Translate this page into:
A case of micro-melanoma and its dermoscopic features
*These authors contributed equally to this manuscript
Corresponding author: Dr. Zizhong Liu, Department of Dermatology, The Fourth People’s Hospital of Zhenjiang, 20 Zhengdong Road, Zhenjiang, 212001, Jiangsu, China. 492151523@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Huang Y, Yang J, Bi M, Liu Z. A case of micro-melanoma and its dermoscopic features. Indian J Dermatol Venereol Leprol 2021;87:71-5.
Sir,
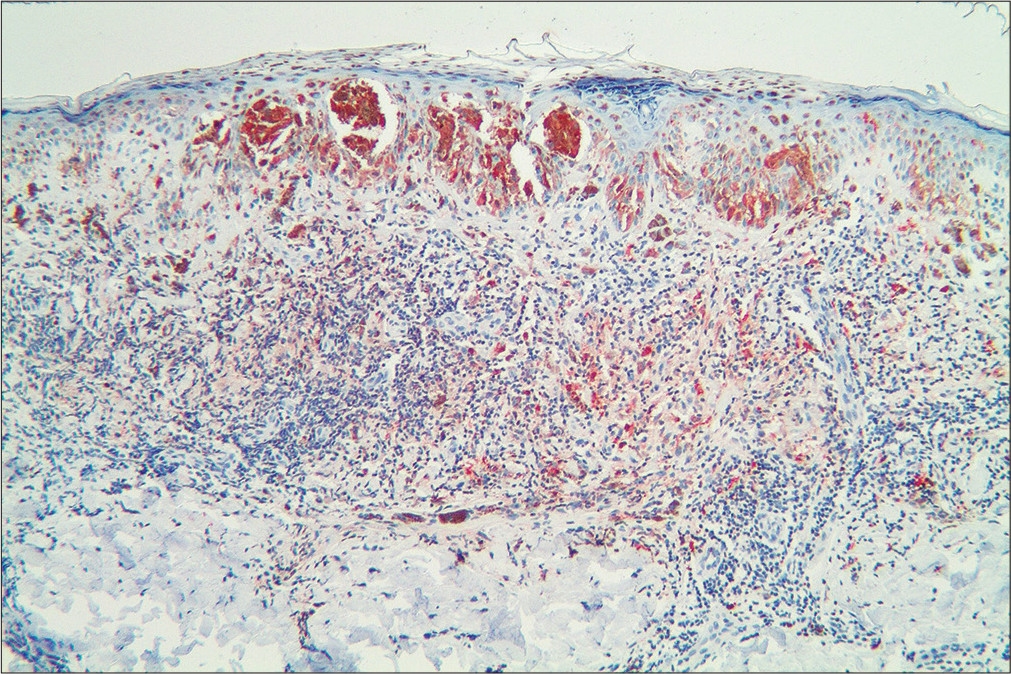
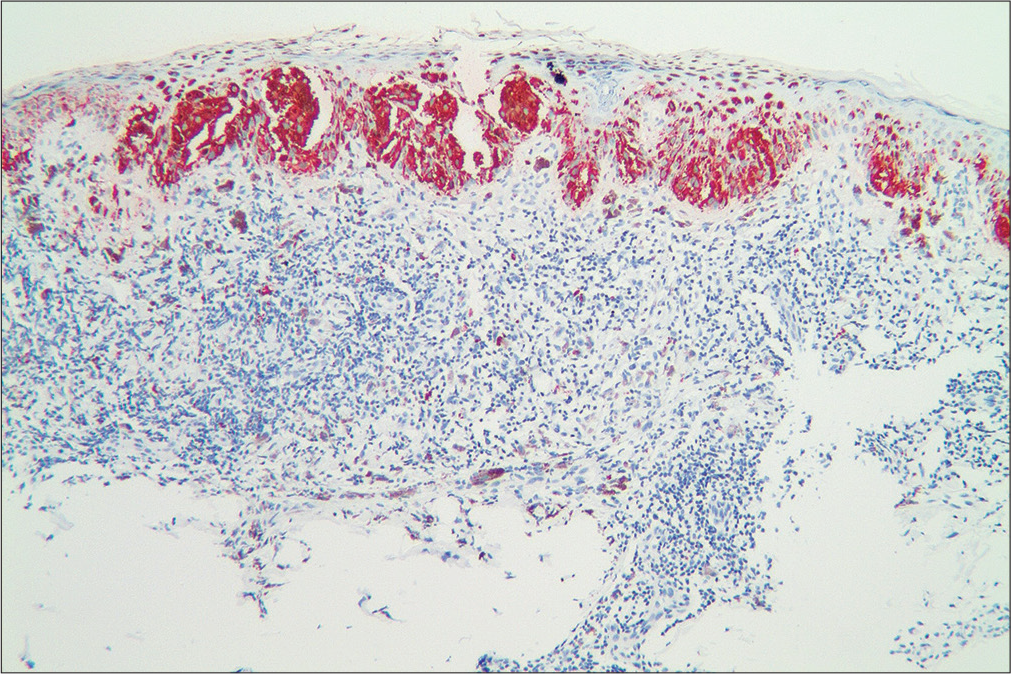
A 45-year-old woman incidentally observed an asymptomatic small black papule on her left calf. She had no past history of melanoma. Physical examination revealed a small, round, black papule on her left calf, which was approximately 2.3 mm in diameter and symmetrical in shape [Figure 1a]. Also, several small brown naevi were seen scattered on the skin, with no obvious abnormality in shape or colour. There was no peripheral lymphadenopathy. Chest radiography and doppler sonography of the liver, bile ducts, pancreas and spleen revealed no anomalies. Dermoscopy (Heine Delta 20, Germany, non-polarized, ×20) of the papule on the calf revealed dark brown homogeneous pigmentation with pseudopods and abruptness of pigment patterns at the periphery, with structure asymmetry in one axis [Figure 1b]. This pigmentation had a starburst-like pattern. Histopathology revealed atypical melanocytes in the epidermis and hair root sheath [Figure 2a]. These melanocytes contained macronuclei and were hyperchromatic and heteromorphic in nature [Figure 2b]. Immunohistochemical staining revealed that neoplastic cells were positive for Melan A, S100 and HMB 45 [Figure 2c-e]. Based on these findings, a diagnosis of melanoma in situ was made.

- Black papule on the left calf of maximum diameter 2.3mm
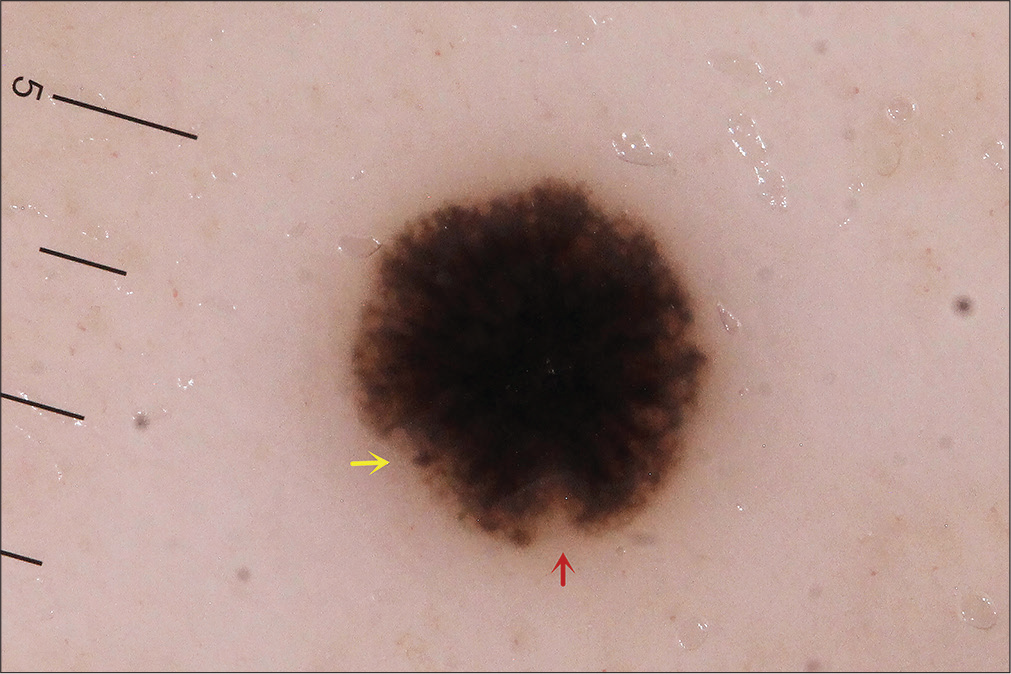
- Dermoscopy (Heine delta 20, nonpolarized, ×20) showing dark brown homogeneous pigmentation with pseudopods (yellow arrow) and abruptness of pigment patterns (red arrow), with structure asymmetry in one axis
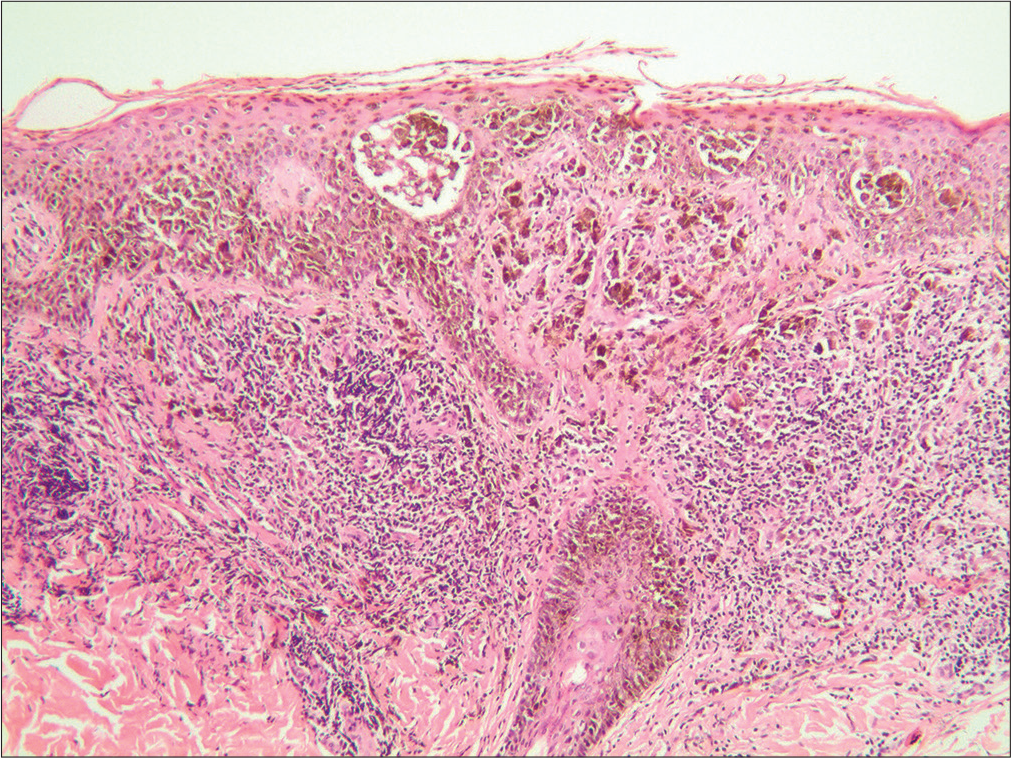
- Histopathology showing atypical melanocytes located in the epidermis and hair root sheath (H and E, ×100)
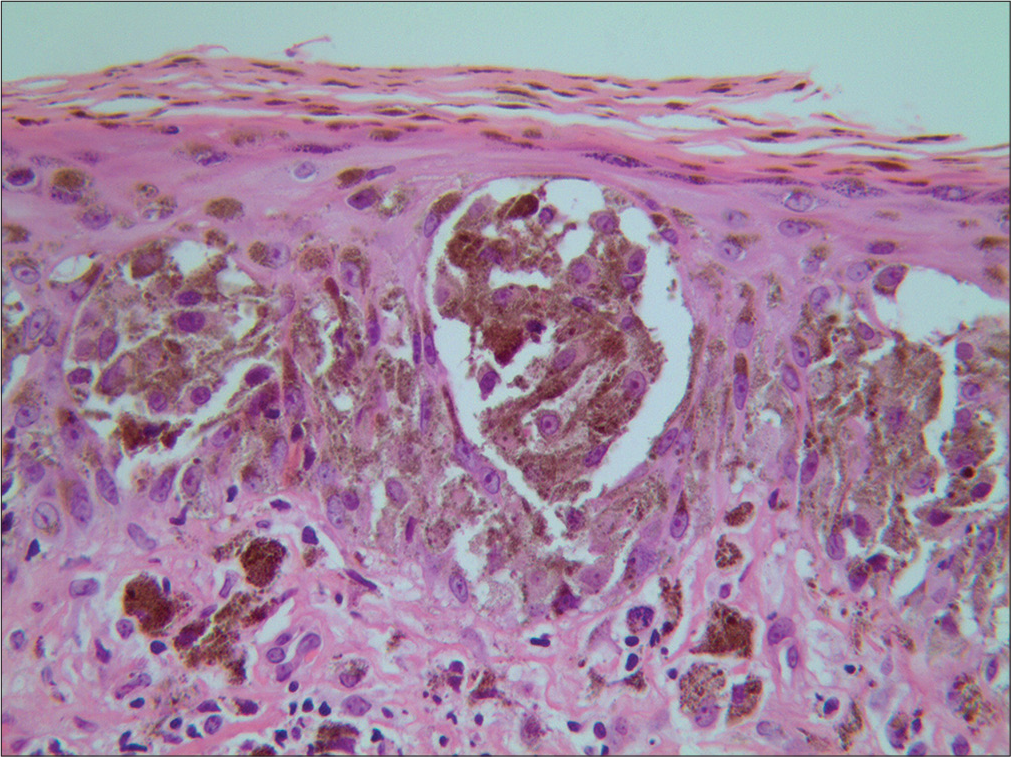
- Hyperchromatic and heteromorphic cells with a macronucleus in the epidermis (H and E, ×400)
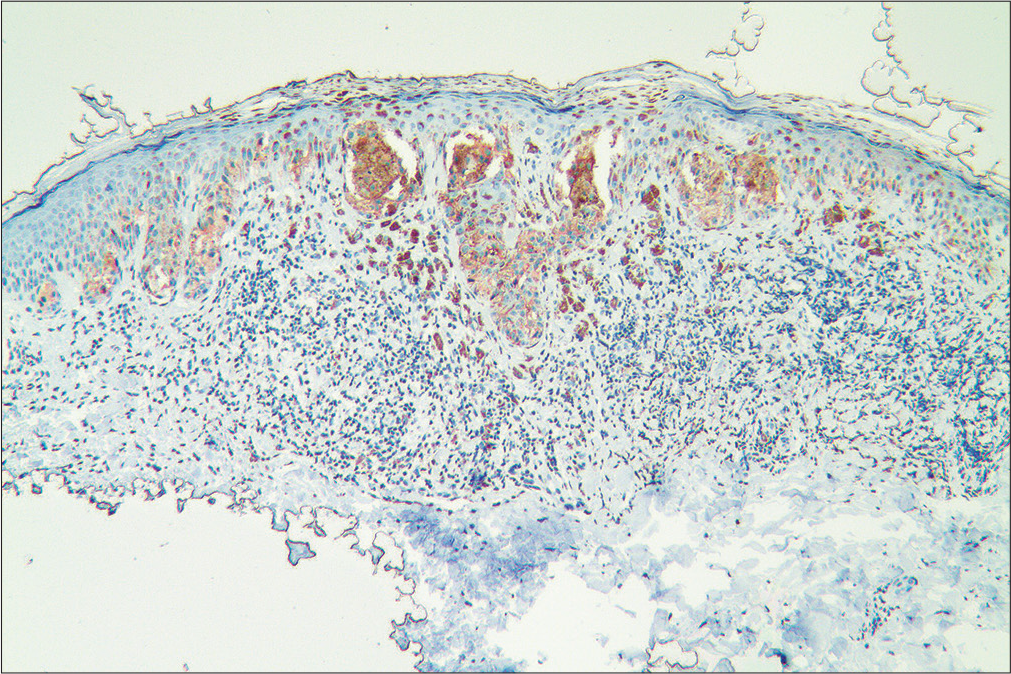
- Immunohistochemical staining with Melan A (×100)
- Immunohistochemical staining with S100 (×100)
- Immunohistochemical staining with HMB45 (×100)
Pigmented lesions are very common and mainly include melanocyte naevus, blue naevus, Spitz naevus, Reed naevus, pigmented basal cell carcinoma, seborrheic keratosis and melanoma. However, pigmented lesions are sometimes difficult to identify with the unaided eye, particularly when they are small. The acronyms ‘ABCD’ (asymmetry, border, colour, diameter) and ‘ABCDE’ (include ‘evolving’) were developed for melanoma screening. However, these criteria are not found suitable for pigmented lesions that are smaller than 5 mm in diameter. Some researchers have even suggested that pigmented lesions smaller than 5 mm cannot be considered as melanoma.1 Thus these small pigmented lesions are easily misdiagnosed in clinical practice.
Public awareness of melanoma has increased in recent decades, and patients often seek medical advice when they notice a new pigmented lesion. Therefore, more number of small melanomas have been diagnosed. In 2004, Bono et al. termed cutaneous melanomas with a maximum diameter of 3 mm as micro-melanomas.2 The main subtypes of micro-melanomas are in situ (about one-third) and Clark level II. The average age of patients with micro-melanoma is nearly a decade younger than that of those with early melanoma, implying that micro-melanoma lesions are identified several years before melanomas are usually detected.2 Early identification of micro-melanoma may greatly reduce patient mortality rate.
The typical lesion of micro-melanoma is a black macule with well-defined borders which may be symmetric or asymmetric.2 Micro-melanoma often presents as an important diagnostic challenge to the dermatologist. Dermoscopy appears to be an important aid to the diagnosis of micro-melanoma. Meta-analyses revealed that dermoscopy increases the diagnostic sensitivity of melanoma up to 25%, in comparison with the unaided eye.3 The dermoscopic features of nodular pigmented melanoma are typified by structureless blue pigmentation, predominant peripheral vessels and areas of pink and black colour. 4 Chaos (i.e., asymmetry of structure or colour) can be found in almost all algorithms, comprising asymmetry, irregular blotch, bizarre pattern or an atypical network.5 However, chaos is not 100% specific or sensitive for melanoma. A small portion of nodular melanomas (5.8%) are not chaotic in either structure or colour. With the wide use of dermoscopy, an increasing number of patients with micro-melanoma have been identified. To the best of our knowledge, a total of 23 cases of micro-melanoma identified via dermoscopy imaging have been reported to date [Table 1], and the smallest melanoma identified with dermoscopic images was 1.5 mm in diameter.6 Pseudopods, radial streaming and irregular network were the mainly observed dermoscopic features (in more than a quarter of patients). The frequency of pseudopods (11/24), radial streaming (7/24), and irregular network (6/24) in micro-melanoma had no significant statistical differences (χ2 = 1.27, P = 0.53). In addition, no significant difference was observed in these dermoscopic features between micro-melanomas in situ and invasive melanomas.
| Number | Diameter (mm) | Color | Type | Clark level | Blue-grey veil | Pseudopods | Radial streaming | Irregular blasck dots | Red dots | Irregular network | Other | Chaos | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 3 | Black | In situ | I | √ | √ | Not mentioned | Bono A, et al. Micro-melanoma detection. A clinical study on 22 cases of melanoma with a diameter equal to or less than 3 mm. Tumori 2004;90:128-31. | |||||
| 2 | 3 | Black | In situ | I | √ | Not mentioned | |||||||
| 3 | 3 | Black | In situ | I | √ | √ | Not mentioned | ||||||
| 4 | 3 | Black-tan | In situ | I | √ | √ | Not mentioned | ||||||
| 5 | 3 | Tan-whitish | In situ | I | √ | Not mentioned | |||||||
| 6 | 2 | Black | Invasive | II | √ | Not mentioned | |||||||
| 7 | 3 | Black-grey | Invasive | II | √ | Not mentioned | |||||||
| 8 | 3 | Black | Invasive | II | √ | Not mentioned | |||||||
| 9 | 3 | Black | Invasive | II | √ | √ | Not mentioned | ||||||
| 10 | 3 | Black | Invasive | II | √ | Not mentioned | |||||||
| 11 | 3 | Black-brown | Invasive | II | √ | Not mentioned | |||||||
| 12 | 3 | Black | Invasive | II | √ | √ | Not mentioned | ||||||
| 13 | 3 | Brown | Invasive | II | √ | √ | Not mentioned | ||||||
| 14 | 3 | Brown-pink | Invasive | II | √ | √ | Not mentioned | ||||||
| 15 | 3 | Black-brown | Invasive | II | √ | √ | √ | Not mentioned | |||||
| 16 | 3 | Brown | Invasive | II | √ | √ | Not mentioned | ||||||
| 17 | 3 | Not mentioned | In situ | I | √ | √ | Not mentioned | Bono A, et al. Micro-melanoma detection: a clinical study on 206 consecutive cases of pigmented skin lesions with a diameter 3 mm. Br J Dermatol 2006;155:570-3. | |||||
| 18 | 1.6 | Pigmented macule | In situ | I | √ | √ | Rosendahl, et al. Dermatoscopy of a minute melanoma. Australas J Dermatol 2011;52:76-8. | ||||||
| 19 | 1.6 | Pigmented macule | In situ | I | √ | √ | √ | equivocal asymmetry | Pellizzari et al. A tiny invasive melanoma: a case report with dermatoscopy and dermatopathology.Dermatol Pract Concept 2013;3:49-51. | ||||
| 20 | 2 | Pigmented macule | In situ | I | Blueness | √ | Paul SP. Micromelanomas: A review of melanomas ≤2 mm and a case report. Case Rep Oncol Med 2014;2014:206260. | ||||||
| 21 | 1.5 | Darkly pigmented | In situ | I | Brown pigmented, structureless | √ | Rosendahl, et al. Diagnosis of a minute melanoma assisted by automated multi-camera-array total body photography. Australas J Dermatol 2016;57:242-3. | ||||||
| 22 | 1.7 | Pigmented lesion | In situ | I | Grey structures | √ | √ | Fomiatti, et al. Dermatoscopic chaos of border-abruptness led to diagnosis of a minute melanoma. Australas J Dermatol 2019;60:e62-4. | |||||
| 23 | 2 | Brown | In situ | I | Hyperpigmented areas | √ | Lallas, et al. A tiny melanoma: The beginning of a life. Dermatol Pract Concept 2019;9:207-8. | ||||||
| 24 | 2.3 | Black | In situ | I | √ | √ | Starburst pattern | √ | |||||
√: positive for this feature
The presence of chaos had a higher sensitivity for the detection of melanoma, as observed in six of the seven described patients.The lesion in the present case was small and symmetrical when visualised with the unaided eye, but the time of onset and the nature of evolution were unknown. The patient also had no personal or family history of melanoma. Dermoscopy revealed that the lesion had a typical starburst pattern, dark brown homogeneous pigmentation with pseudopods and abruptness of pigment patterns at the periphery which was monochromatic and asymmetrical in one axis. The starburst pattern is mainly observed in benign diseases such as blue naevus, Spitz naevus and Reed naevus, but rare in melanoma. Considering the dark colour and incomplete symmetry of the lesion under dermoscopy, melanoma was suspected. A biopsy was performed, which confirmed the diagnosis of melanoma. The patient underwent complete surgical resection, with no recurrence over the 1-year follow-up period.
This finding emphasises that there need not be an association between the size of the pigmented lesions and the diagnosis of melanoma. Presence of asymmetry or the criteria like ABCD or ABCDE and a variety of dermoscopic algorithms can be used for melanoma screening, but they may not be suitable for all patients. Hence clinicians should be vigilant when encountering such small pigmented lesions, particularly new onset black lesions. So it is important that such suspicious lesions must be biopsied and subjected to histopathological examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by the Social Development Project of Zhenjiang (SH2018074).
Conflicts of interest
There are no conflicts of interest.
References
- Diagnosis of early malignant melanoma: Sensitivity and specificity of clinical and histological criteria In: Elder DE, ed. Pathobiology of Malignant Melanoma. Basel: Karger; 1987. p. :96-106.
- [Google Scholar]
- Micro-melanoma detection. A clinical study on 22 cases of melanoma with a diameter equal to or less than 3 mm. Tumori. 2004;90:128-31.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: A meta-analysis of studies performed in a clinical setting. Br J Dermatol. 2008;159:669-76.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented nodular melanoma: The predictive value of dermoscopic features using multivariate analysis. Br J Dermatol. 2015;173:106-14.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of neoplastic skin lesions: Recent advances, updates, and revisions. Curr Treat Options Oncol. 2018;19:56.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of a minute melanoma assisted by automated multi-camera-array total body photography. Australas J Dermatol. 2016;57:242-3.
- [CrossRef] [PubMed] [Google Scholar]





