Translate this page into:
A severe case of universal calcinosis with juvenile dermatomyositis
2 Department of Neuromuscular, the Third Hospital of Hebei Medical University, Shijiazhuang, China
Correspondence Address:
Liu Ya-ling
Department of Dermatology, the Third Hospital of Hebei Medical University, Shijiazhuang 050051
China
| How to cite this article: Ya-ling L, Jing H, Qian L. A severe case of universal calcinosis with juvenile dermatomyositis. Indian J Dermatol Venereol Leprol 2012;78:774 |
Sir,
Juvenile dermatomyositis (JDM) is a multisystem disease characterized by characteristic rash and symmetric proximal muscle weakness. Its diagnosis is mainly confirmed by muscle biopsy. The typical histopathologic features on muscle biopsy of JDM are perifascicular atrophy and inflammatory cell infiltration, especially around small blood vessels. Calcinosis, often reported as the initial complaint, occurs three times more frequent in JDM than in adult-onset dermatomyositis, with incidence of 30 to 40%. [1] Cutaneous calcifications are often located on the extensor aspect of joints and other acral parts, leading to severe pain, muscle atrophy, non-healing skin ulcers, and joint contractures. [2] We present a case of JDM whose muscle biopsy demonstrated an uncommon feature and who developed extensive calcinosis cutis.
A 16-month-old girl was admitted with elevated myocardial enzymes for four months in March 2009. Four months prior to admission, the patient had a cold and went through a course of elevated creatine kinase (CK) fluctuating from 400 to 1000 U/L. During that time, her electrocardiogram revealed sinus tachycardia. She was diagnosed with myocarditis in a local hospital. Gradually, she manifested decreased activity of the limbs and could not walk independently. Family history was negative for similar muscle disorder. Physical examination revealed no obvious rashes. Neurologic examination showed reduced muscle strength with grade 4/5 in the neck and limb. Reduced tendon reflexes and muscle tension especially of the limbs were observed as well. Her CK was elevated to 498 U/L (normal: 65 to 130 U/L), lactate dehydrogenase (LDH) was 382 U/L (normal: 76 to 200 U/L), aspartate aminotransferase (AST) was 83 U/L, and electromyographic pattern indicated myopathy. Muscle biopsy revealed typical perifascicular atrophy and inflammatory cells around the vessels, which are diagnostic symptoms for DM. However, the presence of prominent vacuoles similar to that seen in glycogen storage disease (GSD) within the cytoplasm of myofibers [Figure - 1] confused the histopathologic diagnosis. Numerous dark-stained fibers and vacuoles were observed in periodic acid-Schiff (PAS) staining. We considered the diagnosis of JDM, but we encountered difficulties in differentiating this condition from GSD type II. Due to inadequate laboratory conditions, lysosomal assay to confirm the diagnosis of GSD type II was not conducted. Aggressive therapy with glucocorticoid or intravenous immunoglobulin was strongly recommended; however, it was not executed because the patient′s parents refused such aggressive treatment for their child.
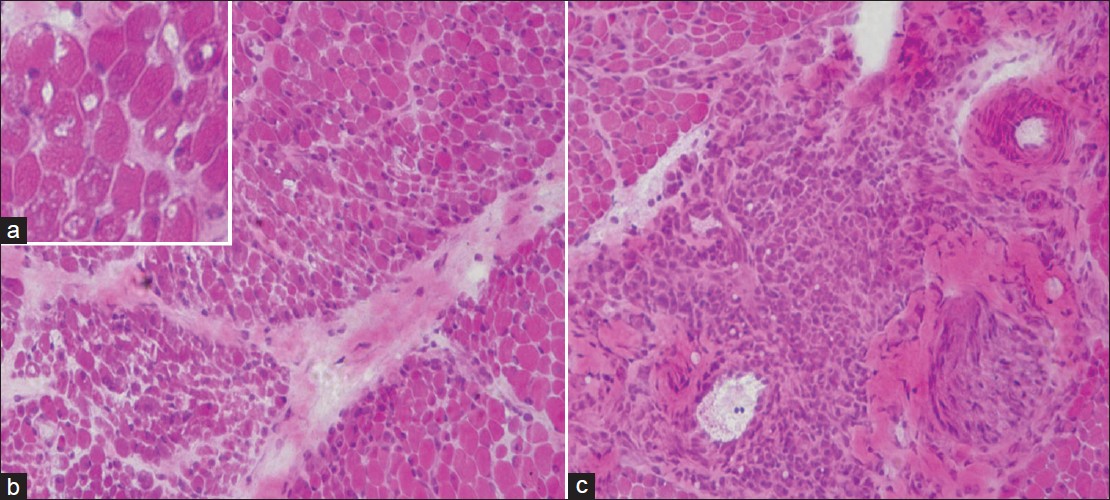 |
| Figure 1: (a) Numerous irregular vacuoles in the cytoplasm of muscle fibers (H and E, ×200) (b) Muscle biopsy showing typical perifascicular atrophy (H and E, ×100). (c) Inflammatory cells that infiltrate muscle tissues and are seen around the small blood vessels (H and E, ×100). |
In September 2011, the patient returned to our department with muscle weakness, joint contracture, hard and painful subcutaneous nodules, and swelling of bilateral buttock. She underwent surgical drainage in January 2010 due to cellulitis of her left thigh. One month later, she developed hard subcutaneous nodules and joint contractures. Half a year later, she experienced skin ulceration and papules around the joints. Physical examination revealed violaceous rashes over the eyelids [Figure - 2]a. Numerous red, hard, mildly tender and peanut-sized subcutaneous nodules were seen on her head [Figure - 2]b, neck, trunk, and extremities [Figure - 2]c. On the extensor surface of her joints, miliary and rock-hard papular rashes were noted [Figure - 2]. Some papules were inflamed with purulent infiltration. Fist-sized subcutaneous swelling was noted on the patient′s bilateral hip characterized by high skin temperature, softness, and tenderness [Figure - 2]e. On her left buttock, there was skin ulceration 1 cm in diameter, with exudates on the surface. Neurological examination was not performed due to joint contractures [Figure - 2]f. Laboratory studies showed an elevated erythrocyte sedimentation rate of 24 mm/h. Blood work up revealed normal levels of calcium, phosphorus and PTH. Radiology [Figure - 3]a and b and computed tomography (CT) [Figure - 3]c and d scan revealed extensive calcium deposits (including the scapular region, spinal column, bilateral hips, abdominal wall, and lower limbs) in subcutaneous tissues, fascia, and muscles. Finally, the patient was diagnosed with severe JDM and universal calcinosis. Differential diagnosis included myositis ossificans, systemic lupus erythematosus, scleroderma, and hyperparathyroidism. The patient started the treatment with 3mg dexamethasone iv daily combined with 5mg Technetium [99TC] methylened phosphonate injection iv daily. Five days later, the subcutaneous nodules were softer. No obvious side effect was observed during treatment, which allowed us to adjust the amount of dexamethasone to 5mg iv daily. Despite the therapy of glucocorticoid and bisphosphonate, a new beaded hard mass appeared on the patient′s sternocostal area and limbs, which was attributed to the primary disease. After two weeks of treatment, the subcutaneous nodules and papules did not exhibit further development.
 |
| Figure 2: (a) Physical examination revealed violaceous rashes over the eyelids. (b, c) Papules on the head and extensor surface of the elbow. Some papules were inflamed with purulent infiltration (arrow). (d) Subcutaneous nodules on the lower limbs. (e) Subcutaneous swelling on bilateral hip. (f) Joint contracture of both knees and hips |
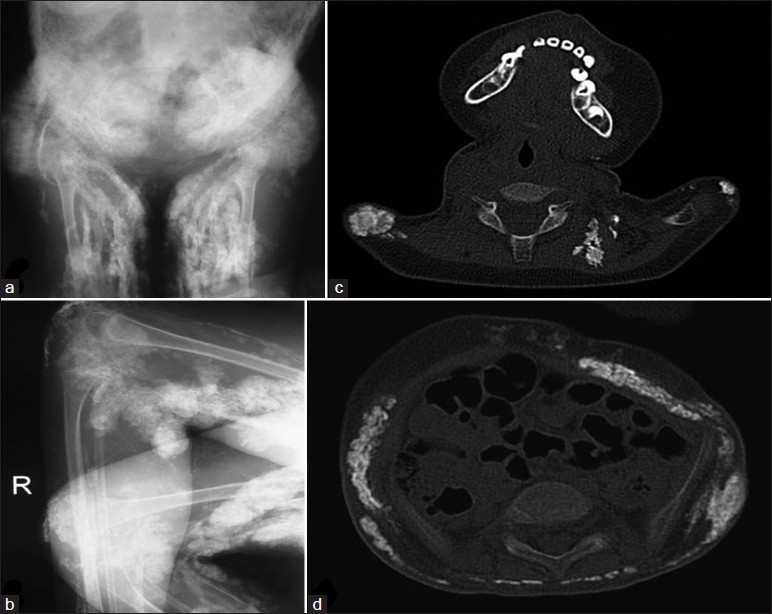 |
| Figure 3: (a, b) Radiograph of bilateral knees and hips showed extensive calcification in the skin, subcutaneous, fascial planes, deeper muscle tissue, and joint contracture. (c, d) CT revealed diffuse calcifications over her entire body, such as in the scapular region and abdominal wall |
JDM, whose pathogenesis remains unclear, is a rare but challenging disease. Although the mechanism of calcinosis in JDM is not fully understood, inflammatory cell cascades, cytokines, and mineralized matrix proteins often lead to injury and inflammation of tissues in JDM. [3] Calcinosis tends to occur more frequently in JDM patients who undergo prolonged inflammatory duration of active disease resulting from delays in diagnosis or inadequate treatment. We believe the following factors caused the patient′s severe calcinosis. First, correct diagnosis was not established promptly. The history of muscle weakness, elevated CK and ESR, myopathic pattern on the electromyogram, and typical perifascicular atrophy and inflammatory cells around the vessels seen on the muscle biopsy all indicated the diagnosis of JDM. However, the absence of skin rashes and the presence of prominent vacuoles in myofibers stainable by HE and PAS made it difficult to differentiate JDM from GSD. Second, the delayed aggressive treatment of glucocorticoid led to persistent inflammation and continued disease activity. Finally, the surgical procedure of drainage itself may have induced the development of calcinosis. In a study in Brazil, cardiac involvement was identified to be independently associated with calcinosis in JDM. [4] We obtained the same finding in our study because our patient had been initially diagnosed with myocarditis based on a four-month history of elevated cardiac enzymes (including CK, LDH, and AST) and sinus tachycardia. This case study emphasizes that delay in diagnosis, as well as late or lack of aggressive treatment in JDM, contributes to the development of calcinosis. Notably, muscle biopsy from JDM patients can present with striking patterns of vacuoles that are similar to those in GSD. The irregular vacuoles in myofibers may be related to ischemia of muscle tissue resulting from inflammatory infiltration around small blood vessels.
Two types of JDM are Brunsting and Banker type. [5] Our case belongs to Banker type because the condition progressed rapidly. As a severe complication of JDM, calcinosis increases morbidity and mortality. The poor functional recovery from JDM is most likely due to calcium deposition. As soon as the diagnosis of JDM is made, early and appropriate treatment should be started right away, such as high-dose corticosteroids, intravenous immunoglobulin, cyclophosphamide, or methotrexate. [6] These treatments can control the progression of the disease and prevent the development of calcinosis. Once the calcification is formed, unfortunately, it is difficult to manage.
| 1. |
Wananukul S, Pongprasit P, Wattanakrai P. Calcinosis cutis presenting years before other clinical manifestations of juvenile dermatomyositis: Report of two cases. Australas J Dermatol 1997;38:202-5.
[Google Scholar]
|
| 2. |
Yun SJ, Lee JB, Kim SJ, Lee SC, Won YH, Kang HC. Calcinosis cutis universalis with joint contractures complicating juvenile dermatomyositis. Dermatology 2006;212:401-3.
[Google Scholar]
|
| 3. |
Rider LG. Calcinosis in juvenile dermatomyositis: Pathogenesis and current therapies. Pediatr Rheumatol Online J 2003;1:119-33.
[Google Scholar]
|
| 4. |
Sallum AM, Pivato FC, Doria-Filho U, Aikawa NE, Liphaus BL, Marie SK, et al. Risk factors associated with calcinosis of juvenile dermatomyositis. J Pediatr (Rio J) 2008;84:68-74.
[Google Scholar]
|
| 5. |
Mustapha MG, Ashir MG, Mayun AA, Machoco Y, Ibrahim AB. Juvenile dermatomyositis in a Nigerian girl: A case report. Niger J Paediatr 2011;38:182-5.
[Google Scholar]
|
| 6. |
Jiang X, Yi Q, Liu D, Wang S, Li L. A case of juvenile dermatomyositis with severe calcinosis and successful treatment with prednisone and diltiazem. Int J Dermatol 2011;50:74-7.
[Google Scholar]
|
Fulltext Views
1,740
PDF downloads
2,077





