Translate this page into:
Pseudopelade of Brocq in two brothers: Possible role of hereditary factors in the pathogenesis
2 Department of Pathology, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology, and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh
India
| How to cite this article: Singh S, De D, Saikia UN, Kanwar AJ. Pseudopelade of Brocq in two brothers: Possible role of hereditary factors in the pathogenesis. Indian J Dermatol Venereol Leprol 2012;78:637-640 |
Sir,
Pseudopelade of Brocq is a primary lymphocytic cicatricial alopecia characterized by flesh colored patches of alopecia without apparent perifollicular inflammation. [1] Only few cases of pseudopelade of Brocq occurring in multiple members of the same family have been previously reported. [2],[3],[4],[5] We herein present a further report of familial pseudopelade of Brocq (PPB) occurring in two brothers in their third decade.
A 29-year-old young man (index case) presented with a complaint of patchy hair loss over scalp for the last 2 years. He was continuing to develop new lesions and the older lesions were also gradually increasing in size, although the lesions themselves were asymptomatic. His younger brother, who was 26 years old, also gave history of similar patches over scalp. The younger brother had the lesions for the past 3-4 years and the disease was similarly progressive as his elder brother, but was more extensive than in the latter. There was no history of papules, pustules or plaques preceding the alopecia in any of the brothers. Also, there was no history of any other cutaneous or systemic illness in both of them. On examination of the index case, there were multiple, 1-2 cm sized, discrete-to-confluent patches of scarring hair loss over the vertex, occipital and parietal scalp. The patches were showing minimal atrophy and wrinkling and were skin colored. But scarring was present, characterized by shiny skin with lack of follicular ostia [Figure - 1]a. There was complete absence of any inflammation, either within or around the patches/surrounding follicles and there were no scaling, crusting or follicular papulo-pustules. Examination with a magnifying lens did not reveal any exclamation mark hair or any leucotrichic hair in the surrounding area. Hair pull test was negative. The younger brother had similar lesional morphology, but more extensive involvement of the vertex [Figure - 1]b, parietal, occipital and temporal areas of scalp. Rest of the scalp, facial and body hair were uninvolved in both brothers and there were no other cutaneous, mucosal or nail findings. KOH examination from the scalp and adjacent hair was done just to rule out tinea capitis, and it was negative in both siblings. Skin biopsy, with the differentials of pseudopelade of Brocq and long standing alopecia areata, was done from representative sites in both brothers. It showed unremarkable epidermis and a single follicular scar traversing the dermis longitudinally without any surrounding scarring or inflammation, along with atrophy of arrector pili and complete absence of the sebaceous unit [Figure - 2], the histopathological findings being compatible with PPB in accordance with criteria given by Braun-Falco et al. [6] There was no history of alopecia in any other family member except for patchy baldness in maternal uncle [[Figure - 3], showing the pedigree chart], which was reported to be persistent, despite using several therapies (he was unavailable for examination). None of them had taken any definitive treatment in the past. We started both brothers on oral mini pulse (dexamethasone 2.5 mg each on 2 consecutive days every week) in order to arrest disease progression which had occurred more rapidly over the past 6 months. But they were subsequently lost to follow up.
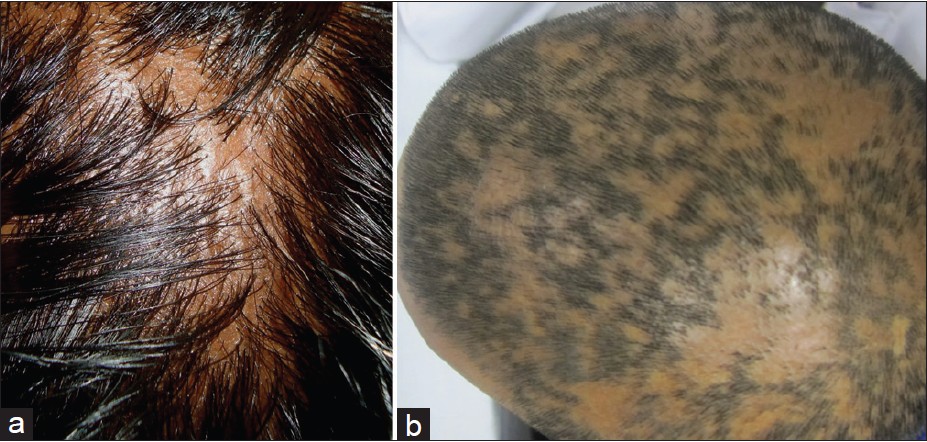 |
| Figure 1: (a) Elder brother (index case) with scarring alopecia showing typical "footprints in the snow" appearance and lack of atrophy. (b) Younger brother with extensive cicatricial alopecia on vertex showing reticulate pattern of scarring |
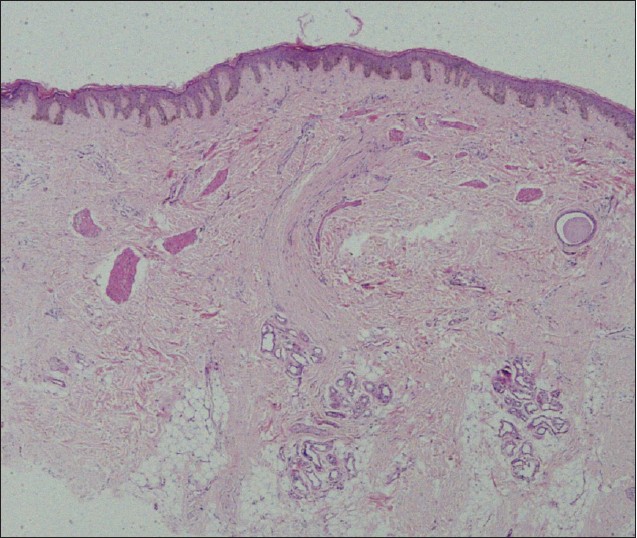 |
| Figure 2: Unremarkable epidermis with paucity of pilosebaceous units and no dermal inflammation. A linear scar is replacing the follicle completely (running perpendicular to the epidermis) and is surrounded by atrophic arrector pili. There is no widespread scarring (H and E, x40) |
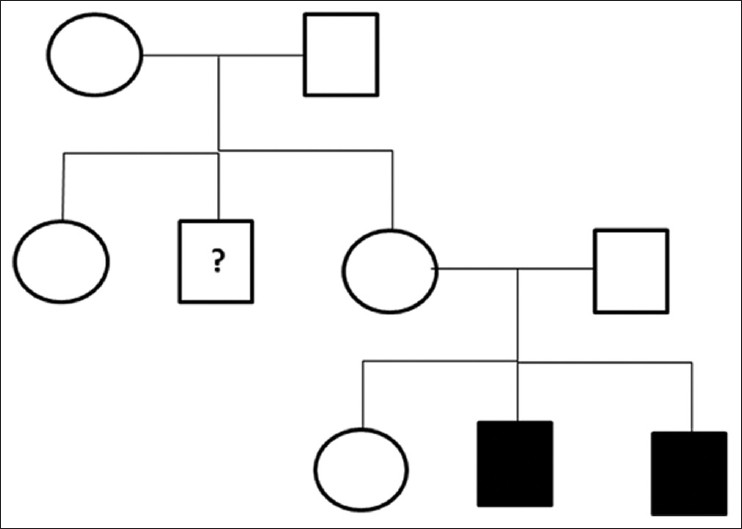 |
| Figure 3: Pedigree chart showing affected siblings as solid blocks. Maternal uncle (?) had history of persistent patchy alopecia but was unavailable for examination |
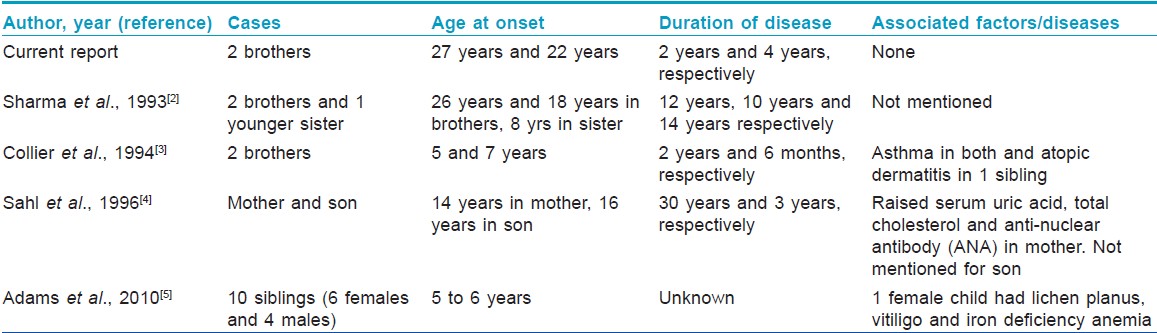
Pathogenesis of PPB is not completely understood as yet. Some of the suspected factors include acquired autoimmunity, Borrelia infection and senescence of follicular stem cell reservoir. [7] Few case reports and case series of familial PPB indicate that heredofamilial factors may be important in its pathogenesis [Table - 1]. Although Sahl et al[4] have proposed that PPB could be transmitted in an autosomal dominant pattern, we have our reservations about it. First, the Mendelian inheritance is complex and can be known accurately only if complete pedigree evaluation of two to three generations is carried out. Second, inheritance patterns of a hitherto non familial disorder cannot be generated based on a single or even few case reports. Third, no single pattern of inheritance can be proposed from the above reported cases. Finally, considering that most of the cases have shown variations in age of onset and clinical extent, incomplete penetrance and variable expressivity may also be suggested. In addition, since most of the familial cases have been among siblings, an infectious agent inciting the follicular inflammation and thus leading to cicatricial alopecia cannot be ruled out with certainty. If we consider maternal uncle of our patients to have PPB (which could not be confirmed clinically or histologically), then the pattern in our cases seems to be that of X linked recessive inheritance. Therefore, detailed genetic studies and linkage analysis are required to conclusively prove that genetic factors are playing a role in the causation of PPB and current data on this is sufficient merely to arouse suspicion and not to prove.
Treatment of PPB is difficult as with other scarring alopecias and no standard protocol exists. Active disease, as assessed by progression of lesions or hair pull test positivity or the presence of lesional symptoms, needs to be treated. Variable success rates have been reported with topical corticosteroids, intralesional triamcinolone acetonide (10 mg/mL), prednisone, oral mini pulse (OMP), hydroxychloroquine, isotretinoin and mycophenolate mofetil. [7],[8] Surgical options are considered when the disease is stable for at least two years and include autologous hair transplantation and scalp reduction surgery. Oral mini pulse (oral dexamethasone/betamethasone on two consecutive days every week) has been used extensively in India for reducing side effects of daily steroids in disorders like active/ progressive vitiligo, alopecia areata and lichen planus. Oral mini pulse has also been mentioned as a treatment modality for cicatricial alopecias, [9] which we used in our patients.
| 1. |
Olsen EA, Bergfeld WF, Cotsarelis G, Price VH, Shapiro J, Sinclair R, et al. Summary of North American Hair Research Society (NAHRS)-sponsored workshop in cicatricial alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol 2003;48:103-10.
[Google Scholar]
|
| 2. |
Sharma DK, Pandey SS. Familial incidence of pseudopelade of Brocq. Indian J Dermatol Venereol Leprol 1993;59:218-9.
[Google Scholar]
|
| 3. |
Collier PM, James MP. Pseudopelade of Brocq occurring in two brothers in childhood. Clin Exp Dermatol 1994;19:61-4.
[Google Scholar]
|
| 4. |
Sahl WJ. Pseudopelade: An inherited alopecia. Int J Dermatol 1996;35:715-9.
[Google Scholar]
|
| 5. |
Adams D, Nasir H, Seiger E, Mahon M. Familial pseudopelade of Brocq [WWW document], 2010. Available from: http://www.aocd.org/jaocd/jaocd-2010-jly.pdf [Last accessed on 2011 Nov 25].
[Google Scholar]
|
| 6. |
Braun-Falco O, Imai S, Schmoeckel C, Steger O, Bergner T. Pseudopelade of Brocq. Dermatologica 1986;172:18-23.
[Google Scholar]
|
| 7. |
Ross EK, Tan E, Shapiro J. Update on primary cicatricial alopecias. J Am Acad Dermatol 2005;53:1-37.
[Google Scholar]
|
| 8. |
Alzolibani AA, Kang H, Otberg N, Shapiro J. Pseudopelade of Brocq. Dermatol Ther 2008;21:257-63.
[Google Scholar]
|
| 9. |
Parsad D, De D. Corticosteroid mini pulses. In: Picardo M, Taieb A, editors. Vitiligo. 1 st ed. Berlin: Springer; 2010. p. 377-9.
[Google Scholar]
|
Fulltext Views
6,785
PDF downloads
1,621





