A case of bacillary angiomatosis developed at a burn site
2 Departments of General Surgery and Burn Unit, Erzurum Region Education and Research Hospital, Erzurum, Turkey
3 Departments of Histology and Embryology, Ataturk University, Erzurum, Turkey
4 Department of Dermatology, Ataturk University, Erzurum, Turkey
5 Departments of Microbiology and Clinical Microbiology, Ataturk University, Erzurum, Turkey
Correspondence Address:
Ayse Albayrak
Department of Infectious Diseases and Clinical Microbiology, Erzurum Region Education and Research Hospital, Erzurum
Turkey
| How to cite this article: Albayrak A, Albayrak Y, Unal D, Atasoy M, Uyanik MH. A case of bacillary angiomatosis developed at a burn site. Indian J Dermatol Venereol Leprol 2012;78:121 |
Abstract
Bacillary Angiomatosis (BA) is frequently seen in patients with human immunodeficiency virus (HIV)-induced immunodeficiency. Our patient was a case that developed granuloma-like lesions in the area of a burn, 8 days after being burnt on the upper right arm by scalding water. No indication of immune deficiency was observed and no history of direct contact with cats was evident. By the sixth day of the patient's admission to our clinic, some of the lesions had reached a diameter of 2.5 cm. An excision biopsy was carried out from the lesions present on the patient. Electron microscopy revealed solitary bacilli located close to the capillary wall. Oral erythromycin treatment was implemented at 250 mg, 4 times a day for 2.5 months. Within this period of treatment, the lesions regressed completely, and a complete cure was achieved. This case demonstrates that BA must be considered in the differential diagnosis of both HIV-infected and immunocompetent patients.Introduction
Bacillary Angiomatosis (BA) is an infectious disease caused by Bartonella henselae (B. henselae) or Bartonella quintana (B. quintana) and is frequently seen in patients with human immunodeficiency virus (HIV)-induced immunodeficiency. [1] The cutaneous morphologies of BA can occur as papules, warts, pedunculated or subcutaneous nodules, or hyperkeratotic plaques. [2] The patients usually own a cat or have a history of recent licking, scratching, or biting by a cat. [3] Our patient was a case that developed granuloma-like lesions in the area of a burn 8 days after being burnt on the anterior surface of the upper right arm by scalding water. This patient had no indication of immune deficiency or any history of direct contact with cats.
Case Report
A 5-year-old boy, presented to our clinic with a 6 x 10 cm second degree burn area on the anterior surface of the upper right arm, and with papulonodular lesions on the burn area. The patient had been hospitalized and treatment had begun 9 days previously for burns resulting from spilled scalding water on the anterior surface of the upper right arm. On the sixth day of his hospitalization, the burn scar had been debrided under general anesthesia. Two days after the debridement, soft, painless lesions, similar to granulomas, developed in the burn scar. By the sixth day of the patient′s admittance to our clinic, some of the lesions had reached a diameter of 2.5 cm [Figure - 1]a. The patient had no history of direct contact with cats, no systemic disorder, and no history of drug use before the appearance of the lesions. No pathological findings were detected in laboratory tests that included a full blood count, blood chemistry, full urine analysis, and an HIV test with the ELISA method (third and sixth month controls). An excisional biopsy was carried out from the lesions present on the patient. No reproduction was evident within the waiting period of two days from the biopsy or from the culture prepared from smears taken from the lesions. Light microscopy showed atrophy of the epidermis, edema in the dermis, capillary proliferation, neutrophil-rich mixed inflammatory infiltrate, vascular ectasia, and extravasated erythrocytes [Figure - 2]a and b. Electron microscopy revealed solitary bacilli located close to the capillary wall [Figure - 3]a-c. Perinuclear edema was also observed in macrophage nuclei. The presence of typical skin lesions and the positive response to erythromycin, in addition to the light and electron microscopy findings, led us to reach a diagnosis of BA. The patient was diagnosed with BA based on the clinical, histological, and electron microscopy findings. Oral erythromycin treatment was implemented at 250 mg 4 times a day for 2.5 months. Within this period of treatment, the lesions regressed completely and a complete cure was achieved [Figure - 1]b. No relapse was observed in the 9-month follow-up period.
 |
| Figure 1: (a) Before treatment: The papulonodular lesions observed on the burn surface. (b) After treatment: Macular lesions were seen at the site of the papulonodular lesions |
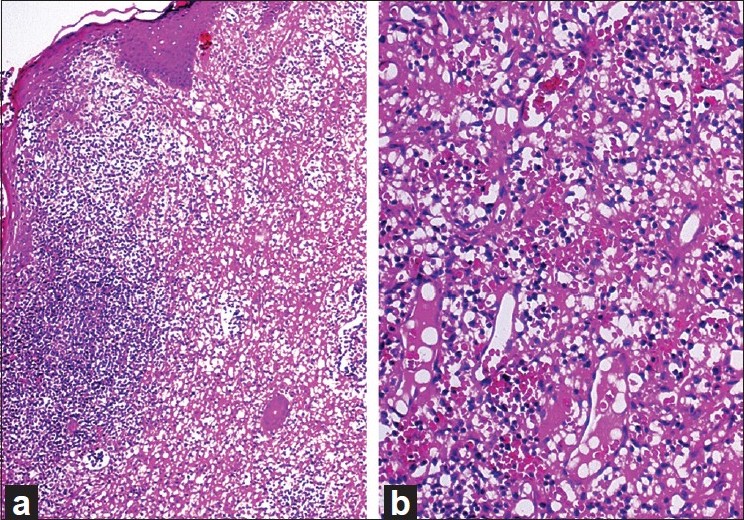 |
| Figure 2: (a, b) Light microscopy shows atrophy of the epidermis, edema in the dermis, capillary proliferation, neutrophil-rich mixed inflammatory infiltrate, vascular ectasia, and extravasated erythrocytes (H and E, ×40, ×100) |
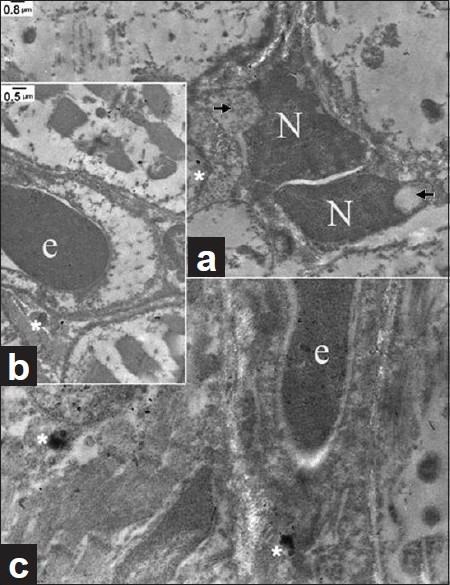 |
| Figure 3: (a-c) Electron micrographs of subcutaneous tissue of patient with bacillary angiomatosis, solitary bacilli* located near capillary wall; N, macrophage's nuclei; e, erythrocyte; arrow, perinuclear edema (Dye: Uranyl acetate-Lead citrate) |
Discussion
BA is caused by B. henselae or B. quintana. Infection by either organism stimulates the proliferation and migration of endothelial cells, resulting in cutaneous BA. [1],[2] BA has an incubation period of about 60 days (range, 10-210 days). [4] BA is very rare in children. In USA, hospitalization rates in 2000 were found to be 0.60 per 100,000 children younger than 18 years of age and 0.86 per 100,000 children younger than 5 years of age. [5] The response to infection with B. henselae depends on the immune status of the infected host. In immunocompetent individuals, the response is granulomatous and suppurative, as compared with a vasoproliferative response in immunocompromised patients. [6] Optimum diagnosis of BA deserves mention: A ′′gold standard′′ for diagnosis does not appear to exist, as only small numbers of patients have been reported and multiple methods have been employed. In many reports, the diagnosis has been based on the demonstration of the bacilli in histological sections stained with silver dyes (such as the Warthin-Starry method), through serological methods, or through culture propagation. [1],[2],[3],[4],[7],[8] Culture of biopsied tissues, electron microscopy (EM) examination, polymerase chain reaction, and serology are other procedures that can be used for BA diagnosis. [1],[3],[4],[8],[9] In particular, EM has been useful for confirming the identity of bacilli when staining techniques have been non-diagnostic. [9] The basic histological architecture of BA is a lobular proliferation of endothelium-lined blood vessels within the superficial dermis. Numerous perivascular neutrophilic granulocytes, especially in deeper regions, are also typically present, together with diffuse formation of blood capillaries ("infectious angiogenesis"). Granulomata are rare. [4]
The cutaneous lesions of BA are usually characterized by pyogenic granuloma-like lesions, subcutaneous nodules, and hyperpigmented indurated plaques, which may sometimes become ulcerated. [10] The differential diagnosis of cutaneous BA includes pyogenic granuloma, lymphocytoma cutis, and Kaposi′s sarcoma. Pyogenic granuloma is an angiomatous papulonodular lesion that usually develops at the site of an injury such as a cut, scratch, or burn. As far as we know, our case is the second case of BA developing after second-degree burns. Although both pyogenic granuloma and BA are rarely encountered after burns, timely and correct differential diagnosis may prevent the development of life- threatening situations.
Systemic manifestations of BA include lymphadenopathy, constitutional symptoms (fever, night sweats, chills, anorexia, and weight loss), and potentially fatal infections of the heart, bone marrow, gastrointestinal tract, and central nervous system. [9],[10] Infection involving the liver and spleen results in a phenomenon known as bacillary peliosis. [2] In the laboratory and from physical examinations of our case, no findings of systemic disorder were determined other than the burn symptoms. BA may be life-threatening in untreated patients. [11]
BA is usually associated with moderate to advanced HIV-induced immunodeficiency. [1],[2] Only a few case reports about BA have been documented in immunocompetent individuals. [2],[3],[4] The present case was immunocompetent, as there was no history of recurrent infections, malignancies, steroid use, or immunosuppressive drug therapy; and no positivity in serological tests for HIV infection.
BA is usually transmitted by a cat scratch, but our patient had no history of contact with a cat. In general, one third of patients with BA have no previous exposure to cats, which suggests that BA may also be acquired in ways other than by direct contact with cats. Ticks, lice, and sand flies have also been implicated in the transmission of various Bartonella species. [1],[4],[7],[10],[12] while B. quintana can be transmitted to humans by arthropods. In our patient, the source of infection may have been one of these alternate vectors for Bartonella infections, which transmitted the causative bacilli to the second-degree burn wound.
Many drugs have been used for the treatment of BA, including doxycycline, trimethoprim-sulphamethoxazole, cephalosporins, aminoglycosides, dapsone, ciprofloxacin, azithromycin or a combination of rifampicin, isoniazid and pyrazinamide. [1],[4],[7] However, the treatment of choice is oral erythromycin. [4],[10] Response to this treatment varies from case to case; some cases resolve rapidly, within several days, while others require a prolonged treatment, even for several months, for resolution. [8] We have diagnosed the case we are presenting as BA based on the clinical, histological, and EM findings, and our patient was successfully treated with erythromycin.
BA is a systemic, life-threatening, but curable infection that causes pyogenic granuloma-like lesions and subcutaneous nodules. This case demonstrates that BA must be considered in the differential diagnosis of immunocompetent patients and not just in HIV-infected individuals. The early diagnosis of BA makes it an easily curable disease and avoids potentially life-threatening issues, even in immunocompetent patients.
| 1. |
Smith DL. Cat-scratch disease and related clinical syndromes. Am Fam Physician 1997;55:1783-9.
[Google Scholar]
|
| 2. |
Mohle-Boetani JC, Koehler JE, Berger TG, LeBoit PE, Kemper CA, Reingold AL, et al. Bacillary angiomatosis and bacillary peliosis in patients infected with human immunodeficiency virus: Clinical characteristics in a case-control study. Clin Infect Dis 1996;22:794-800.
[Google Scholar]
|
| 3. |
Karakas M, Baba M, Aksungur VL, Homan S, Memisoðlu HR, Uðuz A. Bacillary angiomatosis on a region of burned skin in a immunocompetent patient. Br J Dermatol 2000;143:609-11.
[Google Scholar]
|
| 4. |
Maguiña C, Guerra H, Ventosilla P. Bartonellosis. Clin Dermatol 2009;27:271-80.
[Google Scholar]
|
| 5. |
Reynolds MG, Holman RC, Curns AT, O'Reilly M, McQuiston JH, Steiner CA. Epidemiology of cat-scratch disease hospitalizationsamong children in the United States. Pediatr Infect Dis J 2005;24:700-4.
[Google Scholar]
|
| 6. |
Bass JW, Vincent JM, Person DA. The expanding spectrum of Bartonella infections: II. cat-scratch disease. Pediatr Infect Dis J 1997;16:163-79.
[Google Scholar]
|
| 7. |
Schwartz RA, Nychay SG, Janniger CK, Lambert WC. Bacillary angiomatosis: Presentation of six patients, some with unusual features. Br J Dermatol 1997;136:60-5.
[Google Scholar]
|
| 8. |
Rudikoff D, Phelps RG, Gordon RE, Bottone EJ. Acquired immunodeficiency syndrome-related bacillary vascular proliferation (epithelioid angiomatosis): Rapid response to erythromycin therapy. Arch Dermatol 1989;125:706-7.
[Google Scholar]
|
| 9. |
Amsbaugh S, Huiras E, Wang NS, Wever A, Warren S. Bacillary angiomatosis associated with pseudoepitheliomatous hyperplasia. Am J Dermatopathol 2006;28:32-5.
[Google Scholar]
|
| 10. |
Webster GF, Cockerell CJ, Friedman-Kien AE. The clinical spectrum of bacillary angiomatosis. Br J Dermatol 1992;126:535-41.
[Google Scholar]
|
| 11. |
Foucault C, Brouqui P, Raoult D. Bartonella quintana characteristics and clinical management. Emerg Infect Dis 2006;2:217-23.
[Google Scholar]
|
| 12. |
Karakas M, Baba M, Homan S, Akman A, Acar MA, Memisoglu HR, et al. A case of bacillary angiomatosis presenting as leg ulcers. J Eur Acad Dermatol Venereol 2003;17:65-7.
[Google Scholar]
|
Fulltext Views
3,360
PDF downloads
1,992





