Translate this page into:
Fetal varicella syndrome
Correspondence Address:
S Ramachandra
Professor and Head, Department of DVL, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda, Andhra Pradesh
India
| How to cite this article: Ramachandra S, Metta AK, Haneef NS, Kodali S. Fetal varicella syndrome. Indian J Dermatol Venereol Leprol 2010;76:724 |
Abstract
Fetal varicella syndrome is a rare condition of the newborn, presenting with cutaneous scars, limb defects and ocular and central nervous system abnormalities. It is due to varicella or zoster developing in the fetus following maternal varicella infection during early pregnancy. We are reporting one such patient who presented with a linear, depressed, erythematous scar over the left forearm and axillary fold, with a history of maternal chicken pox during the first trimester of pregnancy.Introduction
Fetal varicella syndrome (FVS) is a rare complication of maternal varicella infection occurring in <2% of the babies born to women infected with varicella between 7 and 28 weeks of pregnancy. [1],[2],[3] The newborn may present with low birth weight, cutaneous scars, papular lesions, localized absence of skin on a limb, hypoplasia of one or more limbs, malformed digits along with various ocular and central nervous system (CNS) abnormalities. [3],[4] We are reporting one such case in view of paucity of reports from the Indian subcontinent. [5]
Case Report
Dermatologists opinion was sought for a newborn male baby on the 2 nd day of birth, born with scars over the left upper limb. There was no history of vesiculobullous lesions. The baby was born to a 22-year-old lady (gravida 2 para 1) at full term by cesarian delivery for non-progression of labor. She had a history of chicken pox during the first trimester of pregnancy. Birth weight of the child was 3.2 kg and APGAR score was 8-10. There was no history of consanguinity. Investigations like ultrasonography (fetal anomaly scan) or TORCH battery could not be performed as the mother did not get routine antenatal check ups in our hospital. The previous delivery was a full-term normal vaginal delivery and the baby was healthy.
Cutaneous examination of the child revealed a linear, irregular, depressed, erythematous scar measuring 12 cm × 5 cm over the anteromedial aspect of the left forearm. A similar small scar was present over the left axillary fold [Figure - 1] and [Figure - 2]. This distribution corresponds to C8 and T1 dermatomes. There was no limb hypoplasia, malformed digits, ocular changes or CNS abnormalities. There were no skeletal deformities on X-ray. The patient′s routine blood and urine parameters were within normal limits. His blood group was O positive and Venereal Diseases Research Laboratory test and human immunodeficiency virus antibodies were non-reactive. Differential diagnosis of neonatal scars was considered [Table - 1], but a diagnosis of FVS was made based on the characteristic history and clinical features.
 |
| Figure 1 :Irregular, depressed, erythematous scars over the left forearm and axillary fold |
 |
| Figure 2 :Close-up view of the scar over the left forearm |

The parents of the baby were counseled about the condition and reassured. No active intervention was advised at this stage.
Discussion
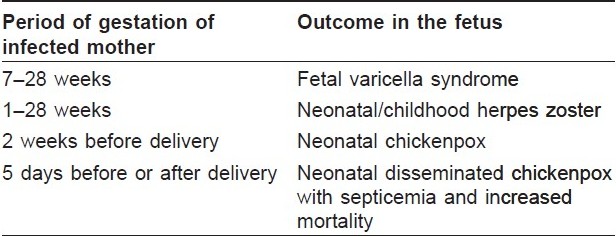
Chicken pox may develop during pregnancy in one to five per 10,000 pregnancies. If infection occurs during the last 2 weeks of pregnancy, the infection may be transmitted to the fetus and the newborn may present with varicella at or soon after birth. [2] The neonate may develop severe disseminated varicella and septicemia with increased mortality (up to 28%) if maternal infection occurs 5 days before or after delivery due to the absence of protective maternal antibodies. [2] Occasionally, herpes zoster can occur in early infancy if the child has been infected with varicella zoster virus during early intrauterine life. [6] Maternal varicella occurring between 7 and 28 weeks of pregnancy may lead to either spontaneous abortions or "fetal varicella syndrome" [Table - 2]. [2],[4],[5],[6]
FVS was first described in 1947 by La Foret and Lynch. [1] Srabstein et al. rediscovered the syndrome in 1974 and named it "congenital varicella syndrome." [7],[8] Subsequently, the condition has been reported under various names like congenital varicella zoster syndrome, fetal varicella zoster syndrome, varicella embryopathy, varicella embryofetopathy, etc.
A majority of the cases (90%) of FVS occur as a complication due to maternal varicella infection during the 1 st or 2 nd trimesters of pregnancy, and a few cases (10%) follow maternal herpes zoster. [7] Risk of transmission to fetus is approximately 2% and is especially more common when the mother has infection between the 13 th and 20 th weeks of gestation. [3],[6]
The typical clinical features include low birth weight, cutaneous lesions like scars often in a dermatomal outline (70%), papular lesions resembling connective tissue nevi, ocular abnormalities (66%) like choreoretinitis, cataracts, microophthalmia, Horner′s syndrome, nystagmus, limb hypoplasia (50%), CNS abnormalities (46%) including seizures, mental retardation, hydrocephalus, cortical atrophy, cerebellar aplasia, encephalomyelitis and dorsal radiculitis, and poor sphincter control (32%). [7]
In anticipated cases of FVS, amniocentesis, fetal blood and chorionic villous sampling may be performed to isolate the virus or to detect specific IgM. Pregnant women who are suspected not to be immune and who experience exposure to varicella zoster should be given varicella zoster immunoglobulin (VZIG) within 3 days after contact, although the efficacy is doubtful. [2] Termination of pregnancy is not indicated as the risk of fetal damage is less. Plastic surgery may be considered for the scars and limb abnormalities.
The case described above shows cutaneous scars typical of FVS, and there is history of varicella in the mother during the first trimester of pregnancy. The segmental distribution of scars probably reflects damage to the fetal nervous system by the neurotrophic virus. [8],[9] Our case is being reported to increase awareness about this rare but fascinating condition, which requires a high index of suspicion and careful history for diagnosis.
| 1. |
La Foret EG, Lynch LL. Multiple congenital defects following maternal varicella. N Eng J Med 1947;236:534-7.
[Google Scholar]
|
| 2. |
Criton S. Viral infections. In: Valia RG, Valia AR, editors. IADVL Textbook of dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 331-96.
[Google Scholar]
|
| 3. |
Pastuszak AL, Levy M, Schick B, Zuber C, Feldkamp M, Gladstone J, et al. Outcome after maternal varicella infection in the first 20 weeks of pregnancy. N Eng J Med 1994;330:901-5.
[Google Scholar]
|
| 4. |
Enders G, Miller E, Cradock-Watson J, Bolley I, Ridehalgh M. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet 1994;343:1548-51.
[Google Scholar]
|
| 5. |
Sasidharan CK, Anoop P. Congenital varicella syndrome. Indian J Pediatr 2003;70:101-3.
[Google Scholar]
|
| 6. |
Sterling JC. Virus infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 7 th ed. Oxford: Blackwell Science Ltd; 2004. p. 251-83.
th ed. Oxford: Blackwell Science Ltd; 2004. p. 251-83.'>[Google Scholar]
|
| 7. |
Gershon AA, Silverstein SJ. Varicella-zoster virus. Richman DD, Whitley RJ, Hayden FG, editors. Clinical virology. New York: Churchill Livingstone;1997. p. 421-44.
[Google Scholar]
|
| 8. |
Srabstein JC, Morris N, Larke RP, DeSa DJ, Castelino BB, Sum E. Is there a congenital varicella syndrome? J Paediatr 1974;84:239-43.
[Google Scholar]
|
| 9. |
Atherton DJ, Gennery AR, Cant AJ. The neonate. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 7 th ed. Oxford: Blackwell Science Ltd; 2004. p. 1.1-14.86.
th ed. Oxford: Blackwell Science Ltd; 2004. p. 1.1-14.86.'>[Google Scholar]
|
Fulltext Views
10,138
PDF downloads
2,984





