Translate this page into:
Localization of T-cell subsets in cutaneous lichen planus: An insight into pathogenetic mechanism
2 Department of Pathology, All India Institute of Medical Sciences, Delhi, India
3 Department of Skin V.D., Hindu Rao Hospital, Delhi, India
Correspondence Address:
Ruchika Gupta
Department of Pathology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 10029
India
| How to cite this article: Rana S, Gupta R, Singh S, Mohanty S, Gupta K, Kudesia M. Localization of T-cell subsets in cutaneous lichen planus: An insight into pathogenetic mechanism. Indian J Dermatol Venereol Leprol 2010;76:707-709 |
Sir,
We would like to report the results of our evaluation of T-cell subsets in cutaneous lichen planus (LP). For the study, 20 cases of cutaneous LP over a one-year period (2007-2008) were included and diagnosis confirmed by a review of the clinical and histopathological features. Patients with features suggestive of systemic lupus erythematosus, human immunodeficiency virus infection or other chronic medical illnesses were excluded. Immunohistochemistry for T-cell helper subset (CD4, BioGenex, USA) and T-cell cytotoxic/ suppressor subset (CD8, BioGenex, USA) was performed on serial sections using the immunoperoxidase technique. The biopsies were examined for inflammatory cells at two locations - dermo-epidermal junction and upper reticular dermis (perivascular locations). Quantification of CD4 and CD8 T cells was performed by two independent observers at X200 magnification. A mean of the observations were taken and the relative proportion (percentage) of CD4 and CD8 subsets of T cells at each location was calculated. Non-parametric test was used to find the significance of difference in T cell subsets at the two locations.
The mean age of our cases was 36.95 ± 16.32 years with slight predominance of females (male: female 1:1.5). Skin biopsies in all cases showed the characteristic histopathological features of lichen planus. At the dermo-epidermal location, the percentage of CD4+ cells ranged from 10 to 50% of total number of T cells, with a mean of 32.3% of cells. On the other hand, CD8+ T cells [Figure - 1]a, b ranged from 52 to 90%, with a mean of 67.7% of cells. In contrast, the peri-vascular location showed preponderance of CD4+ cells [Figure - 1]c ranging from 50 to 88% (mean 69.65%) in the sparse number of T cells present. The CD8+ T cells ranged from 12 to 50%, with a mean of 30.35% of cells.
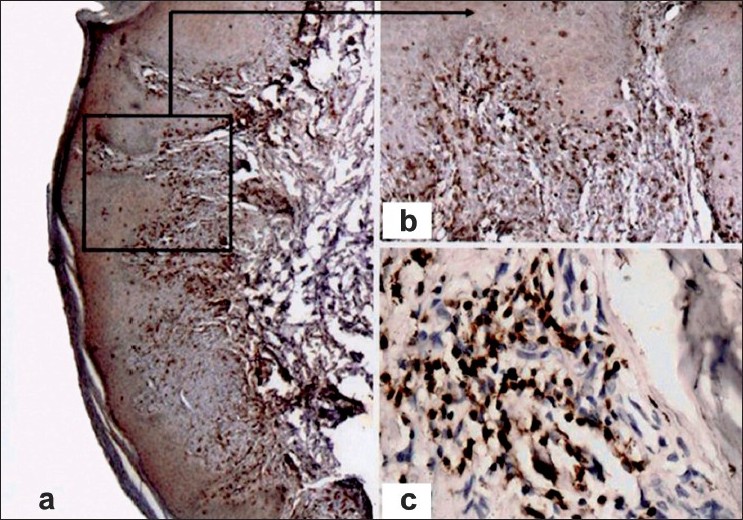 |
| Figure 1: Photomicrograph showing immunohistochemical staining in cutaneous lichen planus with (a, ×100) CD8 demonstrating CD8-positive cells at the dermo-epidermal junction, (b, ×200) higher power view demonstrating the CD8-positive cells, (c, ×200) CD4 staining showing CD4-positive cells in the perivascular location |
The relative percentages of CD 4+ and CD 8+ T cells at the dermo-epidermal junction and in lower dermis are tabulated in [Table - 1]. The difference in percentage of CD 4+ T cells between dermoepidermal junction and perivascular location was statistically significant (Mann-Whitney test, p <0.001). Similar results were obtained for CD8+ T cells, as shown in [Table - 1].
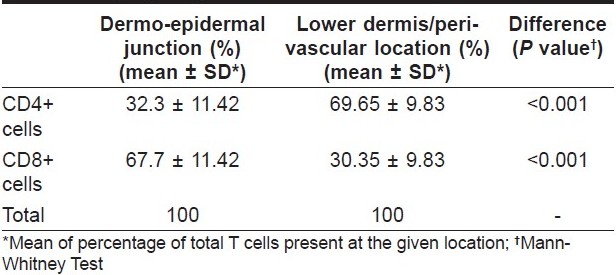
LP is a chronic muco-cutaneous inflammatory disease with typical histopathological changes of compact orthokeratosis with hypergranulosis, irregular acanthosis, basal cell damage and a band-like infiltrate of lymphocytes. [1] Elaborate studies have been performed in cases of oral LP to analyze the subsets of T lymphocytes. The majority of subepithelial and intraepithelial inflammatory cells in oral LP are CD8+ T cells. [2],[3] Activated CD8+ T cells trigger basal cell apoptosis through perforin/ granzyme or Fas/ Fas ligand pathways. [2] At the same time, most of the lymphocytes in lamina propria of oral LP are CD4+ helper T cells. [4] In cutaneous LP also, the inflammatory cells have been shown to be T lymphocytes with majority expressing HLA-DR antigen and some showing expression of IL-2 receptor. [5] Earlier analysis of the various subtypes of T cells has yielded contradictory results, with some authors demonstrating predominance of helper-inducer CD4+ T cells and others reporting suppressor-cytotoxic T lymphocytes as the main subset present in the infiltrate. [4],[6] We found the presence of CD8+ effector T cells as well as CD4+ helper T cells in cutaneous LP. The present study supports the primary role of CD8+ cytotoxic T cells in keratinocyte damage, since the dermo-epidermal infiltrate was seen to be composed predominantly of CD8+ T cells. The perivascular localization of CD4+ T cells is an indicator of the possible assistance offered to the cytotoxic CD8+ cells by secretion of Th1 cytokines. Keratinocyte damage by CD8+ T cells would lead to basement membrane disruption, paving way for the influx of more CD8+ T cells and further basal cell damage resulting in a vicious cycle leading to chronicity of the disease. Our results on cutaneous lichen planus are similar to those postulated for oral LP. [2],[3] The predominance of T cells in the inflammatory infiltrate, as seen in our study, also excludes a primary role of humoral immune mechanism in the pathogenesis of cutaneous LP. With the advent of directed immunotherapy, a detailed study of the pathogenetic mechanisms would provide further refinement of the therapeutic strategies for patients with cutaneous lichen planus. The results of the present study require to be confirmed in further studies.
In conclusion, cutaneous lichen planus is a T-cell mediated inflammatory disease with pathogenetic role of both CD8+ cytotoxic T cells and CD4+ helper T cells. There is a predominance of cytotoxic T cells in the dermo-epidermal infiltrate responsible for keratinocyte damage. Helper/ inducer CD4+ T cells are found in the perivascular dermal infiltrate, which may be assisting the cytotoxic cells in the keratinocyte damage.
| 1. |
Ellis FA. Histopathology of lichen planus based on analysis of one hundred biopsies. J Invest Dermatol 1967;48:143-8.
[Google Scholar]
|
| 2. |
Sugerman PB, Savage NW, Walsh LJ, Zhao ZZ, Zhou XJ, Khan A, et al. The pathogenesis of oral lichen planus. Crit Rev Oral Biol Med 2002;13:350-65.
[Google Scholar]
|
| 3. |
Iijima W, Ohtani H, Nakayama T, Sugawara Y, Sato E, Nagura H, et al. infiltrating CD8+ T Cells in oral lichen planus predominantly express CCR5 and CXCR3 and carry respective chemokine ligands RANTES/CCL5 and IP-10/CXCL10 in their cytolytic granules: a potential self-recruiting mechanism. Am J Pathol 2003;163:261-8.
[Google Scholar]
|
| 4. |
Ishii T. Immunohistochemical demonstration of T cell subsets and accessory cells in oral lichen planus. J Oral Pathol 1987;16:356-61.
[Google Scholar]
|
| 5. |
Sundquist KG, Wanger L. Expression of lymphocyte activation markers in benign cutaneous T-cell infiltrate: discoid lupus erythematosus versus lichen ruber planus. Acta Derm Venereol (Stockh) 1989;69:292-5.
[Google Scholar]
|
| 6. |
Buechner SA. T-cell subsets and macrophages in lichen planus. Dermatologica 1984;169:325-9.
[Google Scholar]
|
Fulltext Views
3,829
PDF downloads
1,411





