Translate this page into:
A case of facial keratosis follicularis squamosa resembling atrophic acne scarring, successfully treated with topical pimecrolimus
Correspondence Address:
Yan Lu
Department of Dermatology, 1st Affiliated Hospital, Nanjing Medical University, #300 Guangzhou Rd., Nanjing, Jiangsu Pr.- 210 029
China
| How to cite this article: Lu Y, Zhang MH, Zhu WY. A case of facial keratosis follicularis squamosa resembling atrophic acne scarring, successfully treated with topical pimecrolimus. Indian J Dermatol Venereol Leprol 2011;77:69-70 |
Sir,
Keratosis follicular squamosa (KFS), first reported by Dohi and Momose [1] in 1903, is a separate clinical entity from keratosis follicularis, Darier′s disease. It appears clinically as scaly patches, 3-10 mm in diameter, with brownish follicular plugs in the center. The margins of the patches, slightly raised from the underlying epidermis, are seen like "lotus leaves on the water". The most commonly affected sites are the abdomen, thighs, buttocks and waist. [2] Here we describe a rare case of KFS which occurred on the face and resembled atrophic acne scarring in clinical features, and it is the first report of facial case with unique manifestation to our knowledge, and furthermore, we achieved satisfying therapeutic results with pimecrolimus cream 1%.
A 32-year-old woman presented with an over 6-year history of asymptomatic atrophic acne scars like lesions scattered on the face. There was no family history of a similar disease. Her medical history was unremarkable and she had no history of acne or other facial problem. She had no habit of using cosmetics before and after the lesions appeared. Physical examination revealed numerous small, atrophic acne scars like eruptions, some of which were scaly depressed patches whose margins were slightly detached from the underlying epidermis. Some lesions had a tiny brownish follicular plug, seen as a black dot, in the center [Figure - 1]. A KOH preparation from the scale was negative. Bacterial culture of the lesion resulted in tiny colonies of Staphylococcus epidermidis, which is a normal skin commensal. Laboratory and endocrinological examination showed no abnormalities with regard to liver and renal function tests and hormones detection. Skin biopsy demonstrated dilated follicles with keratotic plugs and orthohyperkeratosis. Lateral margin of the scale was slightly detached from the granular layer [Figure - 2]. Based on these features, we diagnosed these lesions as facial keratosis follicularis squamosa. Then, the patient began to use topically pimecrolimus cream 1% (Elidel, Novartis, CH-4002 Basel, Switzerland) once daily. The lesions notably improved after 2 weeks. There was nearly complete resolution of those atrophic acne scars like lesions and follicle plugs at the end of the 4 th week [Figure - 3]. Only some yellow or light-brown pigmentation was left on the forehead.
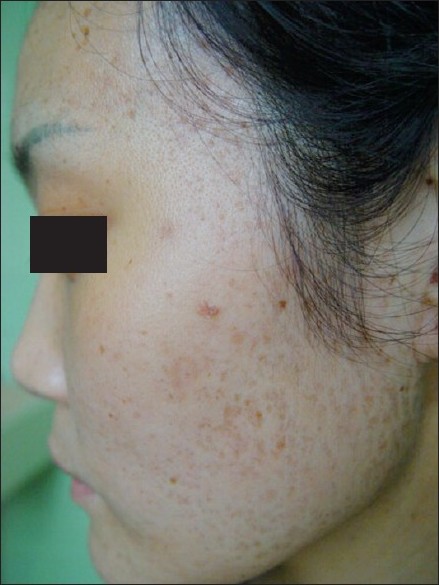 |
| Figure 1 :Clinical appearance before treatment. Atrophic acne scars like lesions, with a tiny brownish follicular plug in the center |
 |
| Figure 2 :Skin biopsy revealed dilated follicles with keratotic plugs and orthohyperkeratosis. Lateral margin of the scale is slightly detached from the granular layer (H and E, ×10) |
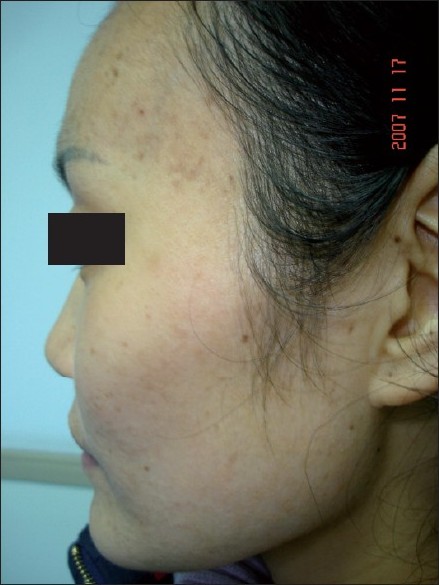 |
| Figure 3 :Clinical appearance after treatment. Most of atrophic acne scars like eruptions and follicular plugs were resolved |
KFS is actually not rare in China, although it is not yet described in the English literature. This is not a typical KFS as previously reported and should be differentiated from atrophic scars of acne and keratosis pilaris. As she had no history of acne occurrence in the past and atrophic lesions could not disappear by themselves, the former dermatosis can easily be excluded. Keratosis pilaris and keratosis follicularis squamosa share the histological finding of keratotic plugging; however, the KFS lesion is usually clinically and histologically surrounded by fine lamellar scales, while typical eruption of keratosis pilaris looks like a horny papule, rather than a black dot as seen in KFS. [3] Additionally, the genetic contribution in KFS is smaller than in keratosis pilaris. Bacterial infection, irritation by clothing, heredity and hormone imbalance have been proposed as pathogenetic factors for KFS, but our patients had no indications of the above possibilities.
Traditionally, oral antibiotics, such as minocycline and roxithromycn, and topical exfoliative agents have been used for the treatment of KFS. [4] Sadahira et al. reported a case successfully treated with topical tacalcitol. [5] We chose pimecrolimus to treat the patient and the lesions were markedly improved after the therapy. Pimecrolimus (SDZ ASM 981), an ascomycin derivative and calcineurin inhibitor, is a nonsteroid, has anti-inflammatory activity, and has demonstrated efficacy in reducing symptoms of atopic dermatitis in adult and pediatric patients when applied topically. It binds cytoplasmic proteins and the resulting complex binds calcineurin, inhibiting its ability to dephosphorylate the nuclear factor of activated T cells, thus suppressing gene transcription. [6] Rubeqni et al. reported a case of extensive Darier′s disease successfully treated with topical tacrolimus, after stopping of oral isotretrinoin due to major depression. [7] However, the mechanism of calcineurin inhibitor to treat hyperkeratotic skin disorders remains unclear. We have been following the patient for 6 months with no recurrence.
| 1. |
Dohi K, Momose G. A presentation of patients with a certain follicular squamous keratosis (in Japanese). Jpn J Dermatol 1903;3:513-4.
[Google Scholar]
|
| 2. |
Tamiya H, Tsuruta D, Umeda R, Kobayashi H, Ishii M. Keratosis follicularis squamosa (Dohi) associated with pseudoacanthosis nigricans. Br J Dermatol 2004;150:603-5.
[Google Scholar]
|
| 3. |
Shimizu S, Shimizu T, Tateishi Y, Shimizu H. Keratosis follicularis squamosa (Dohi): A follicular keratotic disorder well known in Japan. Br J Deramtol 2001;144:1070-2.
[Google Scholar]
|
| 4. |
Nomura Y, Abe M, Natsuga K, Moriuchi R, Kawasaki H, Mayuzumi M, et al. Widespread keratosis follicularis squamosa. Clin Exp Dermatol 2009;34:519-20.
[Google Scholar]
|
| 5. |
Sadahira C, Yoneda K, Moriue T, Katsuura J, Kobota Y. Successful treatment of keratosis follicularis squamosa with topical tacalcitol. Br J Dermatol 2006;154:1010-2.
[Google Scholar]
|
| 6. |
Wellington K, Jarvis B. Topical pimecrolimus: A review of its clinical potential in the management of atopic dermatitis. Drugs 2002;62:817-40.
[Google Scholar]
|
| 7. |
Rubeqni P, Poqqiali S, Sbano P, Risulo M, Fimiani M. A case of Darier's disease successfully treated with topical tacrolimus. J Eur Acad Dermatol Venereol 2006;20:84-7.
[Google Scholar]
|
Fulltext Views
5,526
PDF downloads
2,650





