Translate this page into:
Nevus of Ota: A series of 15 cases
2 Department of Ophthalmology, Kasturba Medical College, Mangalore, Karnataka, India
Correspondence Address:
Shanmuga Sekar
301-D, KMC Gents hostel, Falnir, Mangalore, Karnataka
India
| How to cite this article: Sekar S, Kuruvila M, Pai HS. Nevus of Ota: A series of 15 cases. Indian J Dermatol Venereol Leprol 2008;74:125-127 |
Abstract
Background: The nevus of Ota is a dermal nevus characterized by bluish pigmentation in the distribution of the first and the second division of the trigeminal nerve. Aim: Our aim was to study the cutaneous and extracutaneous manifestations of the nevus of Ota. Methods: A total of 15 cases were included in our study. A detailed history, clinical examination along with direct ophthalmoscopy and otoscopy were done for all the cases. Results: Most of the patients (60%) had lesions at birth and the majority (86.7 %) were females. Five (33.3%) patients belonged to Tanino class II. Combined dermal and ocular involvement was observed in 60% of the cases. Conclusion: Tanino class II was the most common type observed in our studies. A few rarer associations such as nevus of Ito and hemangioma were also noted in our patients.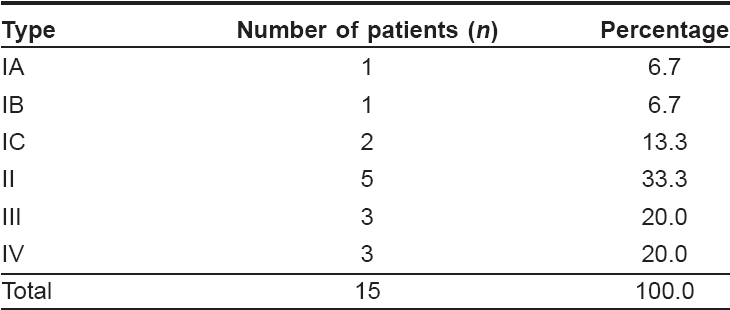
 |
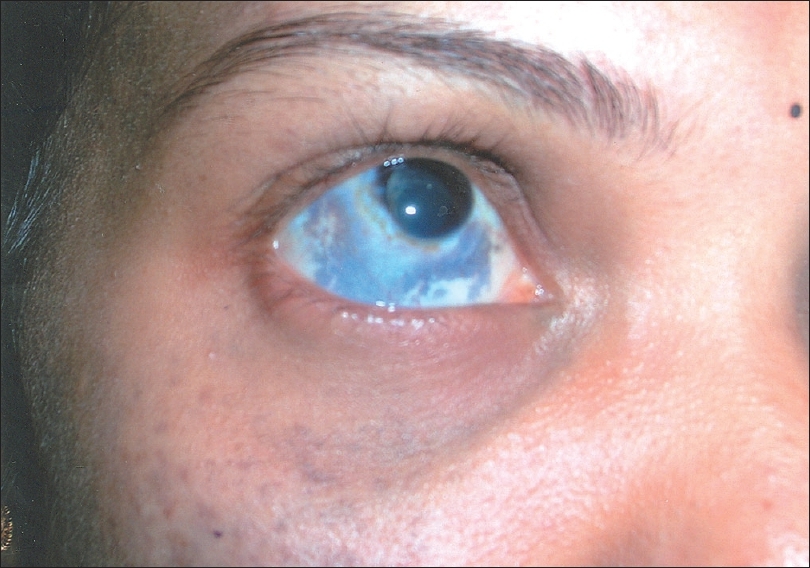
| Figure 2: Nevus of Ito in a patient with nevus of Ota |
 |
| Figure 2: Nevus of Ito in a patient with nevus of Ota |
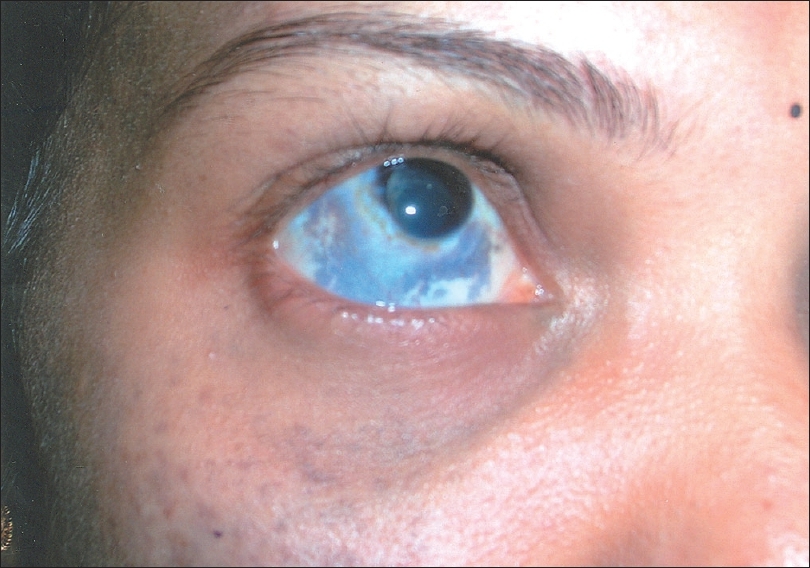 |
| Figure 1: Episcleral involvement in nevus of Ota |
 |
| Figure 1: Episcleral involvement in nevus of Ota |
Introduction
The term ceruloderma [1] was first introduced in 1980 to describe various clinical syndromes characterized by melanin and nonmelanin pigmentation of the dermis. The nevus of Ota consists of hyperpigmentation of facial skin and mucous membranes in the distribution of the ophthalmic, maxillary and occasionally, the mandibular divisions of the facial nerve. [2] The dermal lesions are bluish, confluent, nonhairy, flat, pigmented macules with poorly defined margins. The melanocytosis also affects the oral cavity, nasal mucosa, external auditory canal, tympanic membrane, orbital fissures, meninges and the brain. [3] Tanino [4] has classified the nevus of Ota into four types:
Type I.
IA. Mild orbital type: Distribution over the upper and lower eyelids, periocular and temple region.
IB. Mild zygomatic type: Pigmentation is found in the infrapalpebral fold, nasolabial fold and the zygomatic region.
IC. Mild forehead type: Involvement of the forehead alone.
ID . Involvement of ala nasi alone.
Type II.
Moderate type: Distribution over the upper and lower eyelids, periocular, zygomatic, cheek and temple regions.
Type III. The lesion involves the scalp, forehead, eyebrow and nose.
Type IV. Bilateral type: Both sides are involved.
We studied the clinical features of 15 cases of nevus of Ota.
Methods
The study was conducted for a period of 24 months from August 2004 to July 2006. The study population included patients attending Government Wenlock Hospital and Kasturba Medical College, Mangalore. A total of 15 cases were included in the study. A detailed history regarding the age of onset, site of lesion, duration and any past treatment were obtained. Detailed dermatological and systemic examinations were carried out along with examination of the eyes, oral cavity and ears. Wood′s lamp examination was also done. Direct ophthalmoscopy to visualize pigmentation in the retina and otoscopy for tympanic membrane involvement was also done for all cases.
Results
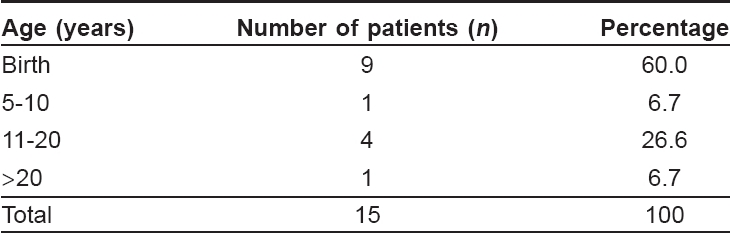
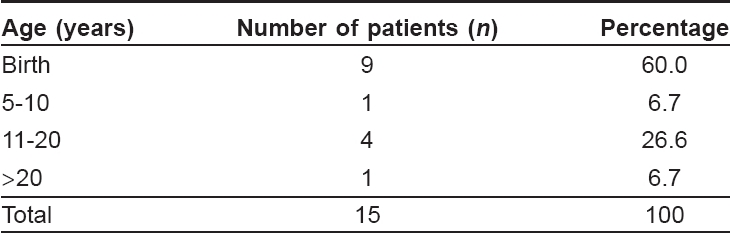
Out of the 15 cases, nine (60%) patients presented in their third decade of life followed by three (20%) in their fourth decade. The youngest patient was eight years old and the oldest was 37 years old. The majority of the cases [13 (86.7%)] was female. The female: male ratio were 6.5:1. The lesions were present at birth in nine (60%) cases [Table - 1] while in four (26.6%), they appeared in the second decade of life. Only one (6.7%) patient had a history of similar lesions in the family.
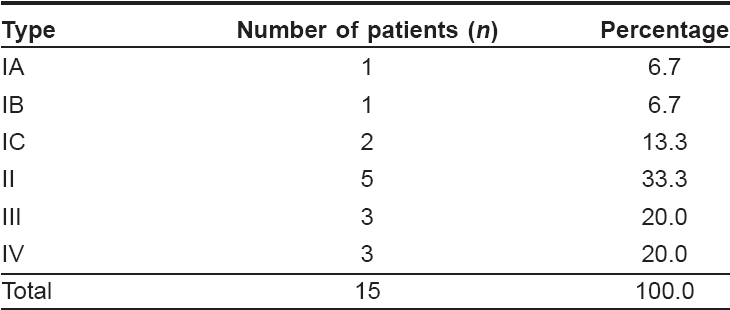
Five patients [Table - 2] belonged to Tanino class II while three belonged to class III and three to class IV. There were no patients in class ID. Dermal and ocular involvement was observed in nine (60%) cases while dermal involvement alone was observed in six (40%) cases. Of the nine cases with ocular involvement, all had bluish pigmentation in the episclera [Figure - 1] while three (33%) had involvement of the palpebral conjunctiva and three of the retina. The alae nasi and hard palate were involved in three (20%) each. None of the patients had any involvement of the tympanic membrane. The nevus of Ito [Figure - 2] and a deviated nasal septum were separately observed in two (13.4%) cases. Hemangioma with glaucoma was observed in a patient with bilateral nevus of Ota.
Discussion
Hulkey first described oculodermal melanosis in 1861 and in 1916, Pusey was the first to draw attention to the relationship of a pigmented lesion of facial skin to the pigmentation of ipsilateral sclera in a Chinese student. In 1939, Ota and Tanino described several cases of pigmented nevus of the skin and eye and named them "nevus fuscoceruleus ophthalmomaxillaris of Ota." Melanocytes move from the neural crest to the skin during early embryonic life. Failure of complete migration into the epidermis before birth with ensuing dermal nesting and melanin production produces characteristic blue patches. Dermal melanin produces blue color because of the Tyndall effect in which all but the blue end of the light spectrum penetrates into the deep dermis and is absorbed by dermal melanin. Sex hormones have been implicated in the pathogenesis of the nevus of Ota.
Out of our 15 cases, nine presented in the third decade of life while four were in their fourth decade. The age of the patients varied between eight and 37 years. The mean age in our study was 23 years and the majority of the patients were females. There were only two (13.3%) males in our study. In a study by Teekhasaenee et al. [5] 147/194 (76%) nevus of Ota cases were females. In our study, nine (60%) patients had lesions at birth, which was consistent with a study by Kopf et al. [6] Hidano et al. [7] reported two peaks of onset - one at birth and the other in the second decade of life. It was proposed that stress and trauma may be accompanied by increased secretion of propiomelanocortin, a precursor of melanocyte-stimulating hormone. Under these conditions, a small unnoticed cell nest could be stimulated to enlarge in size. One patient gave a history of similar lesions in her grandfather. Very few instances of familial occurence have been reported. Trese et al. [8] and Teekhasaenee et al. [5] have reported familial incidence in their studies.
In our study, five (33.3%) cases belonged to Tanino class II while three (20%) each belonged to classes III and IV. In a study by Teekhasaenee et al. [5] 27% each belonged to classes II and III. Blue colored lesions were observed in 13 of our patients while two had slate grey lesions. The color of the lesions depends upon the depth of involvement. The deeper lesions appear blue in color due to the Tyndall effect whereas the more superficial lesions are slate grey in color. The grey-colored lesions were examined under Wood′s lamp, which caused attenuation in the intensity confirming the dermal origin.
Twelve patients (60%) had unilateral involvement while three (20%) had bilateral involvement. Bilateral involvement is rare and seen only in 4% of all cases. [5] In our study, nine (60%) patients had both ocular and dermal involvement while six (40%) had only dermal involvement. ocular involvement alone was not seen. In a study by Teekhasaenee et al. , [5] 59.3% had ocular and dermal involvement while 35% had dermal involvement. Of the nine cases with ocular involvement, all had episcleral involvement while three (33.3%) each had involvement of the palpebral conjunctiva and the retina. Teekhasaenee et al. [5] reported 100% episcleral involvement, 10% conjunctival involvement and 18% retinal involvement. Glaucoma was observed in a case of bilateral Nevus of Ota. Foulks et al. [9] and Khawly et al. [10] have reported this association. Obstruction to aqueous outflow by accumulated melanocytes is the mechanism which is most likely to be directly associated with the nevus of Ota. Palatal involvement was observed in 20% of the patients. Page et al. [11] and Rathi [12] have reported cases of Nevus of Ota with palatal involvement. None of the patients had any tympanic membrane involvement in our study.
Nevus of Ito was observed in a patient along with bilateral nevus of Ota. This association is very rare. Hidano et al. [13] has described a case of bilateral nevus of Ota with nevus of Ito with pigmentation of lips while Mukhouphaday [14] has reported a case of unilateral nevus of Ota and nevus of Ito in an Indian male. Hemangioma was observed in a patient with bilateral nevus of Ota. Reinke et al. [15] has reported a case of nevus of Ota with hemangioma and Takayasu arteritis. Neural crest cells may be disturbed by an overlying vascular malformation, thus explaining the occurrence of nevus of Ota.
To conclude, a majority of our patients of nevus of Ota presented in the third decade of life and most of them were females. Tanino class II was the most common type observed in our studies. Rare presentations observed in our study were bilateral nevus of Ota associated with Nevus of Ito and bilateral Nevus of Ota with bilateral hemangioma and glaucoma. Hence, a detailed systemic examination along with ophthalmological and oral examination is required in all cases of nevus of Ota. The psychological impact of these lesions is high and early treatment with lasers would considerably reduce the stress later in life. The lesions are usually asymptomatic but lifelong follow-up is required as a few cases of malignant melanoma have been reported in literature.
| 1. |
Fitzpatrick TB, Kukita A, Morikawa F, Seiji M, Sober AJ, Toda K. Nevus of ota. In : Biology and Diseases of Dermal pigmentation. Tokyo, Japan: University of Tokyo Press; 1981. p. 65-76.
[Google Scholar]
|
| 2. |
Ota M. Nevus fuscoceruleus ophthalmomaxillaris. Tokyo Med J 1939;63:1243-5.
[Google Scholar]
|
| 3. |
Wilcox JC. Melanamatosis of skin and central nervous system. Am J Dis Child 1939;57:391.
[Google Scholar]
|
| 4. |
Tanino H. Nevus fuscoceruleus ophthalmomaxillaris Ota. Jpn J Dermatol 1939;46:435-451.
[Google Scholar]
|
| 5. |
Teekhasaenee C, Ritch R, Rutnin U, Leelawongs N. Ocular findings in oculodermal melanocytosis. Arch Ophthalmol 1990;108:1114-20.
[Google Scholar]
|
| 6. |
Kopf AN, Weidman AI. Nevus of ota. Arch Dermatol 1962;85:195-208.
[Google Scholar]
|
| 7. |
Hidano A, Kajima H, Ikeda S, Miyasato H, Niimura M. Natural history of nevus of ota. Arch Dermatol 1967;95:187-95.
[Google Scholar]
|
| 8. |
Trese MT, Petit TH, Foos RY, Hofbauer J. Familial nevus of ota. Ann Ophthalmol 1981;13:855-7.
[Google Scholar]
|
| 9. |
Foulks GN, Shields MB. Glaucoma in oculodermal melanocytosis. Ann Ophthalmol 1977;9:1299-304.
[Google Scholar]
|
| 10. |
Khawly JA, Imami N, Shields MB. Glaucoma associated with nevus of Ota. Arch Ophthalmol 1995;113:1208-9.
[Google Scholar]
|
| 11. |
Page DG, Swirsky JA, Kaugars GE. Nevus of ota with associated palatal involvement. Oral Surg Oral Med Oral Pathol 1985;59:282-4.
[Google Scholar]
|
| 12. |
Rathi sanjay K. Bilateral nevus of ota with oral mucosal involvement. Indian J Dermatol Venereol Leprol 2002;68:104.
[Google Scholar]
|
| 13. |
Hidano A, Kajima Y, Endo Y. Bilateral nevus of Ota associated with nevus of Ito. Arch Dermatol 1965;91:357-9.
[Google Scholar]
|
| 14. |
Mukhopadhay AK. Nevus of Ota associated with nevus of Ito. Indian J Dermatol Venereol Leprol 2004;70:112-3.
[Google Scholar]
|
| 15. |
Reinke RT, Haber K, Josselson A. Ota nevus, multiple Hemangiomas and Takayasu arteritis. Arch Dermatol 1974;110:447-50.
[Google Scholar]
|
Fulltext Views
6,350
PDF downloads
1,732





