Translate this page into:
Elephantiasis nostras verrucosa: A rare case of thyroid dermopathy
2 Department of Dermatology, A.O.R.N. "A. Cardarelli", Naples, Italy
Correspondence Address:
Rossella Alfano
Department of Dermatology, Second University of Naples, Via Pansini 5, 80131 Naples
Italy
| How to cite this article: Lo Schiavo A, Caccavale S, Alfano R, Puca RV, Cozzi R. Elephantiasis nostras verrucosa: A rare case of thyroid dermopathy. Indian J Dermatol Venereol Leprol 2012;78:650-652 |
Sir,
An obese 43-year-old male presented to our dermatology department with a bilateral non-pitting edema of both legs. His legs had "woody" appearance [Figure - 1] and were covered with profoundly malodorous, fungating, verrucous skin lesions. There was an ulcerative infected lesion on the lateral malleolus of the left extremity that was causing him severe pain [Figure - 2]. He noticed that the swelling of the legs began 9 years ago, since he was forced to a wheelchair due to a spinal cord injury. The lymphedema has started with swelling of the dorsum of his feet, and then with a progressive involvement of the front and the back of legs. It is to be noted that the leg ulcer has developed and grown constantly in size during the last year. His toenails showed a marked pachyonychia and onycogryphosis. On examination digital clubbing, tachycardia and eyeballs′ protrusion were noted. His medical history revealed obesity (BMI 48 kg/m 2 ) and Graves′ disease; it reported a trauma to the lower limbs whereas was negative for filariasis, surgery, radiation, neoplasia and familial Milroy′s disease. Laboratory evaluation revealed elevated serum levels of glucose (35 mg/ dl due to uncontrolled type 2 diabetes mellitus), triglycerides (321 mg/ dl), and cholesterol (Total cholesterol/high-density lipoprotein cholesterol of 4, 3), thyroid hormonal profile compatible with hyperthyroidism (T3 5 ng/ ml; T4 160 ng/ml; TSH 0.2 mIU/ml) and positivity of anti-TSH receptor (10.2 U/l, normal range:<9 U/l), anti-thyroid peroxidase (37 IU/ml, normal range:0-30 IU/ml) and anti-thyroglobulin antibody (142 IU/ml, normal range 0-40 IU/ml) neither signs of hepatic or renal disease, nor clinical or echo-cardio-graphical signs of cardiac failure. No evidence of chronic venous insufficiency at duplex ultrasonography was seen. Blood examination did not reveal eosinophilia, filarial serology (IgG enzyme immunoassay) was negative and microfilariae weren′t seen on a blood film taken at 4 pm and 1 am. Tissue cultures of specific body areas showed Trichophyton rubrum, Candida albicans, and β-hemolytic Streptococcus group; while, blood cultures were negative. A skin-biopsy was performed in order to exclude malignancy. It showed epidermal thickening, hyperkeratosis with orthokeratosis and acanthosis, as well as lymphangiectasia and chronic lymphocytic infiltrate in papillary dermis. Mucin staining showed increased mucin deposition within the dermal fenestration and glycosaminoglycans in the reticular dermis [Figure - 3]. HPV DNA-search by PCR was negative. These dermatological findings were consistent with elephantiasis nostras verrucosa. Differential diagnoses include filariasis, chromoblastomycosis, lipodermatosclerosis, verrucous carcinoma, papular mucinosis, obesity-associated lymphoedematous mucinosis. [1],[2] Lyphoedematous mucinosis deserves particular mention because it simulates pretibead myxedema: we exclude it because of the presence of clinical feature of thyroid disease, the lack of hemosiderin deposition and vessel modification and the mucin accumulation on deeper dermis. [2] Elephantiasis nostras verrucosa is an uncommon dermatologic disease which is the result of progressive lymphedema complicated by chronic dermal fibrosis and papillomatous eruption with a cobblestone-like appearance deforming the skin. A variety of etiologies can lead to lymphatic obstruction and edema including neoplasia, trauma, Kaposi′s sarcoma, scleroderma, hypothyroidism, but obesity and soft-tissue infection are the predominant risk factors. [3] All forms of elephantiasis share a common pathogenic mechanism: an occult or clinically manifest disruption of the skin barrier results into a nidus for bacterial infection. Recurrent attacks of lymphangitis play a critical role, leading to obstruction and insufficient lymphatic drainage. In our case the presence of ophthalmopathy, hyperthyroidism and the typical localization of lesions let us to diagnosis this elephantiasis as an extremely rare form of thyroid dermopathy: increased levels of glycosaminoglycans cause compression and occlusion of small local lymphatics leading to the accumulation of fluid, swelling and dermal edema. [4] The initiating factor for development of elephantiasis has been patient′s immobility but obesity also has contributed: excessive adipose tissue impaired lymphatic flow led to the accumulation of protein-rich fluid, fibrosis, inflammation and susceptibility to the infection. Elephantiasis′ therapy is a challenge. In our case, a conservative therapy has been adopted to reduce venous stasis and edema using compression stockings and elastic bandages combined with organic diuretics. Oral itraconazole (200 mg per day) and amoxicillin plus clavunalate (1 g twice daily) have been the winning weapons in reducing the local infections. Systemic retinoid therapy hasn′t been deemed appropriate due to hyperlipidemia demonstrated by laboratory, thus it has been necessary to use topical urea-based keratolytics. [5] In order to defeat the development of the disease, our patient was also started on treatment for obesity and hyperthyroidism. After 2 months a moderate improvement was shown. Elephantiasis nostras verrucosa is a poorly understood disease leading to debilitating deformities. To our knowledge, this is one of the few cases reported in literature, in which on the background of a Graves′ disease a precipitant factor, as immobility and obesity, determine the impairment of lymphatic flow leading to elephantiasis. [4],[5]
 |
| Figure 1: Non pitting edema of lower legs with typical cobblestone like findings |
 |
| Figure 2: Ulcerative infected lesion on the left leg |
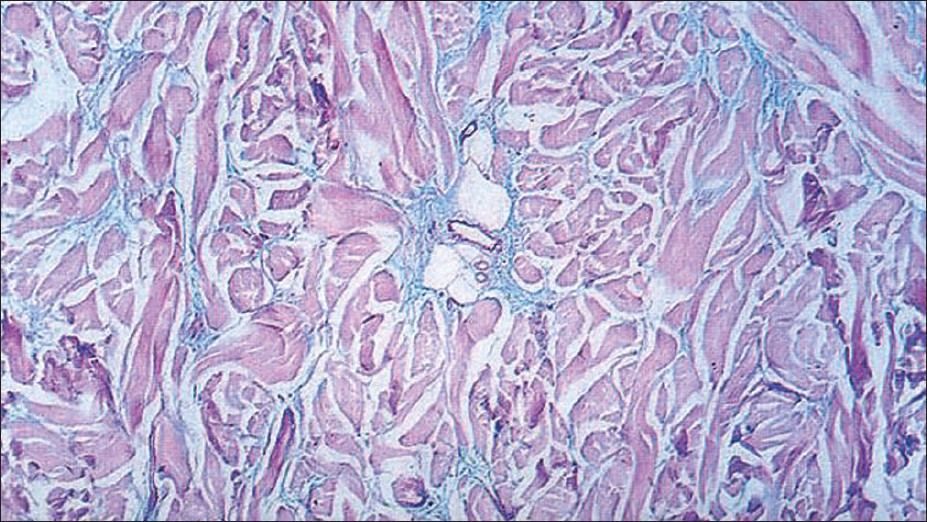 |
| Figure 3: Mucinous oedema with fibroblast proliferation (Alcian blue stain, ×100) |
| 1. |
Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: A review. Am J Clin Dermatol 2008;9:141-6.
[Google Scholar]
|
| 2. |
Rongioletti F, Donati P, Amantea A, Ferrara G, Montinari M, Santoro F, et al. Obesity-associated lymphoedematous mucinosis. J Cutan Pathol 2009;36:1089-94.
[Google Scholar]
|
| 3. |
Dean SM, Zirwas MJ, Horst AV. Elephantiasis nostras verrucosa: An institutional analysis of 21 cases. J Am Acad Dermatol 2011;64:1104-10.
[Google Scholar]
|
| 4. |
Ukinç K, Bayraktar M, Gedik A. Hypothyroid Graves' disease complicated with elephantiasis nostras verrucosa (ENV): A case report and review of the literature. Endocrine 2009;36:6-9.
[Google Scholar]
|
| 5. |
Kakati S, Doley B, Pal S, Deka UJ. Elephantiasis Nostras Verrucosa: A rare thyroid dermopathy in Graves' disease. J Assoc Physicians India 2005;53:571-2.
[Google Scholar]
|
Fulltext Views
7,961
PDF downloads
2,370





