Translate this page into:
Pattern and prevalence of physiological cutaneous changes in pregnancy: A study of 2000 antenatal women
2 Department of Obstetrics and Gynecology, Government Medical College and Hospital, Jammu, Jammu and Kashmir-180 001, India
Correspondence Address:
Shagufta P Rathore
Department of Dermatology, Government Medical College and Hospital, Jammu, Jammu and Kashmir-180 001
India
| How to cite this article: Rathore SP, Gupta S, Gupta V. Pattern and prevalence of physiological cutaneous changes in pregnancy: A study of 2000 antenatal women. Indian J Dermatol Venereol Leprol 2011;77:402 |
Sir,
During pregnancy immunologic, endocrine, metabolic and vascular changes occur that make pregnant women particularly susceptible to changes of skin and its appendages. Whether physiologic or pathologic, these changes affect virtually every organ of pregnant women including the skin. Some of these changes are due to de novo production of a variety of protein and steroid hormones by the fetoplacental unit as well as the increased activity of maternal pituitary, thyroid and adrenal glands. [1]
Cutaneous changes and eruptions during pregnancy are exceedingly common and in some cases a cause for substantial anxiety on the part of the prospective mother. Some of these are benign and reversible after delivery whereas others can have potential effects on the fetus in terms of morbidity and mortality. [1] The present prospective study is an attempt to provide a framework for an effective approach to the spectrum of physiological cutaneous changes encountered in antenatal women.
Two thousand randomly selected, asymptomatic pregnant females, attending the Outpatient Department of Obstetrics and Gynecology, Govt. Medical College and Hospital, Jammu, for a routine antenatal checkup, irrespective of the period of gestation, were enrolled from October 2007 to September 2009. After an informed consent, a detailed history was recorded followed by complete general physical, relevant systemic and a detailed dermatological examination of all patients to study the physiological changes of skin and its appendages. Relevant clinical details were recorded and results compiled in tabulated form.
The age range of patients was 18 to 40 years (mean 26.42 ± 4.05); 63.55% cases were up to 25 years of age; 56.35% were primigravidae; 53.85% cases were in the third and 34.00% in the second trimester of pregnancy. Fifty-eight percent cases belonged to rural areas. 92.7% were housewives and most of them belonged to the lower-middle and lower socioeconomic classes.
Physiological cutaneous changes were seen in 87.55% cases, which included pigmentary changes in 85.9%, connective tissue changes in 64.8%, vascular changes in 25.5%, glandular changes in 13.9%, hair changes in 3.4%, and nail changes in 2.1% [Table - 1]. Other studies have reported physiological skin changes in up to 100% cases. [2],[3]
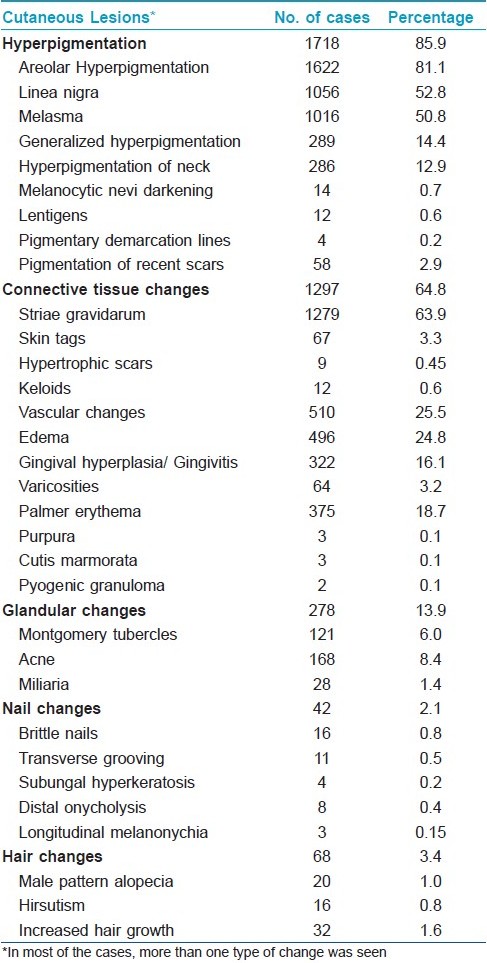
Pigmentary changes were most common, seen in 85.9% cases which were consistent with earlier studies. [2],[3],[4] Melasma [Figure - 1] has been reported to occur in 50-70% of pregnant women. [4] It was seen in 50.8% of our cases, thus conforming to earlier findings. [2],[5] A very low prevalence has been reported by some studies. [3],[6],[7] The possible reason for discrepancy in prevalence could be the skin phototypes and racial differences. The commonest clinical pattern found was the centrofacial pattern (76%) which was consistent with earlier reports. [3],[4] Others have found the malar pattern to be the commonest. [5]
 |
| Figure 1: Melasma: Centrofacial pattern |
Hyperpigmentation of the neck was seen in 12.9% cases whereas Muzaffar et al., [2] reported it in 24.2% cases. Pigmentary demarcation lines, known to appear for the first time during pregnancy were seen in 0.25% cases, similar to 0.3% by Rashmi et al. [3]
Striae gravidarum [Figure - 2] were observed in 63.9% cases, comparable to those reported earlier. [2],[3],[8] The most common site involved was the lower abdomen (92.7%), with an onset mostly during the second trimester, similar to that reported by Chang et al. [8] Familial and racial factors are said to play a role in their development. [8] None of our patients were aware of it.
 |
| Figure 2: Striae gravidarum: Pink-purple linear streaks |
Vascular changes result from distention, instability and proliferation of vessels [9] and were seen in 25.5% cases. Non-pitting edema over the hands, feet and face was observed in 24.8% cases with an onset mostly in the third trimester . Muzaffar et al., [2] reported edema in 48.5% whereas Rashmi et al., [3] reported it in 9.8%. Varicosities [Figure - 3] were seen in 3.2% cases , comparable to the earlier studies. [2],[6] A higher prevalence of up to 40% has been reported. [9]
 |
| Figure 3: Varicosities in lower limbs |
Palmar erythema was observed in 18.7% and spider angioma in 2.1% cases, consistent with other studies. [2],[4] Rashmi et al., [3] reported no case of palmar erythema. Saudeau et al., [7] observed vascular spiders in 53% pregnant women. This discrepancy could be due to erythema being readily appreciated in light-skinned people.
Gingivitis [Figure - 4] may occur in up to 100% of pregnant women with varying degree of severity; [4] 16.1% cases of gingivitis were seen which is in agreement with earlier reports. [2]
 |
| Figure 4: Gingivitis |
The cause as well as significance of nail changes occurring in pregnancy is unknown but they have been described. [2],[3] These were seen in 2.1% of our cases. During pregnancy, conversion of hair from anagen to telogen is slowed down which accounts for observed increase in percentage of anagen hair and decrease in telogen hair. [2],[9] Hair changes were seen in 3.4% cases, comparable to those reported by Rashmi et al. [3] Muzaffer et al., [2] reported them in 12.8% cases.
As the knowledge accumulates regarding the interaction of pregnancy with skin diseases, it can be concluded that a variety of cutaneous lesions can be seen in pregnant women. Awareness about and recognition of their clinical presentation is important for correct diagnosis that will direct the most appropriate laboratory evaluation and careful management in an effort to minimize maternal and fetal morbidity.
| 1. |
Kroumpouzos G, Cohen LM. Dermatoses of pregnancy. J Am Acad Dermatol 2001;45:1-19.
[Google Scholar]
|
| 2. |
Muzaffar F, Hussain I, Haroon TS. Physiologic skin changes during pregnancy: A study of 140 cases. Int J Dermatol 1998;37:429-31.
[Google Scholar]
|
| 3. |
Kumari R, Jaisankar TJ, Thappa DM. A clinical study of skin changes in pregnancy. Indian J Dermatol Venereol Leprol 2007;73:141.
[Google Scholar]
|
| 4. |
Wong RC, Ellis CN. Physiologic changes in the skin during pregnancy. J Am Acad Dermatol 1984;10:929-40.
[Google Scholar]
|
| 5. |
Goh CL, Dlova CN. A Retrospective Study on the Clinical Presentation and Treatment Outcome of Melasma in a Tertiary Dermatological Referral Centre in Singapore. Singapore Med J 1999; 40:455-8.
[Google Scholar]
|
| 6. |
Raj S, Khopkar U, Kapasi A, Wadhwa SL. Skin in pregnancy. Indian J Dermatol Venereol Leprol 1992;58:84-8.
[Google Scholar]
|
| 7. |
Saudeau L, Pierre F, Barruet K, Vaillant L, Lorette G. Physiological cutaneous signs in normal pregnancy: A study of 60 pregnant women. Ann Dermatol Venereol 1994;121:227-31.
[Google Scholar]
|
| 8. |
Chang AL, Agredano YZ, Kimball AB. Risk factors associated with striae gravidarum. J Am Acad Dermatol 2004;51:881-5.
[Google Scholar]
|
| 9. |
Winton GB, Lewis CW. Dermatoses of pregnancy. J Am Acad Dermatol 1982;6:977-8.
[Google Scholar]
|
Fulltext Views
4,271
PDF downloads
2,741





