Translate this page into:
Yellowish face mask in a child: A local side-effect of inhaled corticosteroids?
Correspondence Address:
Adone Baroni
Deparment of Dermatology and Venereology, Second University of Naples, c/o II Policlinico, Edificio 3, uarto piano, Via Pansini, Napoli
Italy
| How to cite this article: Baroni A, Piccolo V, Russo T. Yellowish face mask in a child: A local side-effect of inhaled corticosteroids?. Indian J Dermatol Venereol Leprol 2012;78:666 |
Sir,
Inhaled corticosteroids (ICS) are considered the therapy of choice for asthma, maximizing local effects in airways, reducing systemic exposure, and minimizing side effects. [1] Nevertheless, systemic exposure and unperceived deposit of aerosolized drugs on the face and into the eyes could explain several side effects. [2]
A Caucasian 7-year-old girl presented with a 2-week-history of yellow-brown pigmentation, affecting perioral region, nose, and part of chin, progressively changing its color from bluish-red to a greenish-yellow [Figure - 1]. A light tenderness was present. No similar lesions had appeared in this or in other areas since then.
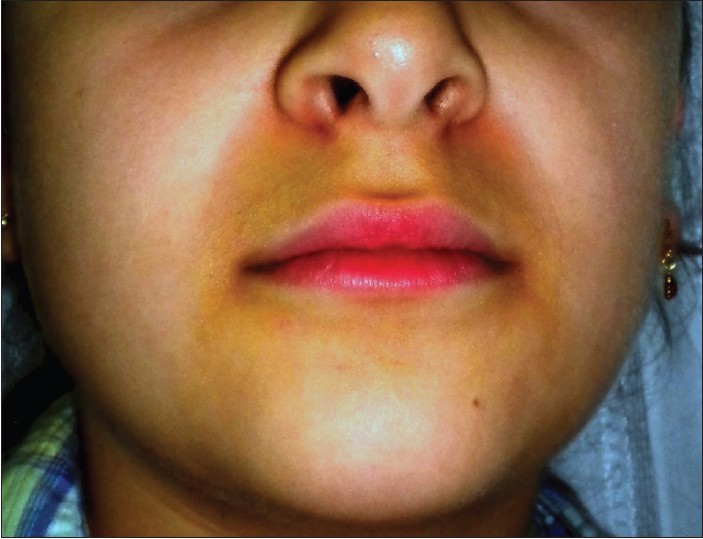 |
| Figure 1: Perioral yellow-brown pigmentation |
Clinical aspect and history given by parents supported the diagnosis of skin bruise, but no trauma or apparent causes were referred. Routine laboratory examinations, coagulation, transaminases, cortisol, adrenocorticotrophic hormone, and electrolytes were unremarkable, permitting us to exclude possible bleeding disorders, hereditary diseases, liver diseases, adrenal disease, and malnutrition that could explain the easy bruising.
Nevertheless, an accurate medical history revealed that the patient was affected by a severe form of asthma and had been administered high dosages of inhaled beclometasone dipropionate (400 mcg twice daily) delivered with an aerosol facemask since a few weeks before the appearance of perioral bruise.
Based on clinical and related findings, and on the relationship with drug administration, a diagnosis of skin bruise induced by cutaneous absorption of ICS was made.
Other causes of perioral discoloration were considered in differential diagnosis as perioral dermatitis (PD), lip-licking cheilitis (LLC), perioral acanthosis nigricans (PAN), and glucocorticosteroids-induced hyperpigmentation (GIH). [3] PD is an inflammatory and chronic papulopustular and vesicular facial dermatitis, often related to the misuse of potent corticosteroids. It could leave a mild hyperpigmentation of the affected area, but the lack of the inflammatory phase preceding the pigmentation permitted us to rule out PD. LLC is common in childhood, but it is characterized by scale and well-demarcated borders and induced by the habit of children to compulsively lick lips, absent in our case. PAN was ruled out because of the absence of roughness of pigmentation, the negativity of metabolic investigations, and the absence of lesions in typical locations of the disease. GIH was another possible cause of perioral pigmentation, but the contusiform evolution of the discoloration gave us the possibility to exclude it.
Subsequently, the child was taught to use mouthpiece device, and, after two weeks, perioral discoloration had completely disappeared and no other lesions occurred.
Easy bruising is a systemic ICS side effect and can be simply defined as "bruising resulting from a slight knock or without apparent cause." [4] The risk of this adverse reaction is more important among the elderly and increase with daily dosage and duration of treatment. It is probably present in about 50% of patients treated with ICS, presenting as purpuric or ecchymotic lesions occurring on the face, the limbs, or the neck, although neither the true incidence in children nor the dosage and duration of therapy at which it appears are known. [1] Easy bruising can also occur in Cushing′s disease, bleeding disease, and collagen-related syndromes such as Ehlers-Danlos. [4]
Hypertrichosis as a side effect of inhaled steroids has been reported in children. [5]
Bruising is probably dependent on collagen synthesis modification. Reduced production of structural proteins by fibroblasts, loss of dermal ground substance, and reduced keratinocyte mitosis lead to thinning of the skin, and changes in dermal endothelium can produce telangiectasias. The persistent vasodilatation and the loss of supporting matrix induced by steroids may dispose to bruising. [2]
Although facial bruise could be in theory as the result of systemic or local adsorption of drug, we suppose that, in our case, skin changes are not related to systemic exposure to ICS because of the limited area of involvement, the normal adrenal function, and the appearance after the use of an aerosol facemask. We consider the unintentional direct skin deposition of aerosol as the cause of this bruise.
Very young children are incapable to use mouthpiece interfaces; therefore, they use a mask attached to either a nebulizer or a valved holding chamber. With these devices, there can be a significant deposition of aerosol on the face and eyes, while the risk seems to be negligible in children assuming ICS with a mouthpiece interface. [2]
To the best of our knowledge, our case represents the first report of perioral bruising induced by ICS. In conclusion, when easy bruising is associated with other systemic side effects, as adrenocortical suppression or increased bone metabolism, further investigations are necessary because it could be a visible marker of a significant systemic absorption of ICS, especially in elderly patients. Moreover, since it is not know if there are effects from topical facial aerosol deposition, and considering our case as an example, we think that it would be prudent to take measures to avoid facial exposure from ICS, and to wean the dose of ICS to the minimal effective dose.
| 1. |
Guillot B. Skin reactions to inhaled corticosteroids. Clinical aspects, incidence, avoidance, and management. Am J Clin Dermatol 2000;1:107-11.
[Google Scholar]
|
| 2. |
Geller DE. Clinical side effects during aerosol therapy: Cutaneous and ocular effects. J Aerosol Med 2007;20:S100-8; discussion S109.
[Google Scholar]
|
| 3. |
Lipozencic J, Ljubojevic S. Perioral dermatitis. Clin Dermatol 2011;29:157-61.
[Google Scholar]
|
| 4. |
Mak VH, Melchor R, Spiro SG. Easy bruising as a side-effect of inhaled corticosteroids. Eur Respir J 1992;5:1068-74.
[Google Scholar]
|
| 5. |
De Vries TW, de Langen-Wouterse JJ, de Jong-Van den Berg LT, Duiverman EJ. Hypertrichosis as a side effect of inhaled steroids in children. Pediatr Pulmonol 2007;42:370-3.
[Google Scholar]
|
Fulltext Views
6,168
PDF downloads
2,246





