Translate this page into:
Cutaneous relapse of primary testicular non-Hodgkin lymphoma-The first sign of disease dissemination
2 Department of Pathology, Dr. Ram Manohar Lohia Hospital, New Delhi, India
Correspondence Address:
Hemanta K Kar
Department of Dermatology, Dr. Ram Manohar Lohia Hospital, New Delhi - 110 001
India
| How to cite this article: Langar S, Sharma PK, Bhardwaj M, Kar HK. Cutaneous relapse of primary testicular non-Hodgkin lymphoma-The first sign of disease dissemination. Indian J Dermatol Venereol Leprol 2010;76:576-578 |
Sir,
Primary non-Hodgkin lymphoma of the testis is a rare tumor, accounting for less than 1% of all non-Hodgkin lymphomas. The prognosis is poor, with majority of patients presenting with relapse within the first 2 years following treatment. [1] The most common sites of relapse include central nervous system (CNS) and contralateral testis in majority of the patients. [2],[3] Skin as the first site of relapse is uncommon and has been infrequently mentioned in the literature. [3],[4] In this letter, we report a rare case of isolated cutaneous relapse of the testicular lymphoma 2 years following treatment.
A 54-year-old man presented with 2-month old asymptomatic red lesions on the right buttock and left forearm. The patient did not have any systemic complaints. He had been diagnosed with left testicular non-Hodgkin lymphoma (NHL) of diffuse large B-cell type (Ann Arbor stage IV) 2 years back. The lymphoma was positive for LCA, CD 20, CD43 and negative for CD3 and placental alkaline phosphate (PLAP). He had undergone left high orchidectomy followed by 8 cycles of postoperative cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP)-derived chemotherapy. Since then, the disease had been under remission for 2 years.
The results of the patient′s general physical and systemic examinations were normal. There were 2 well-defined erythematous, annular, indurated, mildly scaly plaques of size 5 Χ 4 and 3 Χ 2 cm on the lateral side of the right buttock and anterior aspect of the left forearm, respectively [Figure - 1] and [Figure - 2]. The forearm plaque showed mild central clearing and 3 erythematous papular lesions proximal to it. There was no sensory loss and no nerve enlargement.
 |
| Figure 1 : Erythematous, indurated plaque on the right buttock |
 |
| Figure 2 : Erythematous, indurated plaque with central clearing and 3 proximal papular lesions on the left forearm |
In view of the past history of testicular NHL in the patient, a full lymphoma workup was undertaken. Levels of hematological and biochemical parameters, including serum lactate dehydrogenase level, were normal. X-ray chest, computed tomography scans of head and neck, chest, abdomen and pelvis did not show any evidence of lymphoma recurrence. Results of bone marrow examination, bone scan of the body and cerebrospinal fluid examination were also normal. Whole-body Positron emission tomography - computed tomography (PET-CT) scan showed focal involvement in the region of the cutaneous plaques, indicating isolated relapse of testicular lymphoma in the skin. Histopathological examination of the cutaneous plaques showed normal epidermis with heavy, diffuse and interstitial infiltrate of atypical intermediate and large mononuclear lymphoid cells in the entire thickness of the dermis [Figure - 3] and [Figure - 4]. On immunohistochemistry, the mononuclear cells were positive for LCA, CD 20, CD43 and negative for CD 3. The CD expression was identical to the original testicular tumor. A diagnosis of isolated cutaneous relapse of primary testicular B-cell lymphoma was made, and the patient was referred to oncology for further management. Treatment with rituximab (monoclonal antibody against CD 20) was initiated for his cutaneous lesion, with partial response. Eventually the patient developed relapses in the CNS, gastrointestinal tract, lungs and liver before succumbing to his illness 13 months after the initial diagnosis of cutaneous relapse.
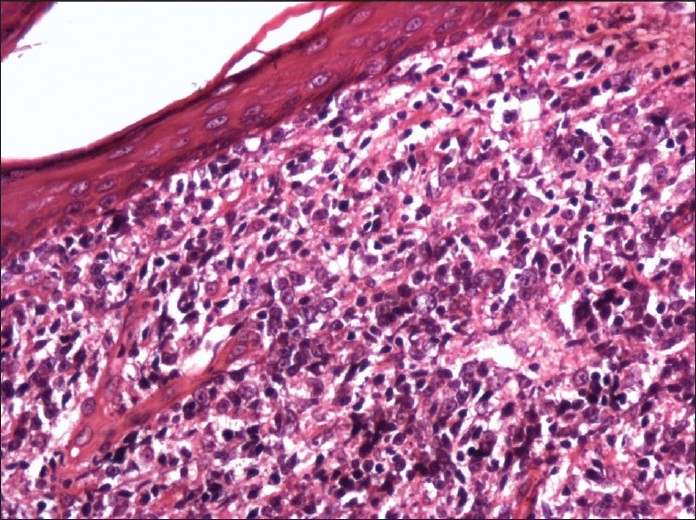 |
| Figure 3 : Heavy, diffuse and interstitial infiltrate of atypical intermediate and large mononuclear lymphoid cells in the entire thickness of the dermis (H and E, ×200) |
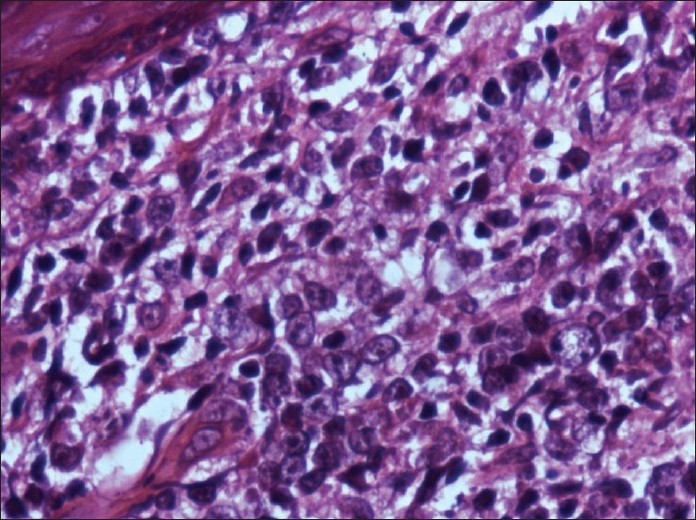 |
| Figure 4 : Infiltrate of atypical intermediate and large mononuclear lymphoid cells in the dermis (H and E, ×400) |
Lymphomas are malignancies of lymphoid cells which present as solid tumors of the immune system. The non-Hodgkin lymphomas may manifest either as primary lymph-node disease or may involve an extranodal site. [1] Primary non-Hodgkin lymphoma of the testis is a rare neoplasm occurring in older men. It accounts for 1% of all non-Hodgkin lymphomas and 1% to 7% of all testicular malignancies. Histologically 80% to 90% of the primary testicular lymphomas are of diffuse large B-cell immunophenotype. [1],[2],[3] The prognosis is poor, with majority of patients presenting with relapse in the CNS and contralateral testis within the first 2 years following treatment. [2],[3] Rarely patients may show relapse at other extranodal sites, such as bone, bone marrow, lung, adrenal glands, skin, liver, gastrointestinal tract and spleen. [4],[5] The cause of extranodal relapse in primary testicular lymphomas remains unclear. A particular pattern of aberrant expression of adhesion molecules on the neoplastic cells resulting in poor adhesion of lymphoma cells to the extracellular matrix of the primary neoplasm and alteration of cell-mediated host responses may contribute to this behavior. [6] Thus a patient with a history of lymphoid malignancy (nodal or extranodal), presenting with a cutaneous plaque should be thoroughly investigated keeping in view the possibility of cutaneous relapse of the lymphoma.
| 1. |
Lagrange JL, Ramaioli A, Theodore CH, Lacombe MJ, Beckendorf V, Biron P, et al. Non-Hodgkin's lymphoms of the testis: A retrospective study of 84 patients treated in the French anticancer centers. Ann Oncol 2001;12:1313-9.
[Google Scholar]
|
| 2. |
Tondini C, Ferrerri AJ, Siracusano L, Valagussa P, Giardini R, Rampinelli I, et al. Diffuse large cell lymphoma of the testis. J Clin Oncol 1999;17:2854-8.
[Google Scholar]
|
| 3. |
Ingram RM, Williams ME, Fintel WA, Ross M. Testicular lymphoma: A literature review and report of a case with a zoster-like cutaneous recurrence. Clin Lymphoma 2002;2:238-41.
[Google Scholar]
|
| 4. |
Zucca E, Conconi A, Mughal TI, Sarris AH, Seymour JF, Vitolo U, et al. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the international extranodal lymphoma study group. J Clin Oncol 2003;21:20-7.
[Google Scholar]
|
| 5. |
Marisavljevic D, Zivkovic R, Markovic O, Martinovic VC. Skin infiltration as solely manifestation of late extranodal relapse of testicular diffuse B- cell lymphoma. Haema 2006;9:582-4.
[Google Scholar]
|
| 6. |
Horstmann WG, Timens W. Lack of adhesion molecules in testicular diffuse entroblastic and immunoblastic B cell lymphomas as a contributory factor in malignant behaviour. Virchows Arch 1996;429:83-90.
[Google Scholar]
|
Fulltext Views
2,686
PDF downloads
1,202





