Translate this page into:
Parthenium dermatitis in India: Past, present and future
Correspondence Address:
Vinod K Sharma
Department of Dermatology and Venereology, AIIMS Teaching Block 4th floor, Ansari Nagar, New Delhi
India
| How to cite this article: Sharma VK, Verma P. Parthenium dermatitis in India: Past, present and future. Indian J Dermatol Venereol Leprol 2012;78:560-568 |
Abstract
Parthenium dermatitis is an immuno-inflammatory disease caused by Parthenium hysterophorus and is the commonest cause of plant dermatitis in India. It is caused by airborne dry and friable plant particles including trichomes, and the most important allergens responsible for allergic contact dermatitis are sesquiterpene lactones. The combined type IV and type I hypersensitivity to parthenium has been recently postulated. In sensitized individuals, it can cause a spectrum of clinical patterns, such as classical airborne pattern, chronic actinic dermatitis-like presentation, mixed pattern dermatitis, exfoliative dermatitis, widespread dermatitis, and other rare patterns. There is definite trend towards change from airborne pattern to chronic actinic pattern in natural history of parthenium dermatitis. Contact sensitivity to parthenium is everlasting, and hence the disease runs a chronic course with exacerbation during summers. Patch testing with acetone or aqueous plant extract is the simplest way of confirming parthenium contact allergy. Management includes avoiding contact with allergen, managing dermatitis with topical corticosteroids/tacrolimus, and other immunosupressives like azathioprine. In future, we expect parthenium dermatitis to become less prevalent due to rapid urbanization and possible development of new biological methods to eradicate the parthenium. Genetic factors associated with susceptibility to parthenium dermatitis need to be studied.Introduction
Compositae plants are among the commonest causes of plant dermatitis and are the second largest family of flowering plants in the world. [1] Compositae dermatitis affects 0.7-1.4% of the general population and 4.5% of the occupationally-exposed groups. [2] Parthenium hysterophorus, a member of compositae family, is popularly known as "bitterweed," "feverfew," or "escobar amarga." In India, it is known as "Congress grass" or "Congress weed," which refers to the US congress (who allocated the shipment for Pune, India). [3] Parthenium is a native of tropical America and was introduced into Asia in cereal and grass seed shipments from U.S.A. during the 1950s and has become the "Scourge of India," producing an epidemic of allergic contact dermatitis. [4] Ranade, Lonkar, and Jog were the first to report parthenium dermatitis at Pune, India, in 1968. Since then, it has been widely reported across the Indian subcontinent. [5] Subsequently, many cases were reported from various parts of the country, namely Bangalore, Hyderabad, Madhya Pradesh, Uttar Pradesh, Haryana, and Himachal Pradesh. [6],[7],[8],[9] The authors have reported epidemics of parthenium dermatitis in Chandigarh and Delhi and in their adjoining states. [2],[8] Presently, Parthenium hysterophorus is the commonest cause of plant dermatitis in India and is responsible for nearly 40% of all patients attending contact dermatitis clinics. [10]
Parthenium hysterophorus
Parthenium hysterophorus belongs to the subfamily asteroidae (tribe heliantheae). It is thought to have originated as a result of natural hybridization between Parthenium confertum and Parthenium Bipinnatifidum. [11] It is an erect annual herb with alternate, deeply-dissected leaves, growing up to 2 m tall with much branched inflorescences bearing white flower heads. [Figure - 1] It grows in almost all types of soil, except near the seashore as the saline soil is not conducive to parthenium flowering. [12] New outbreaks of the weed have been linked to movement of earth and transport of stock, fodder, and grain from Parthenium hysterophorus-infested areas. [13]
 |
| Figure 1: Parthenium hysterophorus with white flower heads |
Pathogenesis
Parthenium dermatitis is an immuno-inflammatory disease, which upon contact sensitization by parthenium antigen propagates as a cell-mediated hypersensitivity immune response with early sensitization phase and a subsequent elicitation phase, if antigen exposure persists. [14] The response is mediated by a series of cellular and molecular mechanisms. Epidermal langerhans′ cells and other cutaneous dendritic cells transport the allergen from the skin to regional lymph nodes where it is presented to T-lymphocytes, and T-cell proliferation occurs with production of effector and memory cells. The reaction is characterized by the infiltration of T-lymphocytes into re-exposed skin sites and the development of cutaneous inflammation.
Akhtar et al showed that all the patients of parthenium dermatitis showed significantly (P < 0.001) elevated levels of TNF-α, IL-6, IL-8, and IL-17 levels as compared to healthy controls and decrease in the anti-inflammatory cytokines IL-4 (P < 0.217) and IL-10 (P = 0.001), suggesting the involvement of pro-inflammatory cytokines in the pathogenesis of parthenium dermatitis. [15] Another study done on Indian cohort showed genetic predisposition to parthenium dermatitis due to lower-producing genotypes of interleukin-10. [14]
Lakshmi et al found that 12 out of the 14 patients of parthenium dermatitis showed a positive prick test. Serum IgE was elevated in all patients to varying degrees. They postulated that a combined immediate (Type I) and delayed hypersensitivity (Type IV) mechanisms may be similarly operational in the initiation and perpetuation of parthenium dermatitis, and that it may also induce exacerbation of lesions of sensitized subjects with atopic diathesis. [16] Although a combination of type III and type IV hypersensitivity had also been postulated, [17] this has been questioned since IgG antibodies that mediate type III hypersensitivity have not been detected. [12]
Mode of sensitization
Parthenium dermatitis is mainly caused by dried leaves and trichomes. Pollen play role, mainly in respiratory allergy. These may not pass beyond the nasal mucosa and hence more often causes allergic rhinitis rather than bronchial asthma. Sesquiterpenelactones (SQLs) have been identified in the leaves, stem, and waxy coat of the pollen, and thus parthenium is capable of producing "dermatitis at a distance" or exacerbating an active outbreak of eczema. [18] Direct or indirect contact sensitization is also possible in view of the rampant growth of the weed.
Allergens in Parthenium hysterophorus
The most important allergens responsible for allergic contact dermatitis are SQLs. [19] They are lipophilic, and are present mainly in the oleoresin fraction of the plant. It is present in the leaf, stem, flower and pollen, but the highest concentrations of SQLs are present in the small glandular hairs (trichomes) present on the undersurface of the leaves and stem. Over 200 skeletal types and 1350 individual types of SQLs have been described, and each of these may have multiple functional groups attached to them. [20]
Among the SQLs, parthenin was found to be the major allergen, the others being coronophillin, tetraneurin A, hymenin etc. Parthenin belongs to the pseudoguinolide class of SQLs. It has an alpha methylene group exocyclic to gamma lactone, which is probably essential for the induction of allergy. Other compositae plants such as Xanthium strumarium, Helianthus annus, Chrysanthemum coronarium, Magnolia stellata and Laurusnobilis also contain similar SQLs and hence these plants may show cross sensitivity with parthenium and vice versa. However, there is no recognized pattern on clinical examination in patients co-sensitized to other plants. Patch and photopatch may reveal co-sensitizers.
Allelopathy and impact on livestock
The phenomenon of allelopathy where one plant exerts a detrimental effect on another through the production of germination and growth inhibiting substances has been well-documented in Parthenium hysterophorous, and water-soluble phenolics and sesquiterpene lactones have been reported from the roots, stems, leaves, inflorescences, pollens, and seeds. [21] The invasive capacity and alleolopathic properties have rendered Parthenium hysterophorus with the potential to disrupt the natural ecosystems. Very sparse or sometimes no other vegetation can be seen in parthenium hysterophorus-dominated areas.
Exposure to Parthenium hysterophorus also causes systemic toxicity in livestock. Alopecia, loss of skin pigmentation, dermatitis, and diarrhea has been reported in animals feeding on parthenium hysterophorus. Degenerative changes in both the liver and kidneys and inhibition of liver dehydrogenases have been reported in buffalo and sheep. The milk and meat quality of cattle, buffalo, and sheep deteriorate on consumption of this weed. [22]
Clinical features
There may be hay fever, asthma or dermatitis [Table - 1] and can be caused by dust and debris from the plant as well as from pollen. [23] A random clinical survey conducted on 2035 residents of Bangalore city with the aid of questionnaires and skin tests revealed that 7.1% of the study population was suffering from allergic rhinitis due to exposure to parthenium pollen. Skin-prick tests performed on 1294 clinic patients suffering from nasobronchial allergy during the past 4 years also showed that 42.5% were sensitive to parthenium pollen. [24] Skin prick test to parthenium was positive in 25 (35.7 %) of 70 patients of atopic dermatitis in a study from Delhi. It suggests that parthenium also plays a role in nasobronchial allergy and atopic dermatitis. [25] The severity of dermatitis in India is greater in comparison to America because the plant grows more abundantly in India and contains large amounts of the sesquiterpene lactone, parthenin. [26] Middle-aged or elderly males who are engaged in outdoor activities and lightly-clothed are commonly affected. Women are less commonly affected (male-to-female ratio 5.5:1 [27] ). This may be possibly because women have lesser exposure as compared to men and their dressing style; however, parthenium dermatitis without direct handling in areas of widespread growth of parthenium has been reported in housewives and indoor workers, suggesting that incidental exposure may sensitize a person to parthenium. Occurrence in teenagers and children is rare. Of 25,000 children employed in the manual pulling of parthenium plants in India, none were known to be sensitized. Studies have shown compositae mix sensitization occurs with higher frequency in atopic children than non-atopics. [28]
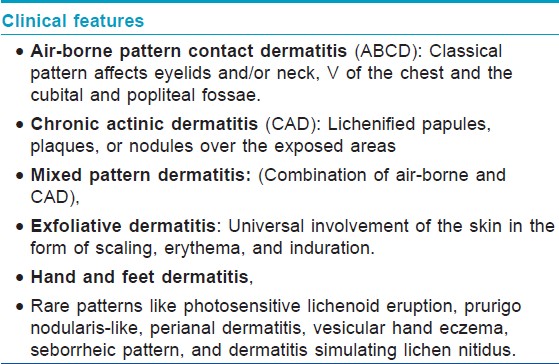
Most of the airborne contact dermatitis starts from the eyelids, suggesting that airborne allergens initially lodge there because of the skin folds and cause dermatitis. A seasonal variation is initially observed with the dermatitis flaring in the summers corresponding to the growing season and disappearing in winters. [29] After several years, persistent pruritic lichenified dermatitis develops without seasonal variation. When such patients move to a parthenium-free area, their dermatitis clears and the skin becomes normal. The perpetuation of parthenium dermatitis may occur through an exposure to contaminated clothes. It can cause a spectrum of clinical patterns, such as classical air-borne pattern, chronic actinic dermatitis (CAD)-like presentation, mixed pattern (combination of airborne and CAD) dermatitis, widespread dermatitis, hand and feet dermatitis, photosensitive lichenoid eruption, and prurigo nodularis-like and other rare patterns.
Classical pattern
It presents as airborne contact dermatitis (ABCD) pattern and affects the face, especially the eyelids and/or neck, V of the chest, and the cubital and popliteal fossae. [Figure - 2] It starts as an acute eczematous reaction that usually appears in the spring and summers and improves during the winters. In sensitized individuals, the manifestations usually starts within 24 hours of exposure, but it may be delayed for up to 2-3 days or even longer in milder cases. In mild cases, dermatitis may manifest as only brief periods of erythema and itching, which subsides within a few hours or days. Moderate dermatitis is characterized by erythema, swelling, papules, or papulovesicles with itching and burning. Severe dermatitis may exhibit extensive vesiculation and exudation associated with edema. Repeated exposures over many years may result in widespread, extensive, and eventually chronic lichenified dermatitis that may persist throughout the year.
 |
| Figure 2: Airborne contact dermatitis pattern. Note diffuse involvement of face including eyelids and neck and V of chest with erythema, oozing, and crusting |
Chronic actinic dermatitis pattern
It manifests as lichenified papules, plaques or papulonodules over the exposed areas [Figure - 3] such as forehead, rim of ears, cheeks, V of chest, nape of neck, dorsae of forearms, and hands. There is relative sparing of the non-sun-exposed areas as eyelids, retroauricular areas, under surface of chin, and depth of the skin folds. Patients with CAD pattern may develop exacerbation over flexures in the summers.
 |
| Figure 3: Chronic actinic dermatitis (CAD)-like pattern. Note lichenified papuloplaques over the dorsa of hands, V of chest, and acutedermatitis over nose and chin. It may be noted eyelids are still involved suggesting evolution through mixed pattern (mixture of ABCD and CAD) |
Mixed pattern
It manifests as scattered infiltrated scaly papules over the exposed parts as in CAD pattern as well as dermatitis over the eyelids and flexural areas of the extremities and the neck as in classical pattern. It represents a transition phase from classic ABCD to CAD pattern in natural history of parthenium dermatitis.
Exfoliative dermatitis
It presents as universal involvement of the skin in the form of scaling, erythema, and induration. [30] There is often a past history of airborne contact dermatitis. Flexural lichenification may be evident in many patients.
Photosensitive lichenoid eruption
Patients present with pruritic, discrete, flat, violaceous papules and plaques over the sun-exposed parts as forehead, ears, cheek, upper chest, upper back, extensor aspect of forearms, and dorsae of hands simulating photosensitive lichenoid eruptions morphologically.
Prurigo nodularis-like lesions
It manifests as multiple hyperkeratotic papules and nodules over the extremities [Figure - 4] with characteristic histopathologic features similar to prurigo nodularis. There is usually a concurrent or a past history of active dermatitis.
 |
| Figure 4: Prurigo-like lesions over dorsa of hands in 18-year-old girl with patch test positive to parthenium |
Other patterns
The other clinical patterns reported are widespread dermatitis of non-airborne contact type, dermatitis of hands and feet, perianal dermatitis, vesicular hand eczema, seborrheic pattern [31] and dermatitis simulating lichen nitidus. [32] In all these variable patterns, patch test contact sensitivity to Parthenium hysterophorus is present. Vitiliginous skin appears to be spared perhaps due to the vacuolization of langerhans cells in these areas. [33] Parthenium hysterophorous may precipitate or exacerbate the atopic dermatitis, which presents with photo aggravation, heat intolerance, and flexural involvement. [29]
Sharma et al studied 74 patients (49 men and 25 women) of parthenium dermatitis with an age range of 22-70 years and the mean duration of 7.7 years. 60 patients had ABCD, 5 patients had mixed pattern, and 9 patients had CAD pattern at the onset. Of the 60 patients with ABCD, 27 changed to CAD pattern and 11 changed to mixed pattern after an average period of 4.2 years. Their results suggested that the clinical pattern of parthenium dermatitis undergoes a significant change after the onset, i.e. progresses from airborne ABCD to mixed pattern or CAD pattern. [2]
The relationship between photosensitivity and parthenium dermatitis has been a mystery. SQLs are not photo sensitizers, they have neither phototoxic nor photoallergic properties. There is only one well-documented case of photocontact dermatitis to parthenium. [34] The reduction in the minimal erythema dose (MED) to UVB and minimal phototoxic dose to UVA has been reported. [35] The photo aggravation of parthenium dermatitis has been reported, [36] but improvement is observed in patients after avoiding further exposure to plant even if they move to a sunny area. Recent study at AIIMS, New Delhi has shown reduced sensitivity to UVB and UVA in CAD due to parthenium. It may be responsible for photolocalization that occurs during natural course of parthenium dermatitis. [37]
Phytophotodermatitis (PPD) is not to be confused with plant dermatitis as it is a cutaneous phototoxic inflammatory eruption, resulting from contact with light-sensitizing botanical substances and long-wave ultraviolet (UV-A 320-380 nm) radiation. Phytophotodermatitis typically manifests as a burning erythema in a bizarre pattern that may subsequently blister. It is not caused by parthenium.
Course of the disease
Contact sensitivity to parthenium is everlasting and hence the disease runs a chronic course with exacerbation during summers. Chronic and recurrent episodes of dermatitis may result in lichenified lesions in the flexural areas. Patients with an initial ABCD subsequently develop localization to the exposed parts that resembles CAD. There may be reduction in the severity of disease due to tolerance, better precautions, and treatment taken by the patient. There are no documented studies of development of tolerance in our patients, with allergic contact dermatitis from parthenium, except by oral hyposensitization, which can be an alternative treatment modality. [38] However, some dermatologist working on parthenium observed that parthenium dermatitis is less severe now, but it may be due to an early diagnosis and treatment with corticosteroids by general practitioners.
Diagnosis
Patch testing with plant allergen [Figure - 5] is the simplest way of confirming parthenium contact allergy. Patch testing can be done with parts of fresh, frozen, and dried plants, but this carries a risk of high false positive irritant reactions and sometimes a risk of test sensitization. Defined SQLs mix is used for the screening of compositae allergy. It consists of a 0.1% mix of equimolar concentrations of 3 different SQLs (alantolactone, costunolide, and dehydrocostuslactone). Testing with the SQL mix was able to detect only 42.2% of those cases that yielded positive results with ethanolic dilutions of ether extracts of the plant and hence is not an adequate screen. Testing with plant extracts can identify most patients with parthenium allergy. The plant allergens can be extracted in various solvents such as acetone, alcohol, ether, acid, alkali, and water and then can be used for patch testing. Solubility of the allergen in the solvent may influence the concentration, which in turn determines the patch test positivity. It has been shown that acetone extract is significantly better than aqueous extract in detecting contact sensitivity to parthenium. [39] The methodology of extraction of antigen from parthenium has already been described in detail in previous report. [18]
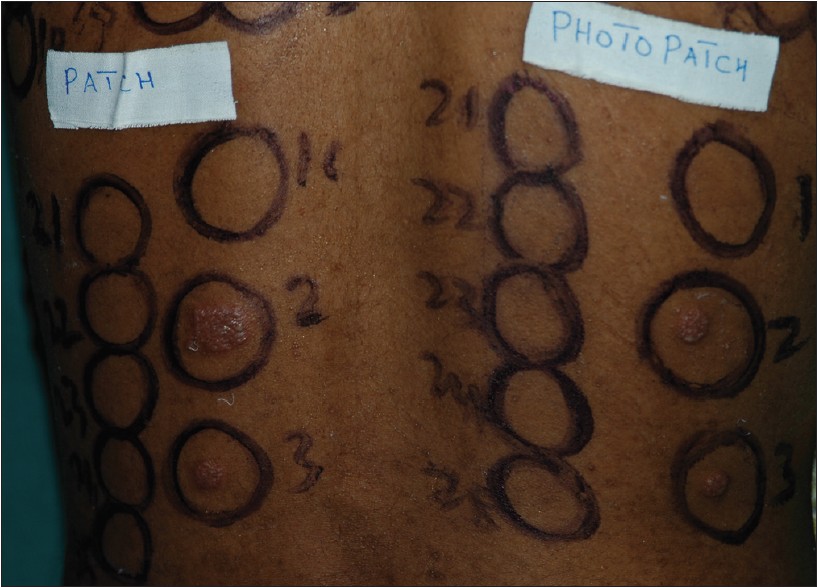 |
| Figure 5: Positive patch test to parthenium. Note patch and photopatch are positive in similar intensity |
Prick test is performed with parthenium antigen included in the Indian standard series (ISS), with leaf "as is" or plant materials crushed and diluted with saline. Both the immediate reaction at 15 mins and the late phase reaction at 24-48 hours should be recorded. [16]
RAST (Radio allergosorbent test) for parthenium specific antibodies is less specific than prick testing. [16]
Histopathology
The contribution of histopathology to diagnosis is limited by frequent overlap in histological findings in different stages of parthenium dermatitis. It can, however, help in ruling out other suspected diagnoses. Acute dermatitis shows epidermal spongiosis with perivascular lymphohystiocytic dermal infiltrate. Photosensitive lichenoid eruption-like lesions on biopsy shows features of chronic non-specific dermatitis. Prurigo may show pronounced hyperkeratosis, irregular acanthosis along with spongiosis. The papillary dermis may show lymphocytic infiltrate with vertically-oriented collagen bundles.
Histopathology in early CAD shows epidermal spongiosis with superficial and deep dermal perivascular lymphohistiocytic infiltrate. In older lesion, however, there is variable often marked acanthosis of the epidermis while spongiosis and lymphocytic infiltrate may be focally prominent. In severe cases, infiltrate may be more prominent, along with marked focal epidermal lymphocyte exocytosis and a degree of irregularity of nuclear outline when cutaneous T cell lymphoma has to be ruled out.
Management
General measures
Severity of dermatitis depends upon degree of contact hypersensitivity and quantity of antigen to which patient is exposed. As the hypersensitivity is difficult to be reduced, only option is to reduce quantity of antigen to which patient is exposed. Since Parthenium hysterophorus is ubiquitous, a change of residence or job is not a suitable option. Also, this would also lead to social and economic consequences. Hence, prevention is aimed at the reduction in the quantity of the antigen to which the patient is exposed. Remove as much of the causative plant as possible from the immediate environment of the patient. Cover as much of the skin as possible by clothing. Wash the uncovered areas of the skin with soap and water as frequently as possible (preferably every 2-3 h) in order to wash off the antigen before it penetrates the skin. Lakshmi and Srinivas [12] recommend us age of a barrier cream more frequently to slow down the penetration of the antigen into the skin and to wash each time before the reapplication of the barrier cream. Avoid the exposure to sunlight; sunscreen lotions may serve as barrier creams. Gloves may not offer protection since the sesquiterpene lactone permeates vinyl, polyethylene, and latex gloves. Drying of clothes indoors also helps in reducing the quantity of antigen. Clothes dried outdoors gather the air borne parthenium allergen. Pieces of cloth dried outside are reported to elicit a positive patch test in a sensitive patient. Avoid going outdoors on days when pollen are present in high concentrations in air. Close all windows in evening when pollen generally settles down to minimize their concentration. Air conditioning decreases indoor pollen counts. Better management of the garden and regular de-weeding is required. Take a bath after coming indoors and wear fresh clothes. No documented studies are available for sunscreen use in parthenium dermatitis, however, if patients have photosensitivity, sunscreens can be used.
Treatment
Corticosteroids are the mainstay of treatment of the parthenium dermatitis, especially in acute cases. Topical steroids can be used for mild to moderate disease while severe/extensive dermatitis will require systemic steroids. Starting doses of 0.5-1 mg/kg/ day of prednisolone or 2-3 mg/day of betamethasone are generally adequate. Complete remission usually occurs within 3 months. Use of high doses for long periods may lead to adrenocortical axis suppression with attendant complications. Hence, effort should be made to taper the steroids accordingly and add adjuvants if required. Management strategies has been described in [Table - 2].
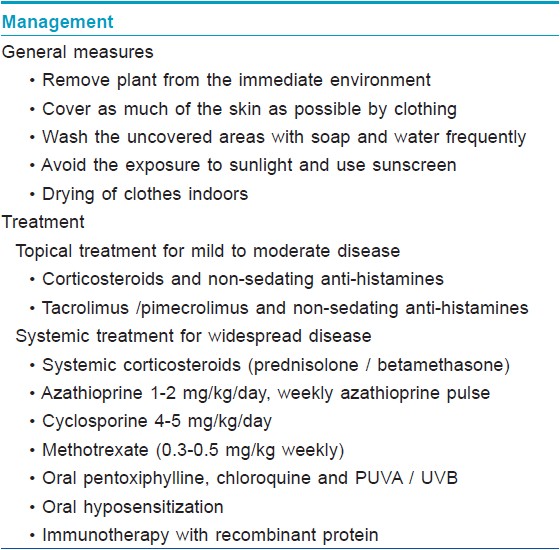
Azathioprine acts as a T cell inhibitor and has immunosuppressive, anti-inflammatory, and steroid-sparing properties. It is effective in the treatment of parthenium dermatitis at the dose of 1-2 mg/kg/day. Various regimes have been tried such as daily doses of 50-150 mg with/without 300 mg monthly bolus doses, the monthly boluses not providing an additional benefit. Weekly azathioprine therapy 300 mg/week was found to be as effective as daily treatment with azathioprine with better compliance and reduced cost of therapy. [40] Authors recommend use of daily azathioprine dose for adequate control of parthenium dermatitis. The treatment may be continued for 6-12 months after subsidence of disease. [41] Its major limitation is that azathioprine takes 4-6 weeks to exert its action. It is preferred for the treatment of chronic stage, and it should be supplemented with corticosteroids in the beginning during the management of acute stage. The major side effects that occur with azathioprine are gastrointestinal intolerance, hepatic dysfunction, and bone marrow suppression. These adverse reactions generally occur at the beginning of the therapy, and people who tolerate it well initially are less likely to have side effects later. TPMT levels are recommended before starting azathioprine. Thiopurine Methyl Transferase (TPMT) is of particular importance because administration of azathioprine to a patient with TPMT deficiency results in significant accumulation of thioguanine nucleotides, and it becomes clinically manifest by increased hematopoietic toxicity. Gastrointestinal side effects do not appear to be related to TPMT deficiency and instead may be related to normal or wild-type TPMT activity. 1 in 300 individuals are homozygous for very low TPMT activity, roughly 10% are heterozygous with intermediate activity, and approximately 90% are homozygous, demonstrating the high methylator phenotype. [42] TPMT testing is not being regularly used as results are not completely reliable.
Verma et al showed azathioprine 100 mg daily (group A) or betamethasone 2 mg daily (group B) given for 6 months in a blinded manner to be almost equally effective (P = 0.0156 vs. 0.0005) in the treatment of parthenium dermatitis. However, adverse effects and relapses were observed to be more frequent in patients treated with betamethasone. [43] Hence, azathioprine must be administered to patients who have relative contraindications to corticosteroids like diabetes mellitus, hypertension etc. or to those not responding to corticosteroids.
Cyclosporine, an immunosuppressive with potent anti-inflammatory actions, has been reported to be effective in the acute phase of parthenium dermatitis. It produces a quicker response and also overcomes the side effects of systemic corticosteroid usage. It suppresses the delayed hypersensitivity reaction as well as the late phase reaction. [44] Side effects of cyclosporine include hypertension and nephrotoxicity. Methotrexate has also been reported to be effective at a dose of 15 mg/week in parthenium dermatitis. [45] Others like topical tacrolimus, pimercolimus, oral pentoxiphylline, chloroquine and PUVA / UVB have been mentioned as treatment modalities, but require further evidence. [46]
Combination/sequential therapies have been suggested, which consists of giving (cyclosporine + azathioprine) × 4-6 weeks followed by daily azathioprine × 6 weeks and then weekly azathioprine as maintenance for 2-5 years.
Oral hyposensitization means that an antigen is introduced into the body by a route different from natural one to induce such a change in the immune system that the body does not develop clinical manifestations when antigen is introduced into the body through normal route. It is thought to act by causing depletion of memory T-cells. Oral hyposensitization was demonstrated to be effective in the 1950s for ragweed dermatitis, but has not been widely accepted because it carries considerable risk of provoking and worsening eczema. The results of oral hyposensitization with parthenium leaf are not consistent, and continued therapy appears to be necessary. Handa et al evaluated the effect of oral hyposensitization as an alternative therapeutic modality in 24 patients of parthenium dermatitis. In 70% of those patients who completed the study, there was a gradual improvement in their clinical status and 30% of patients had an exacerbation during the course of the study. Patients tolerated therapy well and no significant side-effects were seen, except for abdominal pain, ′heartburn,′ and cheilitis. [38]
Immunotherapy with recombinant protein is administered in cases where patients are co-sensitized with several unrelated pollen allergens. Based on frequent co-sensitization patterns, some of the hybrid proteins have been evolved with the polymerase chain reaction. These hybrids contain all the epitopes from the different allergen in a single protein. These have been used for vaccination against pollen allergy. It has been reported useful in hay fever and allergic rhinitis and is under trial for use in ABCD. [47]
Prevention of relapses
Azathioprine or other adjuvants like methotrexate or cyclosporine can be used in maintenance doses. Protection can be given by covering the exposed parts, removal of the agent from the environment, or removal of the patient from the contaminated environment and desensitization methods.
Past, Present, and Future
Clinical picture and management of parthenium dermatitis has changed significantly since its first description by Lonkar et al. The dermatitis is less severe due to prompt diagnosis and treatment. The frequency of exfoliative dermatitis has become less. Parthenium dermatitis is not confined to men, and more and more women are being affected including those working in fields, and even housewives are affected if they regularly walk through parthenium plants or directly handle it. Rarely, children or teenagers playing in parthenium-infested grounds may be affected. Patch test with parthenium is easily available. It is better to avoid patch test with parthenium leaves/flowers as it may lead to sensitization. The acetone extract is preferred, but aqueous extract of parthenium may serve the purpose. Immunosuppressives like azathioprine have become widely accepted in the treatment of parthenium dermatitis and help in long term management of chronic cases. However, patient may have mild summer exacerbation that can be managed with topical corticosteroids/tacrolimus. Tacrolimus has been used with good results in patients with CAD due to parthenium.
What future holds is difficult to predict? We expect parthenium dermatitis to become less prevalent due to rapid urbanization, and more studies on prevalence of parthenium dermatitis need to be carried out. Tacrolimus may become first line of treatment in preference to topical corticosteroids, along with daily azathioprine. There may be an increase in simultaneous type I and IV hypersensitivity due to parthenium due to changing life style, and type I hypersensitivity may increase as happens in developed countries and needs to be monitored. There are already several reports of genetic factors playing role in nickel dermatitis. [48] Similarly, study of genetic factors is needed to develop a test to predict who will develop parthenium dermatitis and may be prevented from exposure.
Immunosuppressives like azathioprine will continue to play an important role in management of chronic parthenium dermatitis.
The eradication of parthenium is difficult, and uprooting and burning of plant does not eliminate allergen as it persists in smoke and ashes. There is urgent need to study new biological methods to eradicate the parthenium.
| 1. |
Paulsens E. Compositae dermatitis: A survey. Contact Dermatitis 1992;26:76-86.
[Google Scholar]
|
| 2. |
Sharma VK, Gomathy S, Bhat R. Evolution of clinical pattern of parthenium dermatitis: A study of 74 cases. Contact Dermatitis 2005;53:84-8.
[Google Scholar]
|
| 3. |
Guin JD. Sesquiterpene-lactone dermatitis. Immunol Allergy Clin North Am 1989;9:447-61
[Google Scholar]
|
| 4. |
Mitchell JC, Calnan CD. Scourge of India. Parthenium dermatitis. Int J Dermatol 1978;17:303-4
[Google Scholar]
|
| 5. |
Tiwari VD, Sohi AS, Chopra T. Allergic contact dermatitis due to pathenium hysterophorus. Ind J Dermatol Venereol Leprol 1979;45:392-400.
[Google Scholar]
|
| 6. |
Sharma VK, Kaur S. Contact dermatitis due to plants in Chandigarh. Indian J Dermatol Venereol Leprol 1987;53:26-30.
[Google Scholar]
|
| 7. |
Bajaj AK, Govil DC, Bhargave SN. Contact dermatitis due to plants. lndian J Dermatol Venereol Leprol 1982;48:268-70.
[Google Scholar]
|
| 8. |
Sharma SC, Kaur S. Airborne contact dermatitis from Compositae plant in Northern India. Contact Dermatitis 1989;21:1-15.
[Google Scholar]
|
| 9. |
Singh KK, Singh G. Air-borne Contact Dermatitis in Varanasi. lndian J Dermatol Venereol Leprol 1986;52:140-2.
[Google Scholar]
|
| 10. |
Sharma VK. Patch testing with the European standard series and compositae extracts in patients with airborne contact dermatitis. Contact Dermatitis 2001;44:49-50.
[Google Scholar]
|
| 11. |
Nath R. Note in the effect of parthenium extract on germination and seedling growth of crops. Indian J Agricultural Sci 1988;51:601-3.
[Google Scholar]
|
| 12. |
Lakshmi C, Srinivas CR. Parthenium: A wide angle view. Indian J Dermatol Venereol Leprol 2007;73:296-306.
[Google Scholar]
|
| 13. |
Mcconnachie AJ, Ltrathie WS, Mersie W, Lgebrehiwot. Current and potential geographical distribution of the invasive plant Parthenium hysterophorus (asteraceae) in eastern and southern Africa. Weed Res 2011;51:71-84.
[Google Scholar]
|
| 14. |
Khatri R, Mukhopadhyay K, Verma KK, Sethuraman G, Sharma A. Genetic predisposition to parthenium dermatitis in an Indian cohort due to lower-producing genotypes of interleukin-10) 1082 G>A and ()) 819 C>T loci but no association with interferon-c (+) 874 A>T locus. Br J Dermatol 2011;165:115-22.
[Google Scholar]
|
| 15. |
Akhtar N, Verma KK, Sharma A. Study of pro- and anti-inflammatory cytokine profile in the patients with parthenium dermatitis. Contact dermatitis 2010;63:203-8.
[Google Scholar]
|
| 16. |
Lakshmi C, Srinivas CR. Type I Hypersensitivity to Parthenium hysterophorus in patients with parthenium dermatitis. Indian J Dermatol Venereol Leprol 2007;73:103-5.
[Google Scholar]
|
| 17. |
Mahajan VK, Sharma NL, Sharma RC. Parthenium dermatitis: Is it a systemic contact dermatitis or an airborne contact dermatitis? Contact Dermatitis 2004;51:231-4.
[Google Scholar]
|
| 18. |
Sharma VK, Sethuraman G. Parthenium Dermatitis. Dermatitis 2007;18:183-90.
[Google Scholar]
|
| 19. |
Lonkar A, Nagasampagi BA, Narayanan CR, Landge AB, Sawaikar DD. An antigen from Parthenium hysterophorus Linn. Contact Dermatitis 1976;2:151-4.
[Google Scholar]
|
| 20. |
Warshaw EM, Zug KA. Sesquiterpene lactone allergy. Am J Contact Dermat 1996;7:1-23.
[Google Scholar]
|
| 21. |
Javaid A, Anjum T. Control of Parthenium hysterophorus L., by aqueous extracts of allelopathic grasses. Pak J Bot 2006;38:139-45.
[Google Scholar]
|
| 22. |
Patel S. Harmful and beneficial aspects of Parthenium hysterophorus: An update. Biotech 2011;1:1-9.
[Google Scholar]
|
| 23. |
McFadyen RE. Parthenium weed and human health in Queensland. Aust Fam Physician 1995;24:1455-9.
[Google Scholar]
|
| 24. |
Sriramarao P, Nagpal S, Rao BS, Prakash O, Rao PV. Immediate hypersensitivity to Parthenium hysterophorus. II. Clinical studies on the prevalence of parthenium rhinitis. Clin Exp Allergy 1991;21:55-62.
[Google Scholar]
|
| 25. |
Kumar S, Khandpur S, Rao DN, Wahaab S, Khanna N. Immunological Response to Parthenium hysterophorus in Indian Patients with Parthenium Sensitive Atopic Dermatitis. Immunol Invest 2012;41:75-86.
[Google Scholar]
|
| 26. |
Towers GH, Mitchell JC, Rodriguez E. Biology and chemistry of Parthenium hysterophorus L. A problem weed in India. J Sci Industrial Res 1997;36:672-84.
[Google Scholar]
|
| 27. |
Singh KK, Singh G. Air borne contact dermatitis in Varanasi. Indian J Dermatol Venereol Leprol 1986;52:140-2.
[Google Scholar]
|
| 28. |
Paulsen E, Otkjær A and Andersen KE. Sesquiterpene lactone dermatitis in the young: Is atopy a risk factor?. Contact Dermatitis 2008;59:1-6.
[Google Scholar]
|
| 29. |
Shenoi SD, Srinivas CR. Changing clinical patterns of parthenium dermatitis. Contact Dermatitis 1997;37:128.
[Google Scholar]
|
| 30. |
Agarwal KK, Nath AK, Jaisankar TJ, D'Souza M. Parthenium dermatitis presenting as erythroderma. Contact Dermatitis 2008;59:182-3.
[Google Scholar]
|
| 31. |
Sethuraman G, Bansal A, Sharma VK and Verma KK. Seborrhoeic pattern of parthenium dermatitis. Contact Dermatitis 2008;58:372-4.
[Google Scholar]
|
| 32. |
De D, Jindal R, Kanwar AJ. Contact dermatitis to parthenium simulating lichen nitidus. Indian J Dermatol Venereol Leprol 2010;76:286-7.
[Google Scholar]
|
| 33. |
Singh KK, Srinivas CR, Balachandran C, Menon S. Parthenium dermatitis sparing vitiliginous skin. Contact Dermatitis 1987;16:174.
[Google Scholar]
|
| 34. |
Bhutani JK, Rao DS. Photocontact dermatitis caused by Parthenium hysterophorus. Dermatologica 1978;157:206-9.
[Google Scholar]
|
| 35. |
Srinivas CR, Shenoi SD. Minimal erythema dose to ultra violet light in parthenium dermatitis. Indian J Dermatol Venereol Leprol 1994;60:149-50.
[Google Scholar]
|
| 36. |
Jeanmougin M, Taieb M, Mancieb JR, Moulin JP, Ciratte J. Photo-aggravated Parthenium hysterophorus contact eczema. Ann Dermatol Venereol 1988;115:1238-40.
[Google Scholar]
|
| 37. |
Wadhwani A. A Study of Clinical Spectrum of Photodermatoses with Focus on Chronic Actinic Dermatitis. MD Dermatology Venereology Thesis submitted to All India Insitute of Medical Sciences, Nov 2010.
[Google Scholar]
|
| 38. |
Handa S, Sahoo B and Sharma VK. Oral hyposensitization in patients with contact dermatitis from Parthenium hysterophorus. Contact Dermatitis 2001;44:279-82.
[Google Scholar]
|
| 39. |
Sharma VK, Sethuraman G, Tejasvi T. Comparison of patch test contact sensitivity to acetone and aqueous extracts of Parthenium hysterophorus in patients with air borne contact dermatitis. Contact Dermatitis 2004;50:230-2.
[Google Scholar]
|
| 40. |
Verma KK, Bansal A, Sethuraman SG. Parthenium dermatitis treated with azathioprine weekly pulse doses. Indian J Dermatol Venereol Leprol 2006;72:24-7.
[Google Scholar]
|
| 41. |
Sharma VK, Chakrabarti A, Mahajan V. Azathioprine in the treatment of parthenium dermatitis. Int J Dermatol 1998;37:299-302.
[Google Scholar]
|
| 42. |
Patel AA, Swerlick RA, McCall CO. Azathioprine in dermatology: The past, the present, and the future. J Am Acad Dermatol 2006;55:369-89.
[Google Scholar]
|
| 43. |
Verma KK, Mahesh R, Srivastava P, Ramam M, Mukhopadhyaya AK. Azathioprine versus betamethasone for the treatment of parthenium dermatitis: A randomized controlled study. Indian J Dermatol Venereol Leprol 2008;74:453-7.
[Google Scholar]
|
| 44. |
Lakshmi C, Srinivas CR, Jayaraman A. Ciclosporin in parthenium dermatitis -a report of 2 cases. Contact Dermatitis 2008;59:245-8.
[Google Scholar]
|
| 45. |
Sharma VK, Bhat R, Sethuraman G, Manchanda Y. Treatment of Parthenium dermatitis with methotrexate. Contact Dermatitis 2007;57:118-9.
[Google Scholar]
|
| 46. |
Dogra S, Parsad D, Handa S. Narrow band ultraviolet B in air borne contact dermatitis: A ray of hope!. Br J Dermatol 2004;150:367-99.
[Google Scholar]
|
| 47. |
Cromwell O, Niederberger V, Horak F, Fiebig H. Clinical Experience with Recombinant Molecules for Allergy Vaccination. Curr Top Microbiol Immunol 2011;352:27-42.
[Google Scholar]
|
| 48. |
Kassinen SS, Ikaheimo I, Tiilikainen A. TAP1 and TAP2 genes in nickel allergy. Int Arch Allergy Immunol 1997;114:94-6.
[Google Scholar]
|
Fulltext Views
32,928
PDF downloads
5,160





