Translate this page into:
A measurement of the stigma among vitiligo and psoriasis patients in India
Correspondence Address:
Premkumar Ramaswamy
Schieffelin Institute of Health-Research and Leprosy Centre, Karigiri-632 106, Dist-Vellore, Tamil Nadu
India
| How to cite this article: Pichaimuthu R, Ramaswamy P, Bikash K, Joseph R. A measurement of the stigma among vitiligo and psoriasis patients in India. Indian J Dermatol Venereol Leprol 2011;77:300-306 |
Abstract
Background and Aim: The aim is to measure and to compare the level of social participation experienced by vitiligo and psoriasis patients in their domestic and social life in an Indian context. Methods: A cross-sectional comparative study with a sample of 150 cases each of psoriasis and vitiligo, a total of 300 subjects. A detailed clinical assessment of these two conditions, including the extent of lesions on the affected body parts, socioeconomic status and participation levels in social and domestic lives, was done. Results: The result showed that, 17.3% of vitiligo patients participated minimally in domestic and social life, whereas 28% of psoriasis patients had this problem (P=0.027). Extreme participation restriction was observed only among psoriasis patients (2.7%). Psoriasis patients also faced significantly more restrictions in a number of day-to-day life situations such as, less confidence in learning and applying knowledge, difficulties in meaningfully participating in major life areas like, work, education and employment, and also in community, social and civic life (all three domains P<0.0001), to vitiligo patients. Conclusion: Both psoriasis and vitiligo patients suffered moderate to severe restriction while participating in their domestic and social life. Of these two groups, psoriasis patients faced significantly more restrictions in a number of day-to-day life situations. The Indian population of this study was predominantly dark-skinned and hypo-pigmentation as seen in vitiligo is much more noticeable than psoriatic red patches. However, the results showed that the component of hypo or hyperpigmentation of the skin is not the only factor leading to participation restrictions.Introduction
Vitiligo and psoriasis are cosmetically disfiguring conditions that are commonly seen in Indian dermatological outpatients′ clinics. Psoriasis goes further than this with systemic association of arthritis. The real prevalence of these conditions still remains unknown, as no epidemiological surveys have been conducted so far. However, calculated from the dermatological outpatients′ records the prevalence of vitiligo ranges between 3 and 4% globally, with Mexico and India having the highest incidence of this condition. [1] Similar estimates with psoriasis suggest its prevalence ranging between 0.8 and 5.6%. [2]
Earlier studies on the psychosocial aspects have shown that vitiligo may have a profound impact on self-image, self-esteem and interpersonal relationships. [3] In addition, the patient can experience stigmatization, embarrassment and self-consciousness about vitiligo. [4] There were more such studies on psoriasis than vitiligo, for example on the aspect of social stigma due to psoriasis [5],[6],[7],[8],[9],[10],[11],[12] and on establishing social relationships. [12] There were also four studies comparing the psychosocial aspects in psoriasis and vitiligo. [13],[14],[15],[16] The first three studies were on the psychiatric morbidity of these conditions, two from India-one suggested that it is marginally higher in vitiligo than psoriasis [13] and the other study had the opposite result. [16] The third, from Egypt had shown a slightly lower level of psychiatric morbidity in people with vitiligo than those with psoriasis. [14] The fourth study from the United States of America compared the social functioning of patients with these two conditions and found that psoriasis patients had more social dysfunction than patients with vitiligo in a self-rated severity scale. [15]
This study made a specific attempt to quantify social and domestic participation restrictions that patients having the above two stigmatizing dermatological conditions experience from an Indian perspective and compares the severity between both these conditions. Besides, we made an attempt to use a recently developed tool called participation scale (P-scale) [17] which uses the framework of the International Classification of Functioning, Disability and Health (ICF) to measure social participation in such stigmatizing diseases. [18] It has so far not been used to measure these two conditions. The use of the word participation is based on the ICF terminology and participation restriction in this study is defined as problems an individual may experience with involvement in life situations. This study intentionally did not use relevant quality of life questionnaires such as short form (36) health survey (SF-36), a quality of life measure for patients with Skindisease (Skindex), dermatology life quality index (DLQI), the impact of chronic skin disease on daily life (ISDL) despite the fact that they have been validated for skin diseases because the ICF model was hardly elaborated theoretically in these tools.
The objectives of the study were to find out in groups of people affected by these disorders, and also compare to a control population without dermatological conditions:
- the extent of social participation and the differences between these groups;
- participation domains that were significantly affected.
Methods
Sample
The data was collected from the dermatology outpatient clinic in the southern part of India. Patients attending these clinics were a mixture of the rural population from the neighboring villages as well the urban residents of the nearby town.
Study design
It was a cross-sectional comparative study which was completed in a period of 10 months from March to December 2006. Ethics′ clearance for this study was obtained from the institution′s research committee. There were no earlier participation restriction studies on vitiligo and psoriasis. Therefore, this study adopted an earlier work in leprosy, [19] which used the p-scale to identify the subjects who have restriction in social and domestic life. It concluded that 40% of their study population suffered from participation restriction. Using this 40% as p, with 95% confidence interval and with d (allowable difference) of 20% of p, the minimum sample size needed was estimated as 144. A consecutive sample of 150 vitiligo patients and the same number of psoriasis patients who had consented and also met the following selection criteria were enrolled in the study.
- Psoriasis and vitiligo patients with no other stigmatizing diseases like leprosy.
- The patients should have no other skin disease with visible patches.
- The patients should be above 14 years of age.
- The patients should be free from psychiatric illness.
One of the researchers made certain that they were free from psychiatric illnesses. During the time of data collection no matching among cases or controls was attempted.
The subjects were classified sex-wise, and age-wise as adolescents (14 to 17 years); adults (18 to 60 years) and old age (61 years and above).
Instruments used
1. Socioeconomic status and standard of living index of NFHS-2 [20] was administered to both cases and controls. The interpretation for the household income was that if it was below Rs. 24,000/- per annum it was considered to be below the poverty line. The score for the standard of living was as follows: 0-14 indicated low standard of living; 15-24 the middle level and those who scored between 25-67 had a high standard of living.
2. Clinical profile of all the psoriasis and vitiligo cases such as the dermatological diagnosis and its type, and duration of the diagnosis, was noted. For these conditions the data of the percentage of the body surface area and body parts affected was elicited. The body was divided into nine parts as shown in [Figure - 1]. The samples were divided into three clusters based on the affected parts, such as (i) Exposed (1-6); (ii) non-exposed (7- 9); and, affected in both exposed as well in non-exposed body parts.
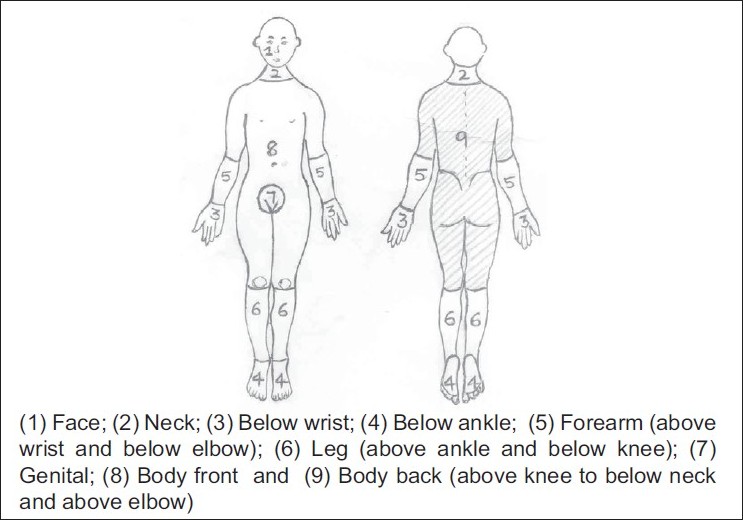 |
| Figure 1: Body parts affected |
3. Participation scale: This tool has been validated in India, Nepal and Brazil. [17] It measures the extent to which people participate in common social events. The key issue of stigma is that it excludes people from participating in such events. The Indian version has been translated into Hindi, Bengali, Telugu and Tamil and the Tamil version was used for this study, as it is the local language spoken in and around the study centre. Its intra-tester stability by Intra-class correlation coefficient (ICC) in Tamil language was 0.83 and inter-tester reliability in the same language was 0.80. The internal consistency reliability of the scale was checked with Cronbach′s alpha. It was 0.92. [17] The P-scale is an 18-item instrument (Annexure 1),[SUPPORTING:1] which covers eight out of the nine participation domains of the ICF. [18] A five-point rating scale is used to measure the level of participation for each item. For each subject the scores obtained for the 18 items were added up. If the score was 12 or less, people were considered not to have restriction in their domestic and social life situation. Scores of 13 to 90 represent restriction at different intensities; 13 to 32 as moderate, 33 to 52 as severe and 53-90 as extreme restrictions.
Procedure
Data collection was carried out on the same day over two sessions; the first was by BK who carried out the initial recruitment by diagnosing vitiligo and psoriasis. Those who fulfilled all the inclusion criteria of the study were considered for the data collection. The interviewer (PR) orally informed the subjects about the study and data was collected only from those who were willing to participate. The dermatology registrar administered the clinical profile instrument described above. Recruitment was done consecutively until the sample size was reached. After recruitment, the subjects were directed to PR who has been trained in the administration of the NFHS-2 and P-scale, to collect this information by the interview. This interviewer was blinded to the clinical profile of the samples.
Data analysis
The statistical package for social sciences (SPSS Inc., Chicago, IL) was used for all analysis. The dataset was analyzed using means, standard deviations, chi-square, ANOVA F and t-tests. A P value equal to or less than 0.05 was accepted as significant.
Results
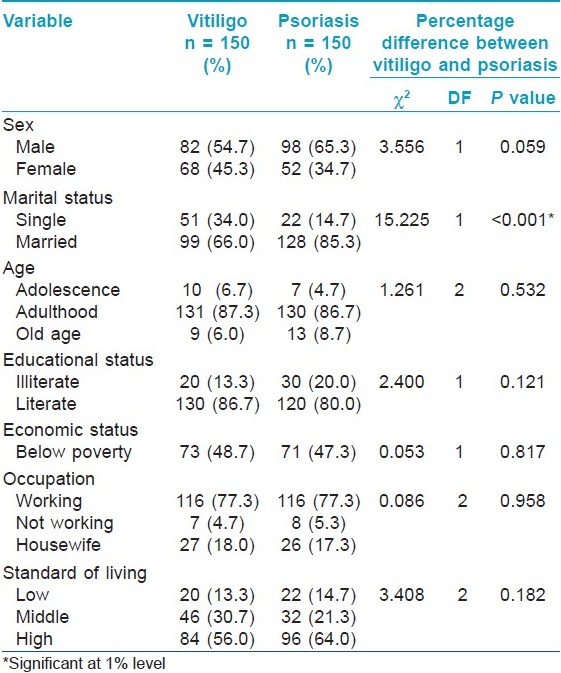
Demographic characteristics are shown in [Table - 1].In this cross-sectional study, the vitiligo and psoriasis patients had comparable socio-demographic characteristics, except in the marital status. The mean age (SD) of vitiligo and psoriasis was 35.11 (14.69) and 42.13 (15.05), respectively.
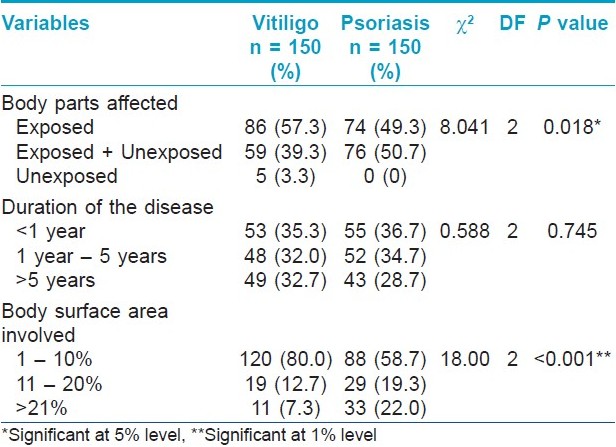
[Table - 2] revealed that the duration of the disease was almost similar in both these groups. However, in this consecutive data collection, no psoriasis patients sought medical assistance when unexposed body parts were affected; also psoriasis patients had significantly more body parts and surface area affected.
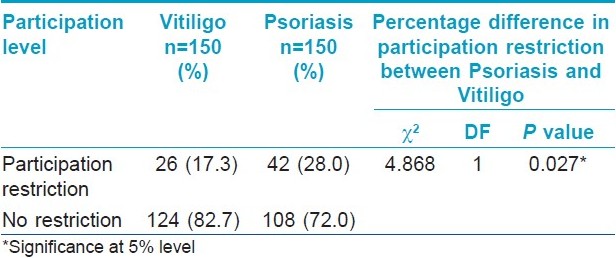
[Table - 3] shows that participation restrictions in domestic and social life were more among psoriasis patients than among vitiligo patients. [Figure - 2] shows the different intensities of participation restriction. Extreme restriction was observed only among psoriasis patients.
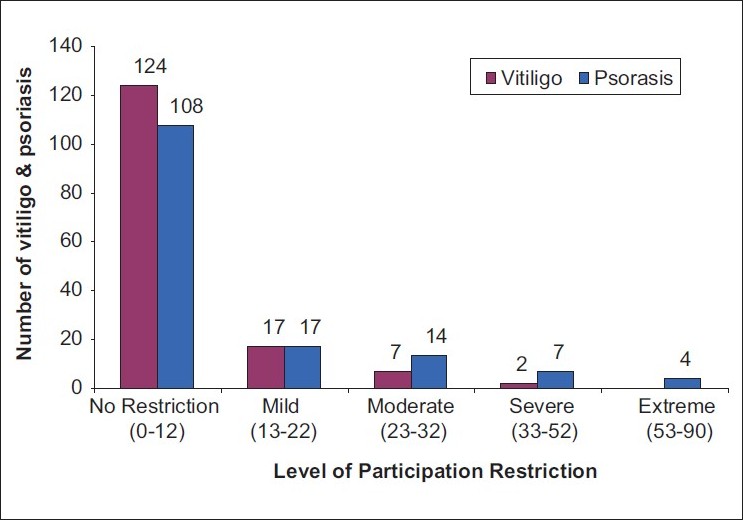 |
| Figure 2: Participation restriction at different intensities among psoriasis and vitiligo |
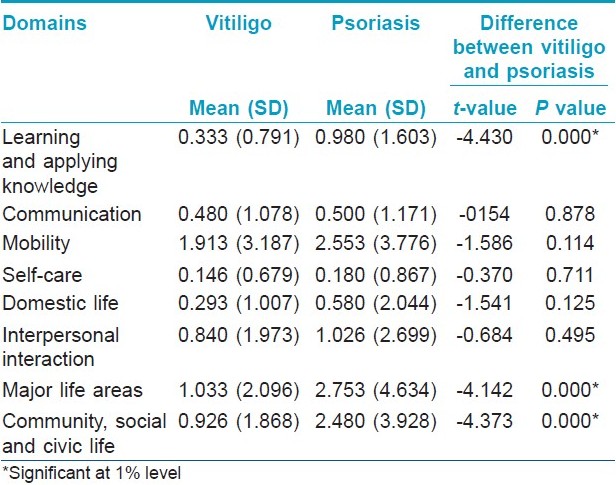
[Table - 4]: Further investigations sought to establish which participation domains were most affected in their life situations. The mean differences between the participation scores of patients with psoriasis and vitiligo were significant in learning and applying knowledge as well as in meaningfully participating in their major life areas like work, employment and education activities compared with vitiligo patients (All three domains P<0.001).
Discussion
Participation restrictions are problems experienced in any life situation, for example, in relationships or in employment. We specifically selected the participation scale to assess the above factors because it covered all but one of the participation components of the ICF and was designed for use in low and middle-income countries. The strength of this study is that it is the first of its kind to highlight the prevalence of participation restriction in patients with vitiligo and psoriasis. In addition, it was a rigorous single-blind study where both clinical and sociometric assessors did not have access to each other′s data. Besides, the data were collected from relatively large groups of patients and healthy controls.
Our results clearly showed that both vitiligo and psoriasis patients reported participation restrictions in sizeable percentages. At the same time, it was interesting to note that psoriasis patients faced more restrictions at a significant level (P = 0.027) than vitilgo patients in a number of day-to-day life situations. Moreover, psoriasis is the only condition in which some patients suffered extreme participation restrictions. It could be due to the fluctuating course of psoriasis, which is also symptomatic, whereas vitiligo patients would have become inured to their condition.
In the past, only one study from the United States (US), which compared the social functioning of these two conditions, found that psoriasis patients had more social dysfunction than patients with vitiligo in a self-rated severity scale. [15] Our study corroborates the above finding in terms of restrictions in domestic, work and social life. It is understandable that among the predominantly white population of the US a red patch due to psoriasis is more visible than a vitiligo lesion, and therefore, a psoriasis patient may suffer greater social dysfunction than a vitiligo patient. The Indian population of this study was predominantly dark-skinned, so that hypo-pigmentation as seen in vitiligo is much more noticeable than psoriatic red patches. One would therefore expect more severe social problems among vitiligo patients. Conversely, this study disagrees with such reasoning and shows clearly that the component of hypo or hyper pigmentation of the skin is not the only factor leading to participation restrictions.
The findings of this study show that a substantial proportion of patients with psoriasis had problems participating in major life areas like work, education and employment, and also in community, social and civic life [Table - 4]. A strong correlation was seen between the above findings and a number of studies from North America and Europe. For example, a large-scale national survey from the US suggested that psoriasis has a significant negative impact on overall work productivity. [21] Another US-based study found that 84% psoriasis patients reported that one of the worst things they experience was difficulty in establishing social contacts and relationships. [12] A Canadian study also indicated that moderate to severe psoriasis may have a substantial impact on the work productivity of patients with this disease. [22] A study from the UK reported that 14% of psoriasis patients discontinued careers at least once in their lives because of the appearance of their skin. [23] Another study from the same country stated that 15% of psoriasis patients experienced limited employment opportunities because of discrimination based on the appearance of their skin during job interviews. In addition, they take frequent sick leaves related to skin eruptions. Eighty-nine percent of patients reported embarrassment and shame and 42% experienced lack of self-confidence on account of their psoriasis. [24] This leads to the inference that, in the case of psoriasis a similar scenario of problems in participating in major life areas exists both in Eastern and Western populations.
Over-representation of married subjects among the psoriasis group is either due to the age factor or the stress a married life can bring about. In this study the mean (SD) age of vitiligo and psoriasis patients is 35.11 (14.69) and 42.13 (15.05) respectively [Table - 1]. Interestingly, in another Indian study that compared vitiligo and psoriasis patients, a similar mean age difference was observed. [13] With the increase in age the likelihood of a person being married is high in India where most weddings are arranged by parents. [25] An alternative inference worth considering is the physical, emotional and psychological stress a married life could bring about. This possibly aggravates the psoriasis signs and symptoms, thus more patients in married demographic groups attend the dermatological clinics.
One unanticipated but important finding of this study was delayed presentation to the dermatological clinic by psoriasis patients [Table - 2]-no psoriasis patients sought medical assistance when unexposed body parts were affected. For any disease, delay in treatment has its own implications. Therefore, one future direction to be taken is to look into why people with psoriasis delay in the help-seeking process. This could include cultural causes, social consequences, and patients′ lack of knowledge of the allopathic cure, and the consequences of delayed treatment. The second area which needs attention is to develop steps and remedies to be offered to these groups of patients to overcome participation restriction. Both these were beyond the scope of this project.
In summary, this rigorous single-blind study indicated that both psoriasis and vitiligo patients suffered moderate to severe restriction while participating in their domestic and social life. Of these two groups, psoriasis patients faced significantly more restrictions in a number of day-to-day life situations. The Indian population of this study was predominantly dark-skinned and hypo-pigmentation as seen in vitiligo is much more noticeable than psoriatic red patches. However, the results showed that the component of hypo or hyperpigmentation of the skin is not the only factor leading to participation restrictions.
| 1. |
Dhar S, Dutta P, Malakar R. Pigmentary disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 736-98.
[Google Scholar]
|
| 2. |
Pavithran K, Karunakaran M, Ragunatha S. Disorders of keratinization. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 995-1069.
[Google Scholar]
|
| 3. |
Hautmann G, Panconesi E. Vitiligo: A psychologically influenced and influencing disease. Clin Dermatology 1997;15:879-90.
[Google Scholar]
|
| 4. |
Ongenae K, Dierckxsens L, Brochez l, van Geel N, Naeyaert JM. Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology 2005;210:279-85.
[Google Scholar]
|
| 5. |
Coles RB. Group therapy in the skin department. Trans St. John's Hosp Dermatol Soc 1970;53:82-5.
[Google Scholar]
|
| 6. |
Savin JA. Patient's beliefs about psoriasis. Trans St John's Hosp Dermatol Soc 1970;56:19-42.
[Google Scholar]
|
| 7. |
Coles RB, Ryan TJ. The psoriasis sufferer in the community. Br J Dermatol 1975;93:111-2.
[Google Scholar]
|
| 8. |
Roenigk RK, Roenigk HH Jr. Sex differences in the psychological effects of psoriasis. Cutis 1978;21:529-33.
[Google Scholar]
|
| 9. |
Leichtman SR, Burnett JW, Robinson HM Jr. Body image concerns of psoriasis patients as reflected in human figure drawings. J Pers Assess 1981;45:478-83.
[Google Scholar]
|
| 10. |
Hughes JE, Barraclogh BM, Hamblin LG, White JE. Psychiatric symptoms in dermatology patients. Br J Psychiatry 1983;14:51-4.
[Google Scholar]
|
| 11. |
van der Schaar WW. Psychometric investigation in 48 Dutch patients suffering from psoriasis. Psychother Psychosom 1977;17:159-61.
[Google Scholar]
|
| 12. |
Jobling R. Learning to Live With It: An account of a career of chronic dermatological illness and patienthood. In: Davis A, Horobin G, editors. Medical Encounters, the Experience of Illness and Treatment. 1 st ed. New York: St. Martin's Press; 1977. p. 72-86.
[Google Scholar]
|
| 13. |
Mattoo SK, Handa S, Kaur I, Gupta N, Molhotra R. Psychiatric morbidity in vitiligo and Psoriasis: A comparative study from India. J Dermatol 2001;28:424-32.
[Google Scholar]
|
| 14. |
Saleh HM, Salem SA, El-Sheshetawy RS, Abd El-Samei A. Comparative study of psychiatric morbidity and quality of life in psoriasis, vitiligo and alopecia areata. Egypt Dermatol Online J 2008;4:2.
[Google Scholar]
|
| 15. |
Porter JR, Beuf AH, Lerner A, Nordlund J. Psychosocial effect of vitiligo: A comparison of vitilgo patients with normal control subjects with psoriasis patients and with patients with other pigmentary disorders. J Am Acad Dermatol 1986;15:220-4.
[Google Scholar]
|
| 16. |
Sharma N, Koranne RV, Singh RK. Psychiatric morbidity in psoriasis and vitiligo: A comparative study. J Dermatol 2001;28:419-23.
[Google Scholar]
|
| 17. |
van Brakel WH, Anderson AM, Mutatkar RK, Bakirtzief Z, Nicholls PG, Raju MS. The participation scale: Measuring a key concept in public health. Disabil Rehabil 2006;28:193-202.
[Google Scholar]
|
| 18. |
World Health Organisation. In: International classification of functioning, disability and health - Short Version, 1 st ed. Geneva: WHO Publications; 2001. p. 1-10.
[Google Scholar]
|
| 19. |
Cross H, Choudhary R. STEP: An intervention to address the issue of stigma related to leprosy in Southern Nepal. Lep Rev 2005;76:316-24.
[Google Scholar]
|
| 20. |
Roy TK, Arnold F, Kulkarni S, Kishor S. In: National Family Health Survey India - 2. Mumbai: International Institute for Population Sciences-India Publications; 2004-05. p. 35-41.
[Google Scholar]
|
| 21. |
Wu Y, Mills D, Bala M. Impact of psoriasis on patients' work and productivity: A retrospective, matched case-control analysis. Am J Clin Dermatol 2009;10:407-10.
[Google Scholar]
|
| 22. |
Chan B, Hales B, Shear N, Ho V, Lynde C, Poulin Y, et al. Work-related lost productivity and its economic impact on Canadian patients with moderate to severe psoriasis. J Cutan Med Surg 2009;13:192-7.
[Google Scholar]
|
| 23. |
Ramsey B , O'Reagan M. A survey of the social and psychological effects of psoriasis. Br J Dermatol 1988;118:195-201.
[Google Scholar]
|
| 24. |
Jowett S, Ryan T. Skin disease and handicap: An analysis of the impact of skin conditions. Soc Sci Med 1985;20:425-9.
[Google Scholar]
|
| 25. |
Kulhara P, Avasthi A, Gupta N. Life events and social support in married schizophrenics, Ind J Psychiatry 1998;40:376-82.
[Google Scholar]
|
Fulltext Views
4,210
PDF downloads
1,802





