Translate this page into:
Migratory "moles" - dermoscopic diagnosis
Correspondence Address:
Manjot Marwah
107/5, Shere-Punjab, Mahakali Caves Road, Andheri (East), Mumbai-400093, Maharashtra
India
| How to cite this article: Marwah M, Gautam M, Patil S, Nadkarni N, Godse K. Migratory "moles" - dermoscopic diagnosis. Indian J Dermatol Venereol Leprol 2012;78:665 |
Sir,
Pediculosis pubis (PP) is infestation with pubic lice of the species Phthirus pubis. Direct contact is the primary source of transmission. In adults, PP most frequently occurs as a sexually transmitted disease (STD), commonly associated with other STDs. [1] However, transmission may occur from sheets and clothing. Phthirus pubis habituates regions that are rich in apocrine glands, so predilection sites are pubic area, axillae, and eyelashes. Scalp hair, beard, moustache, and in hirsute individual′s short hairs of the thighs, trunk, and perianal area may be involved. [1]
Pubic lice feed and reproduce on the human host cementing their nits to the hair shaft 1 cm from the skin surface and nits hatch in 8 to 10 days. [1] Pubic lice can sometimes be macroscopically identified with the naked eye and with a magnifying lens. [1] The diagnosis is confirmed by microscopic examination of the plucked hair to identify the nits with vital nymphs and hatched empty cases. [1] Lice are difficult but possible to see with close inspection or magnification. Additionally, dermoscopy allows us to differentiate nits with vital nymphs from empty cases and to identify pubic lice. [2]
A 28-year-old unmarried male presented with small dark colored spots over the lower leg and thighs, noticed since the past 8 days. The spots were moderately itchy. He had no significant medical history. On examination, the patient had multiple small brown colored "papules" located on the lower legs, thighs, and buttocks [Figure - 1]. The examining resident made an initial diagnosis of "eruptive" nevi. However, in view of the history of itching, a closer examination of the lesions was made through a magnifying lens, when it was noticed that some of the lesions were slightly mobile. This was confirmed when a noncontact digital dermoscope was used at magnification of both 10× and 200×, when the complete picture of active pubic louse emerged [Figure - 2].
 |
| Figure 1: Pigmented scratch papules seen in groins |
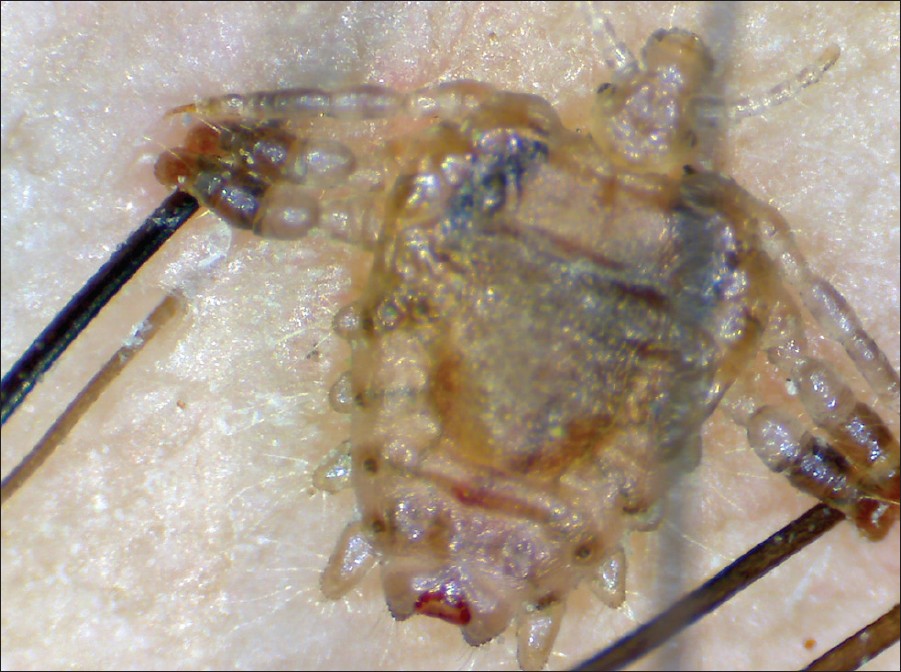 |
| Figure 2: Phthirus pubis seen under 200× magnification |
Dermoscopy of affected hair showed nits containing unhatched nymphs and translucent empty cases [Figure - 3]. Alive and moving lice were seen in PP performing digital dermoscopy in real-time projection on the monitor. [2] Treatment with permethrin 1% shampoo was done in two cycles for 3 weeks, along with nit removal. The response to treatment was good. At control visit the patient was free from any symptoms and no nits or lice were observed.
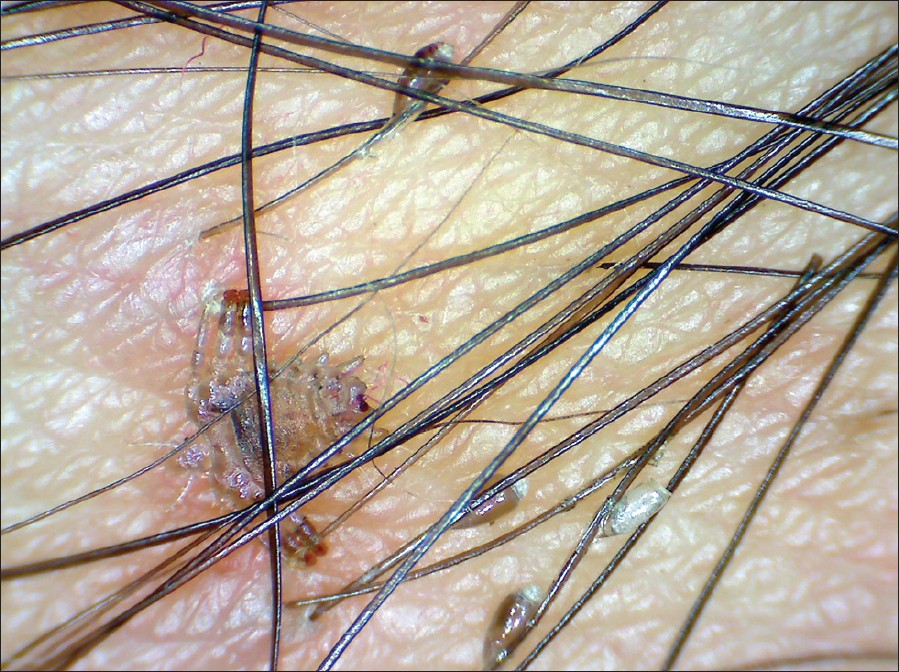 |
| Figure 3: Viable and empty nits seen glued on the hair shaft |
Dermoscopy is a noninvasive technique used in the evaluation of pigmented skin and nonpigmented skin lesions, particularly for the early detections of melanoma. [3] Furthermore, it is also employed as an adjunct to clinical examination in general dermatology. [4] "Entodermoscopy" is a new term employed for dermoscopy of skin infections and infestations, recently introduced by Zalaudek et al. [5] In our case, dermoscopy with a noncontact dermoscope enabled us to establish a rapid diagnosis visualizing unhatched and hatched nits and lice, and also treatment follow-up. Therefore, in vivo dermoscopy is a safe, reliable, and simple method in diagnosing treatment and monitoring of PP that can be used in daily routine.
| 1. |
Chosidow O. Scabies and pediculosis. Lancet 2000;355:819-26.
[Google Scholar]
|
| 2. |
Chuh A, Lee A, Wong W, Ooi C, Zawar V. Diagnosis of pediculosis pubis: A novel application of digital epiluminescence dermatoscopy. J Eur Acad Dermatol Venereol 2007;21:837-8.
[Google Scholar]
|
| 3. |
Argenziano G, Soyer HP, Chimenti S, Talamini R, Corona R, Sera F, et al. Dermoscopy of pigmented skin lesions: Results of a consensus meeting via the Internet. J Am Acad Dermatol 2003;48:679-93.
[Google Scholar]
|
| 4. |
Zalaudek I, Argenziano G, Di Stefani A, Ferrara G, Marghoob AA, Hofmann-Wellenhof R, et al. Dermoscopy in general dermatology. Dermatology 2006;212:7-18.
[Google Scholar]
|
| 5. |
Zalaudek I, Giacomel J, Cabo H, Di Stefani A, Ferrara G, Hofmann-Wellenhof R, et al. Entodermoscopy: A new tool for diagnosing skin infections and infestations. Dermatology 2008;216(1):14- 23.
[Google Scholar]
|
Fulltext Views
3,197
PDF downloads
2,514





