Translate this page into:
Cutaneous findings in five cases of malaria
Correspondence Address:
Jignesh B Vaishnani
Department of Dermatology, Room No 10, Surat Municipal Institute of Medical Education and Research Hospital, Opp. Bombay Market, Umarwada, Surat - 395 010, Gujarat
India
| How to cite this article: Vaishnani JB. Cutaneous findings in five cases of malaria. Indian J Dermatol Venereol Leprol 2011;77:110 |
Abstract
Malaria is an infectious disease caused by protozoa of the genus Plasmodium. Cutaneous lesions in malaria are rarely reported and include urticaria, angioedema, petechiae, purpura, and disseminated intravascular coagulation (DIC). Here, five malaria cases associated with cutaneous lesions have been described. Out of the five cases of malaria, two were associated with urticaria and angioedema, one case was associated with urticaria, and other two were associated with reticulated blotchy erythema with petechiae. Most of the cutaneous lesions in malaria were nonspecific and reflected the different immunopathological mechanism in malarial infection.Introduction
Malaria is an infectious disease caused by protozoa of the genus Plasmodium, characterized by fever with rigor, headache, anemia and splenomegaly. Complicated malaria is characterized by severe anemia, thrombocytopenia, pulmonary edema, hypoglycemia, hypotension, encephalopathy and death. Cutaneous lesions in malaria are rarely reported and include urticaria, angioedema, petechiae, purpura, and disseminated intravascular coagulation (DIC). [1],[2],[3] Here, five malaria cases associated with cutaneous lesions have been reported.
Case Reports
Case 1
A 16-year-old adolescent male presented with skin rash of 2 days duration. He had history of fever without rigor. Cutaneous examination revealed multiple discrete erythematous and edematous papular skin lesions involving face, trunk, and proximal part of limbs [Figure - 1]. Lesions were mildly itchy. There was no mucosal lesion and no history of drug in last 3 weeks. On investigation, blood count, hemogram and liver function were within normal range. Peripheral smear showed trophozoites of Plasmodium vivax. The patient was treated with chloroquine along with antihistamine. Rash disappeared completely on the third day of starting anti-malarial and anti-histamine. The patient had been given primaquine for 14 days for radical cure.
 |
| Figure 1: Multiple discrete urticarial lesions on trunk |
Case 2
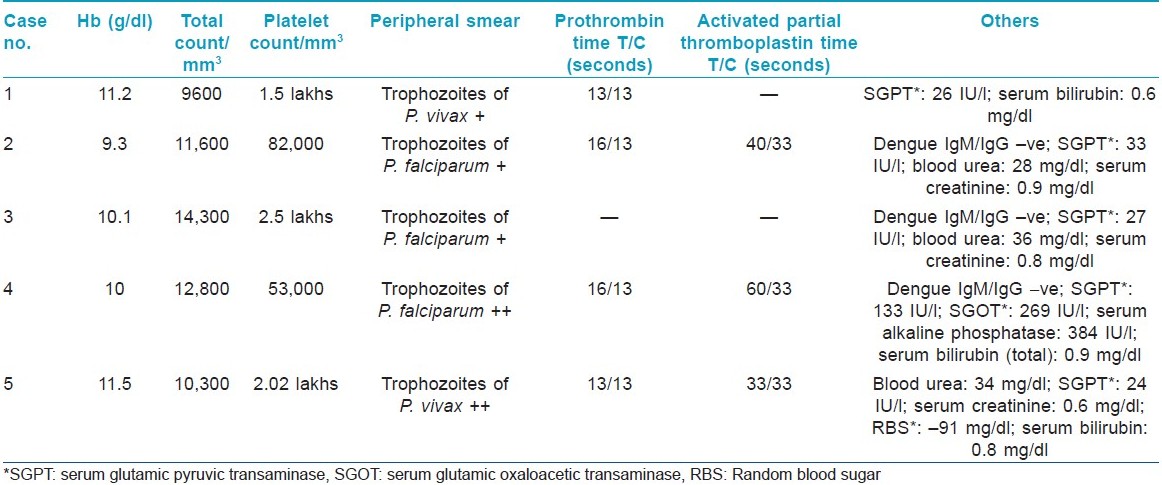
A 19-year-old male was admitted with history of high-grade fever, chills and skin rash. There was history of generalized weakness, giddiness, headache, and dry cough, but no history of hematemesis, hemoptysis, melena, or joint pain. Examination revealed asymptomatic blotchy reticulate erythema with petechiae involving upper and lower limbs sparing palms, soles, trunk and face. There was redness of conjunctiva, but oral mucosa was found to be normal. The patient had tachycardia with fever (100.4°F) and postural hypotension (supine and sitting were 112/76 and 84/60 mm Hg, respectively). Details of investigations are given in [Table - 1]. Peripheral smear showed trophozoites of Plasmodium falciparum (2+). He was given parenteral α-β arteether, quinine, platelet concentrate and intravenous fluids. Rash started resolving on the third day of starting treatment with anti-malarial and disappeared completely on the ninth day of treatment.
Case 3
A 43-year-old female was admitted with severely itchy erythematous and edematous skin lesions, with swelling of eyelids and lips of 1 day duration. There was history of fever with rigor and giddiness. On examination, she had urticaria involving trunk, limbs and face with angioedema of both upper eyelids. Temperature (oral) was 99.8°F, with tachycardia and hypotension (86/60 mm Hg). Peripheral smear showed trophozoites of P. falciparum. Details of investigations are given in [Table - 1]. The patient was treated with parenteral dexamethasone and chlorpheneramine maleate along with injection α-β arteether and IV fluids. Urticaria and angioedema disappeared on the second day and systemic steroids were discontinued. The patient was given oral antihistamine (cetirizine) for 5 days. Urticaria did not recur after discontinuation of antihistamine.
Case 4
A 6-year-old female child presented with skin rash over limbs with history of fever with rigor and generalized weakness of 2 days duration. On examination, the patient had diffuse non-itchy, blotchy reticulate erythema with petechiae involving both upper and lower limbs, sparing palms, soles and face [Figure - 2]. Mucosa was normal. Mild hepatosplenomegaly was found on systemic examination. Details of investigations are presented in [Table - 1]. The patient was treated with parenteral α-β arteether, platelet concentrates and IV fluids. Rashes started resolving on the second day and disappeared completely on the seventh day of starting anti-malarial treatment.
 |
| Figure 2: Diffuse reticulate erythema and petechiae with edema of fingers |
Case 5
A 17-year-old male presented with fever, headache, generalized weakness and skin rash of 2 days duration. On examination, the patient had fever (temperature: 99.8°F) and hypotension (blood pressure 90/58 mm Hg). Cutaneous examination revealed swelling of lips and eyelids and multiple urticarial skin lesions over face, trunk and limbs. On finding trophozoites of P. vivax on peripheral smear, the patient was treated with injectable chloroquine and one dose of intravenous dexamethasone 8 mg and chlorpheneramine maleate 12.5 mg. Rash disappeared on the second day and the patient was given oral anti-histamine (cetirizine). After the full course of chloroquine, the patient was given primaquine for 14 days for radical cure.
Discussion
Malaria is a major public health problem in India. Both P. falciparum malaria and P. vivax malaria can present with urticaria, angioedema, petechiae and purpura. [1],[2],[3] Exact pathogenesis of skin rash in malaria not known, but these may reflect part of different immunological consequences during malarial infection.
Mast cells [4] play a central role in pathophysiology of malaria. Many features of malarial pathology [5] like increased expression of endothelial adhesion molecules (ICAM-1, VCAM-1, E-selectin), increased vascular permeability and vasodilatation are mediated by mast cell mediators like histamine, serotonin, heparin, proteoglycans, certain proteases, prostaglandins, leukotrienes, platelet activating factor and cytokines [tumor necrosis factor (TNF)]. Histamine [6],[7] is produced during all stages of infection with plasmodia, and pattern of histamine release may differ in different individuals. Platelet activating factor (PAF) [7],[8] causes aggregation of human platelets, wheal and flare response with late phase erythema. Leukotriene (LTC 4, LTD4, LTE 4) [7],[8] induced wheal-flare response is long lasting and associated with endothelial activation and up-regulation of adhesion molecules.
Precise mechanism of mast cell activation in malaria is not known. There can be multiple mechanisms that activate the mast cell.
Anti-malarial IgE antibody [9] is usually found in individuals from high endemic areas and can have both protective and pathogenic roles. IgE binds to high affinity FceRI receptors expressed on mast cells, and malarial antigen cross linking of FcεRI induces activation of mast cell and release of mediators. Besides anti-malarial IgE antibody, IgG [10] anti-malarial antibody is also found to be protective against malarial infection. IgG binds to FcγRI receptors expressed on human mast cell, and antigen cross linking leads to mast cell activation and release of mediators.
As skin mast cells alone express CD88, the receptor for anaphyltoxin C5a, allowing them to be activated in complement-mediated disease. It has been shown that malaria product (P. falciparum glycosylphosphatidylinositol) potentiates cytokine secretion through C5a. [11]
Both IgG and IgE containing immune complexes [12] (Ics) are elevated in malaria and probably play a role in pathogenesis. IgE containing Ics are associated with complicated malarial infection. Deposition of such Ics in cutaneous vessels may result in local vasculitic damage and skin lesions.
Most of the cutaneous lesions in malaria are not specific. But when associated with systemic features, one must carefully evaluate the condition including peripheral smear that may help to clench the diagnosis of malaria. In the cases presented here, skin lesions associated with malaria reflect the different immunopathological mechanisms in malarial infection. Urticaria and erythema are usually due to histamine and/or other mediators like PAF and leukotrienes. Purpura and petechiae may be a result of cytoadherance, local vasculitis and vessel damage from immune complex injury.
| 1. |
Singh RP, Mittal SP, Narayanan VA, Shetty KJ. Occurrence of urticaria as a manifestation of Falciparum malaria. J Assoc Physicians India 1988;36:261-2.
[Google Scholar]
|
| 2. |
Maheshwari N, Maheshwari V, Mobashir M. Plasmodium vivax malaria presenting with urticaria (letter). Postgrad Med J 1989;65:266-7.
[Google Scholar]
|
| 3. |
Khaira A, Gupta V, Mahajan S, Bhowmik D, Tiwari SC. Purpura fulminans in a complicated Falciparum malaria. J Assoc Physicians India 2008;56:467-9.
[Google Scholar]
|
| 4. |
Furuta T, Kikuchi T, Iwakura Y, Watanabe N. Protective roles of mast cells and mast cell-derived TNF in murine malaria. J Immunol 2006;177:3294-302.
[Google Scholar]
|
| 5. |
Lee KH, Kim JY, Kang DS, Choi YJ, Lee WJ, Ro JY. Increased expression of endothelial cell adhesion molecules due to mediator release from human foreskin mast cells stimulated by antibodies in chronic urticaria sera. J Invest Dermatol 2002;118:658-63.
[Google Scholar]
|
| 6. |
Enwonwu CO, Afolabi BM, Salako LO, Idigbe EO, Bashirelah N. Increased plasma levels of histidine and histamine in falciparum malaria: Relevance to severity of infection. J Neural Transm 2000;107:1273-87.
[Google Scholar]
|
| 7. |
Steinhoff M, Griffiths CE, Church MK, Luyer TA. "Inflammation"- mediators of inflammation. In: Burn T, Breathnach S, Cox N, Griffith C, editors. Rook's TB of dermatology. 7 th ed. Massachusetts USA: Blackwell Science; 2004. p. 9.1-67.
th ed. Massachusetts USA: Blackwell Science; 2004. p. 9.1-67.'>[Google Scholar]
|
| 8. |
Wasserman SI. Biological mediators of allergic reaction. In: Grammar LC, Greenberger PA, editors. Pattorsons allergic disease. 6 th ed. Philadelphia USA: Lippincort William and Wilkins; 2002. p. 55-63.
[Google Scholar]
|
| 9. |
Yamaguchi M, Sayama K, Yano K, Lantz CS, Noben-Trauth N, Ra C, et al. IgE enhances Fcå receptor I expression and IgE-dependent release of histamine and lipid mediators from human umbilical cord blood-derived mast cells: Synergistic effect of IL-4 and IgE on human mast cell Fcε receptor I expression and mediator release. J Immunol 1999;162:5455-65.
[Google Scholar]
|
| 10. |
Tangteerawatana P, Montgomery SM, Perlmann H, Looareesuwan S, Troye-Blomberg M, Khusmith S. Differential regulation of IgG subclasses and IgE antimalarial antibody response in complicated and uncomplicated plasmodium malaria. Parasite Immunol 2007;29:475-83.
[Google Scholar]
|
| 11. |
Patel SN, Berghout J, Lovegrove FE, Ayi K, Conroy A, Serghides L, et al. C5 deficiency and C5a or C5aR blockade protects against cerebral malaria. J Exp Med 2008;205:1133-43.
[Google Scholar]
|
| 12. |
Mibei EK, Otieno WO, Orago AS, Stoute JA. Distinct pattern of class and subclass antibodies in immune complexes of children with cerebral malaria and severe malarial anaemia. Parasite Immunol 2008;30:334-41.
[Google Scholar]
|
Fulltext Views
13,005
PDF downloads
3,086





