Translate this page into:
Mucocutaneous nasal histoplasmosis in an immunocompetent young adult
2 Dr. B.R. Ambedkar Centre for Biomedical Research, University of Delhi, Delhi, India
3 Division of Mycotic Diseases, Centers for Disease Control and Prevention, Atlanta, GA 30333, USA
Correspondence Address:
Harish C Gugnani
Dr. B. R. Ambedkar Centre for Biomedical Research, University of Delhi, Delhi
India
| How to cite this article: Sood N, Gugnani HC, Batra R, Ramesh V, Padhye AA. Mucocutaneous nasal histoplasmosis in an immunocompetent young adult. Indian J Dermatol Venereol Leprol 2007;73:182-184 |
Abstract
A case of mucocutaneous nasal histoplasmosis in an immunocompetent host is described below. A 30-year-old male had a broadened nose with swelling and repeated blockage of nasal passages for the past six months. Diagnosis was made on the basis of histological demonstration of characteristic yeast cells of Histoplasma capsulatum var. capsulatum occurring within histiocytes and extracellularly in stained smears of fine needle aspirates and biopsy from the lesions in ala of the nose and perioral region. The patient showed appreciable regression of lesions after three weeks of itraconazole therapy but was not available for re-assessment.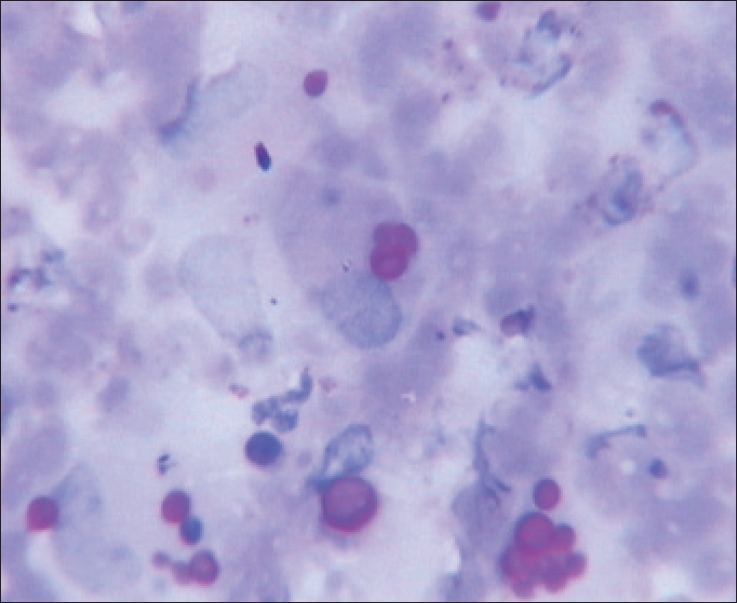 |
| Figure 2: PAS stained smear of FNA showing oval yeast cells of H. capsulatum var. capsulatum within histiocyes and extracellularly, x1250 |
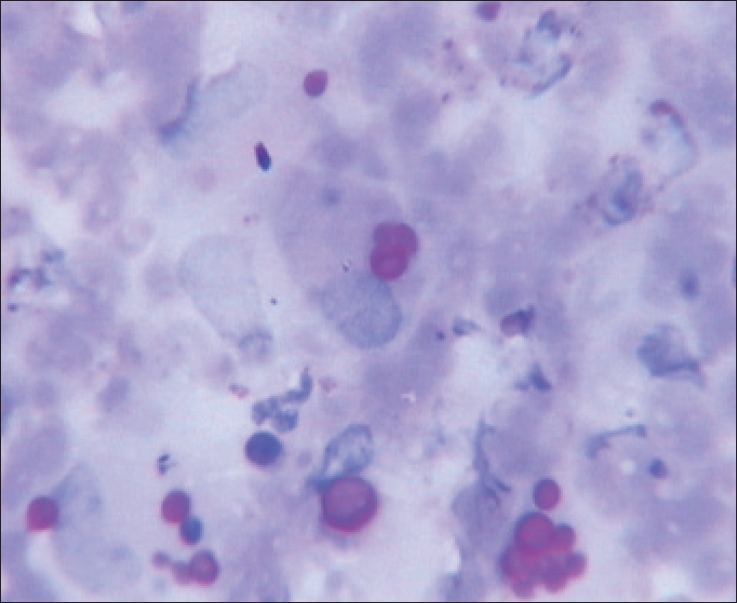 |
| Figure 2: PAS stained smear of FNA showing oval yeast cells of H. capsulatum var. capsulatum within histiocyes and extracellularly, x1250 |
 |
| Figure 1: Hypertrophic and erythematous lesions on the nose (also involving the nasal mucosa) and the surrounding facial area |
 |
| Figure 1: Hypertrophic and erythematous lesions on the nose (also involving the nasal mucosa) and the surrounding facial area |
Introduction
Histoplasmosis, a systemic mycosis caused by the dimorphic fungus, Histoplasma capsulatum var. capsulatum , is endemic in many parts of the world though it is mainly confined to the Central and Eastern part of the USA, Central and South America and South Africa. [1],[2] The clinical manifestations range from an acute pulmonary to a chronic pulmonary infection or a progressive disseminated disease. [2] On exposure to the fungus, the infection is self-limiting and restricted to lungs in 99% of the individuals with no preexisting immunological defects. The remaining 1%, however, progress to either disseminated or chronic disease involving the lungs, liver, spleen, lymph nodes, bone marrow and sometimes the skin and mucous membranes. [2] Mucocutaneous histoplasmosis is frequently reported in AIDS patients but it is rare in immunocompetent hosts. [3] This report describes a rare case of nasal mucocutaneous histoplasmosis in an immunocompetent patient.
Case Report
A 30-year-old male tailor from state of Bihar in eastern India presented with nasal swelling and recurrent blockage of nasal passages for the past six months . The swelling started as a small eruption that had enlarged in the span of a month to affect the entire nose. On examination, discrete erythematous papules were seen on the nose and right cheek. In the lower half of the nose, the eruptions had coalesced to form a large erythematous plaque with crusts resulting in a swollen and broadened nose [Figure - 1]. Removal of the crusts revealed an eroded crateriform lesion.
A fissure was seen running from the nasal tip to the posterior border of the right ala. The moustache area was affected with a few papular lesions involving the central upper lip margins on the right side. Anterior rhinoscopy showed crusts in the anterior two cm of the septum, floor of the nose and the lateral nasal wall. The turbinates were not involved. A radiograph of paranasal sinuses showed soft tissue swellings in the region of both alae of the nose without any bone destruction. There was no other abnormality in his ear-nose-throat (ENT) examination nor was there any lymphadenopathy. The patient had no other systemic or underlying disease; his chest X-ray, liver and kidney function tests, routine urine and stool examination were normal. He was non-diabetic and HIV-negative.
Hematological examination revealed hemoglobin of 11.5 gm%, a total leukocyte count of 9800/mm 3 (P67 L28 M3 E2) and ESR was 60 mm at the end of 1 hour (Westergreen). The patient was clinically diagnosed as a case of leishmaniasis or tuberculosis. May Grünwald Giemsa (MGG)-stained smears of fine needle aspirates (FNA) from the ala of the nose and perioral region showed the presence of epithelioid cell granulomas consisting of multinucleate giant cells, histiocytes and polymorphs. Extracellular and intracellular, small, oval, singly budding yeast cells (2.2-4.5 µm in diameter) with a distinct halo around them were seen within giant cells and histiocytes, a feature consistent with the tissue form of Histoplasma capsulatum var. capsulatum .
The smaller size of yeast cells and absence of broad-based or multiple budding cells ruled out Blastomyces dermatitidis and Paracoccidioides brasiliensis as etiological agents. H . capsulatum var. duboisii produces much larger yeast cells (8-15 µm in diameter), which occur predominantly in multinucleate giant cells rather than in histiocytes. Moreover, no case of human or animal infection due to H . capsulatum var. duboisii has been reported from India. Candida was also ruled out since it is observed as budding yeast cells and pseudohyphae in the infected tissue and rarely occurs intracellularly.
Smears stained by periodic acid Schiff (PAS) [Figure - 2] and Grocott methenamine silver (GMS) stains also confirmed the characteristic morphology of yeast forms.
Tissue sections of a biopsy from the lesion revealed hyperplastic epidermis with a dense chronic inflammatory infiltrate in the underlying zone. Epithelioid cell granulomas infiltrated by polymorphs were also observed. Extracellular and intracellular yeast cells with single buds attached by a narrow base, characteristic of H . capsulatum var. capsulatum were present within histiocytes as well as in multinucleate giant cells. Cultures of a portion of biopsy were attempted on Sabouraud dextrose agar and brain-heart infusion agar, both containing chloramphenicol. The etiological agent could not be isolated as the cultures were overgrown by contaminating fungi. The patient did not consent for a repeat FNA or biopsy. The patient was put on itraconazole 100 mg twice daily and partial regression of lesions was observed after nearly three weeks of treatment. The patient was thereafter lost to follow-up.
Discussion
Histoplasmosis is a sporadically reported disease in India. Randhawa et al . reviewed 37 cases of histoplasmosis from all over India until 1992. [4] In a critical overview of cases of the disease reported in India from 1968 to 1992, Padhye et al. listed 25 cases as authentically diagnosed. [5] After 1992, numerous cases of the disease have been recorded from different parts of India including the very recently reported largest series of 19 cases of disseminated infection. [6] The striking clinical manifestation in the cases of histoplasmosis known from India appears to be the predominant occurrence of mucocutaneous lesions in the oral cavity with the liver, spleen and lungs being involved only in 35% of the cases. [4],[5],[6]
A search of the reported literature on cases of histoplasmosis from India to-date showed only two cases of nasal involvement, both of them being from the state of Maharashtra, India. One was a 60-year-old male who presented with a large ulcerating mass on the left ala of the nose [7] and the other, a 55-year-old male, was a case of disseminated infection with a nodular mass on the nose. [8] The present case with primary mucocutaneous involvement of nose and adjoining facial area in an immunocompetent patient assumes significance in view of the rarity of this type of presentation in India. Though the patient had no suggestive pulmonary shadows on radiological examination, the possibility, however remote, of his having an earlier self-limited pulmonary histoplasmosis prior to mucocutaneous presentation, cannot be excluded. Amphotericin B remains the standard drug for the treatment of the acute stage of life-threatening histoplasmosis and other endemic mycoses occurring in both immunocompetent and immunocompromised hosts. Itraconazole is the drug of choice for the treatment of nonlife-threatening histoplasmosis in immunocompetent individuals. [9] The patient in this case showed good response to itraconazole but was not available for a follow-up of the treatment.
| 1. |
Mendell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 4 th ed. Churchill Livingstone Inc: New York; 1995.
[Google Scholar]
|
| 2. |
Tewari RP, Wheat LJ, Ajello L. Agents of histoplasmosis. In : Ajello L, Hay J, editors. Topley and Wison`s Microbiology and Microbial Infections. 9 th ed. Vol. 4. Arnold: London; 1998; p. 373-93.
[Google Scholar]
|
| 3. |
Souza Filho FJ, Lopen M, Almeida OP, Scully C. Mucocutaneous histoplasmosis in AIDS. Br J Dermatol 1995;33:472-4.
[Google Scholar]
|
| 4. |
Randhawa HS, Khan ZU. Histoplasmosis in India: Current Status. Indian J Chest Dis Allied Sci 1994;36:193-213.
[Google Scholar]
|
| 5. |
Padhyae AA, Pathak AA, Katyar VJ, Hazare VK, Kaufman L. Oral histoplasmosis in India: Case report and overview of the cases reported during 1968-1992. J Med Vet Mycol 1994;32: 93-103.
[Google Scholar]
|
| 6. |
Subramanian S, Abraham OC, Rupali P, Zachariah A, Mathews MS, Mathai D. Disseminated histoplasmosis. J Assoc Physicians India 2005;53:185-9.
[Google Scholar]
|
| 7. |
Talvalkar GV. Histoplasmosis simulating carcinoma: A report of three cases. Indian J Pathol Microbiol 1972;9:149-53.
[Google Scholar]
|
| 8. |
Sane SY, Patel MG, Patel BM, Kokal KK. Disseminated histoplasmosis. J Postgrad Med 1983;29:270-3.
[Google Scholar]
|
| 9. |
Lortholary O, Denning DW, Dupont P. Endemic mycoses: A treatment update. J Antimicrob Chemother 1999;43:321-31.
[Google Scholar]
|
Fulltext Views
3,032
PDF downloads
1,470





