Translate this page into:
A new site of milia en plaque
2 Department of Dermatology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Correspondence Address:
Wen-Yuan Zhu
Department of Dermatology, The First Affiliated Hospital of Nanjing Medical University, Nanjing 210029
China
| How to cite this article: Zhang RZ, Zhu WY. A new site of milia en plaque. Indian J Dermatol Venereol Leprol 2012;78:122 |
Sir,
Milia en plaque (MEP) is a rare benign epidermal tumor characterized by numerous tiny milia on an erythematous base that arise spontaneously on healthy skin in predisposed individuals without any apparent causative factor. MEP has preferential areas of involvement including the preauricular area, eyelids, periorbital area, inner canthus, supraclavicular, submandibular, earlobes, nasal bridge, and cheek. [1],[2],[3] To our knowledge, there are no reports of MEP appearing in a patient′s bilateral external auditory canals to date. Here, we describe an elderly female with this condition.
A 65-year-old woman developed skin-colored to gray papules on the internal surfaces of the end points of bilateral auricular canals over a 20-year period. During the first several years of the course, the patient infrequently consulted some dermatologists, but did not gain a definitive diagnosis since she refused to accept an incisional biopsy. Considering the lesions appearing as bilateral and asymptomatic and systemic examination revealing no other abnormality, a dermatologist comforted the patient by explaining to her that the lesions are nonmalignant, but a long-term follow-up was indicated. Therefore, the patient was reluctant to search for more medical opinions. Over the preceding 6 months prior to the initial presentation, the patient occasionally felt itchy. On examination the papules, 3 to 5 mm in diameter were grouped partly confluent and forming both massive lesions, symmetrically located at the end points of bilateral auricular canals [Figure - 1]a and b. A few sporadic papules could be seen around the masses. Close view revealed many slender and darkish hairs growing at the walls of the ear canal entrance. The patient did not have hearing loss and dizziness. Serological investigation for autoimmune diseases including lupus erythematosus was negative. We repeatedly persuaded her to perform a pathological examination, finally she agreed. A biopsy specimen from the lesion (an arrow indicates in [Figure - 1]a) was taken. Histological studies using hematoxylin and eosin (H and E) demonstrated a well-formed cyst just beneath the epidermis. The cyst was enveloped by the stratified squamous epithelium and surrounded by a moderate lymphocytic infiltrate [Figure - 2]a. Alcian blue/periodic acid-Schiff (AB/PAS) staining for mucin was carried out and was negative [Figure - 2]b. Based on the case history, clinical appearance of the lesions and pathologic findings, the diagnosis of MEP was made. The patient was prescribed topical 0.1% adapalene twice daily. Nine months later, the lesions had partially cleared and there was a significant decrease in milia count [Figure - 3]a and b and the patient was advised to continue the treatment.
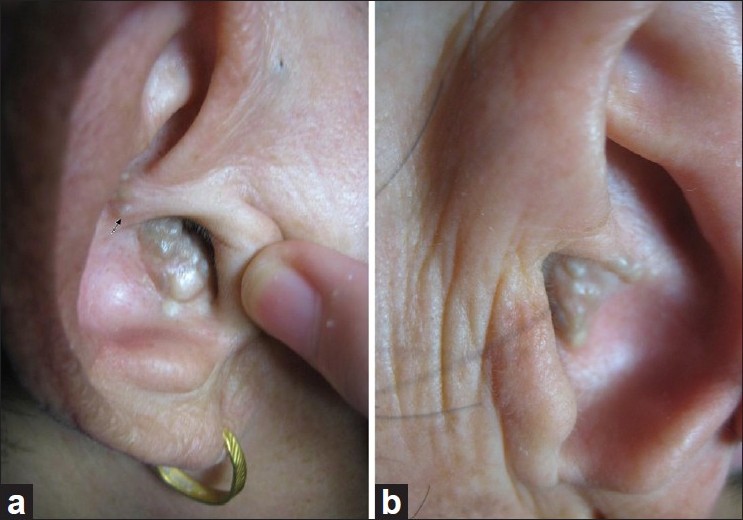 |
| Figure 1: Grouped skin-colored to gray papules, 3 to 5 mm in diameter on erythematous background, symmetrically locating at the end points of bilateral auricular canals (a: right; b: left) |
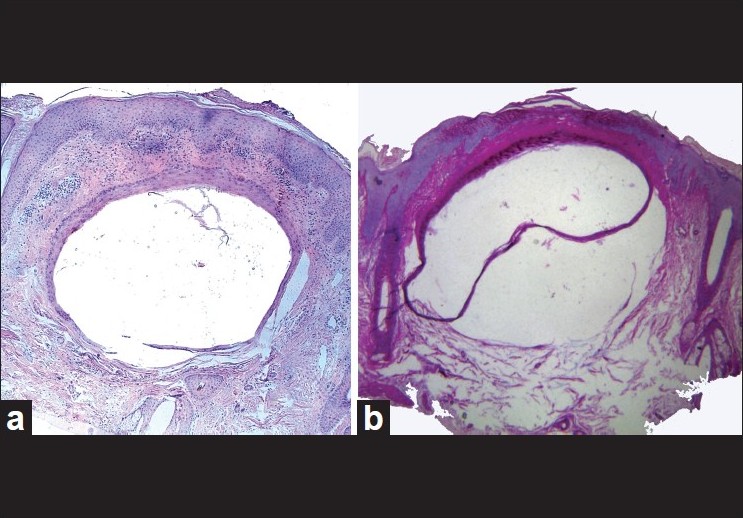 |
| Figure 2: Pathological examination. a: A well-formed cyst just beneath the epidermis was enveloped by the stratified squamous epithelium and surrounded by a moderate lymphocyte infiltrate (H and E, ×40) b: The AB/PAS staining for mucin was negative (×40) |
 |
| Figure 3: Nine months later, the lesions partially cleared and there was a significant decrease in milia count (a: right ear; b: left ear) |
Milia are rather common skin tumors and are classified as primary or secondary. Primary milia are derived from the vellus hair and the secondary milia present represent retension cysts derived from hair follicles and eccrine ducts. MEP is a quite rare variant of milia which occurs spontaneously without identifiable causative factors. The pathogenesis of MEP remains unclear. Some authors proposed damage to the adnexal structures, alteration of the infundibular portion of the follicle, or degeneration of elastic fibers may be attributable to milia formation.
In most of the previous reports, the lesions were distributed in the periauricular area and perioptic area. In 1996, Keohane et al., reported two cases of MEP which occurred on the inferior border of both ear lobes and on the ear lobes and anterior to the right tragus, respectively, and were treated with oral minocycline. [4] In contrast, the lesions in our report were symmetrically situated at the end points of auricular canals. Moreover, these lesions persisted for 20 years which is the longest course of the disease reported so far. We know many old people in China try to get wax out of their ears by poking things into the ear canal. However, our patient denied these actions which can do damage and cause infection. It is worth noting that much slender and darkish hairs growing at the walls of the ear canal were present. The observation may imply the relationship between the formation of milia and vellus hair.
The differential diagnoses include cutaneous myxomas, proliferative trichilemmal tumor and cyst, follicular mucinosis, but the clinical appearance and histopathological features are quite distinctive. In our case, AB/PAS staining for mucin was negative. The finding of H and E staining confirmed the diagnosis of MEP.
MEP is a benign process, but entails cosmetic problems. There is no standard treatment for MEP, but it can be treated by either surgical or medical modalities, including topical tretinoin, oral minocyclin, oral etretinate, ablative laser therapy or cryosurgery, dermabrasion, electrodesiccation, photodynamic therapy, radiosurgical destruction. [1-6] Among them, simple extraction or topical tretinoin is the mostly frequently tried option, with good response, especially in superficially located milia. Our patient obtained a satisfactory result after application of 0.1% adapalene cream for 9 months.
| 1. |
Wollina U. Bilateral milia en plaque of the eyelids: Long eyelashes and unibrow: Case report and review of literature. Dermatol Surg 2010;36:406-8.
[Google Scholar]
|
| 2. |
Hubler WR Jr, Rudolph AH, Kelleher RM. Milia en plaque. Cutis 1978;22:67-70.
[Google Scholar]
|
| 3. |
Ishiura N, Komine M, Kadono T, Kikuchi K, Tamaki K. A case of milia en plaque successfully treated with oral etretinate. Br J Dermatol 2007;157:1287-9.
[Google Scholar]
|
| 4. |
Keohane SG, Beveridge GW, Benton EC, Cox NH. Milia en plaque: New site and novel treatment. Clin Exp Dermatol 1996;21:58-60.
[Google Scholar]
|
| 5. |
Van Lynden-van Nes AM, der Kinderen DJ. Milia en plaque successfully treated by dermabrasion. Dermatol Surg 2005;31:1359-62.
[Google Scholar]
|
| 6. |
Al-Mutairi N, Joshi A. Bilateral extensive periorbital milia en plaque treated with electrodesiccation. J Cutan Med Surg 2006;10:193-6.
[Google Scholar]
|
Fulltext Views
4,921
PDF downloads
2,977





