Translate this page into:
Thin-layer rapid-use epicutaneous test (TRUE test)
Correspondence Address:
H R Jerajani
Department of Dermatology, LTM Medical College and LTM General Hospital, Sion, Mumbai - 400 022
India
| How to cite this article: Jerajani H R, Melkote S. Thin-layer rapid-use epicutaneous test (TRUE test). Indian J Dermatol Venereol Leprol 2007;73:292-295 |
 |
| Figure 1: TRUE test kit |
 |
| Figure 1: TRUE test kit |
Introduction
Contact dermatitis accounts for 10% of the patients reporting in dermatology clinics and allergic contact dermatitis contributes 30-50% of these cases. [1] The exact cause of this contact allergy must be ascertained before formulating an appropriate management program that predominantly includes an effective strategy to avoid the allergen. A properly applied and correctly interpreted patch test is currently the only scientific diagnostic method to confirm allergic contact dermatitis. [2] Proper history complements but does not substitute the patch test in diagnosing allergic contact dermatitis.
History
Individual intolerance to wood and other natural products is recognized since antiquity. In 1847, Stadler gave a detailed description of epicutaneous testing using crude antigens and a strip of blotting paper. [3] In 1895, Jadassohn introduced the application method using purified antigens that heralded modern patch testing. [3],[4] Over a period of time, patch testing techniques have evolved from the use of allergen impregnated fabric, occluded paper discs, Al test units, Finn chambers to the most recently introduced thin-layer rapid-use epicutaneous (TRUE) test.
Patch Test
Of more than 6 million chemicals in our environment, at least 2800 have contact sensitizing properties. [5] However, only a small number of these account for the majority of the contact allergies. As the frequency of the positive responses to various allergens change depending on the patient population and occupational and environmental influences, [6] a variety of screening series are available for patch testing. National and international contact dermatitis groups recommend one particular allergen series to be used for universal testing. This encompasses the allergens responsible for 70-80% of the allergic contact sensitivities in that particular region. [7],[8],[9],[10] The Contact and Occupational Dermatoses Forum of India (CODFI) has approved an Indian standard battery consisting of an array of 28 allergens. [11] Additional test series are available for fragrances, textile dyes, cosmetics and footwear.
The conventional patch test methods use inert polyethylene or aluminum chambers mounted on hypoallergenic adhesive strips as the test units. The allergens incorporated in a vehicle (usually petrolatum) are available as test preparations in preloaded syringes. An appropriate quantity of the test preparation has to be carefully placed into the chambers by the physician. It is important for the physician to use gloves while handling the test preparations to prevent contact allergy. The patches are then applied onto the back of the patient. This entire process is perceived as cumbersome and time consuming. Its accuracy is completely dependent on the skill of the physician who has to be specifically trained for performing patch tests. It is due to these reasons that patch tests are infrequently used as diagnostic aids.
The TRUE test alleviates some of the difficulties encountered in conventional patch test methods.
True Test [12]
This ready to use patch test represents a new generation of patch tests. The allergens are incorporated into hydrophilic gels coated on a water impermeable sheet of polyester and dried to a thin film. The gels themselves have low sensitizing potential, adhere to polyester backing and are compatible with most of the allergens. The gel has cellulose derivatives or a polyvinylpyrrolidone vehicle. A new hydrophilic vehicle, SOFTSAN, is expected to release allergens to a greater degree. This vehicle shows good stability for the allergens that are crystallized, micronized or emulsified into a gel. The coated polyester sheet is cut into square patches of approximately 0.81cm 2 . These are mounted on surgical tapes (5.2x13 cm). These tapes are covered with a protective sheet and packed into a pouch of laminated foil [Figure - 1].
The dry film has a thickness of approximately 3 to 20µg of allergen/cm 2 (3 to 1200µg/patch). When these patches are applied onto the skin, the film is hydrated by perspiration and it gets transformed into a gel of thickness 50-70µm from which the allergen migrates to the skin. The gel occluded with the plastic material ensures optimal contact with skin and subsequent permeation, thereby enabling high antigen bioavailability. In this manner. the allergen is evenly spread over the test area and the dose is accurately controlled. For most of the allergens, the equivalent TRUE test dose is one third of that used with the chamber method.
The patches of the TRUE test are arranged in panels of 12 allergens on a test strip. This is a very simple to use patch test system: one just opens the envelope of the laminated foil, pulls out the tape strip, removes the protective backing and applies the strip on the back. The test area should be marked with water resistant skin marker. After 48h of application, the test material is removed by the physician. The patient is asked to wait for half an hour before the readings are taken. Under optimal conditions, the test should be read at 72-96h after the application.
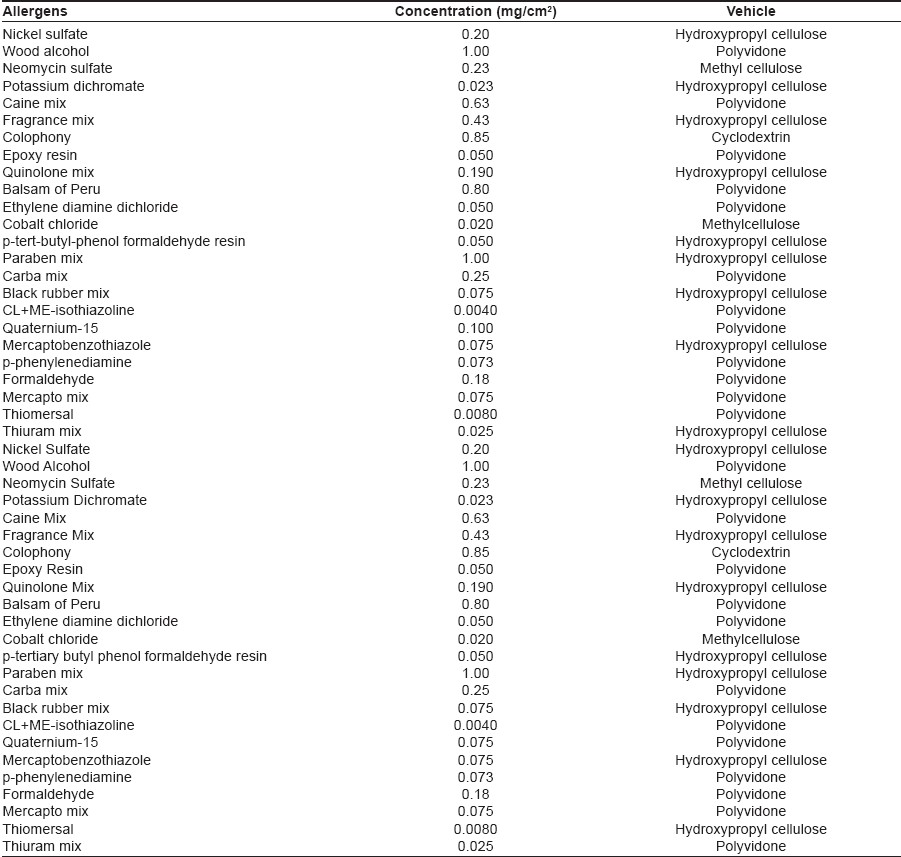
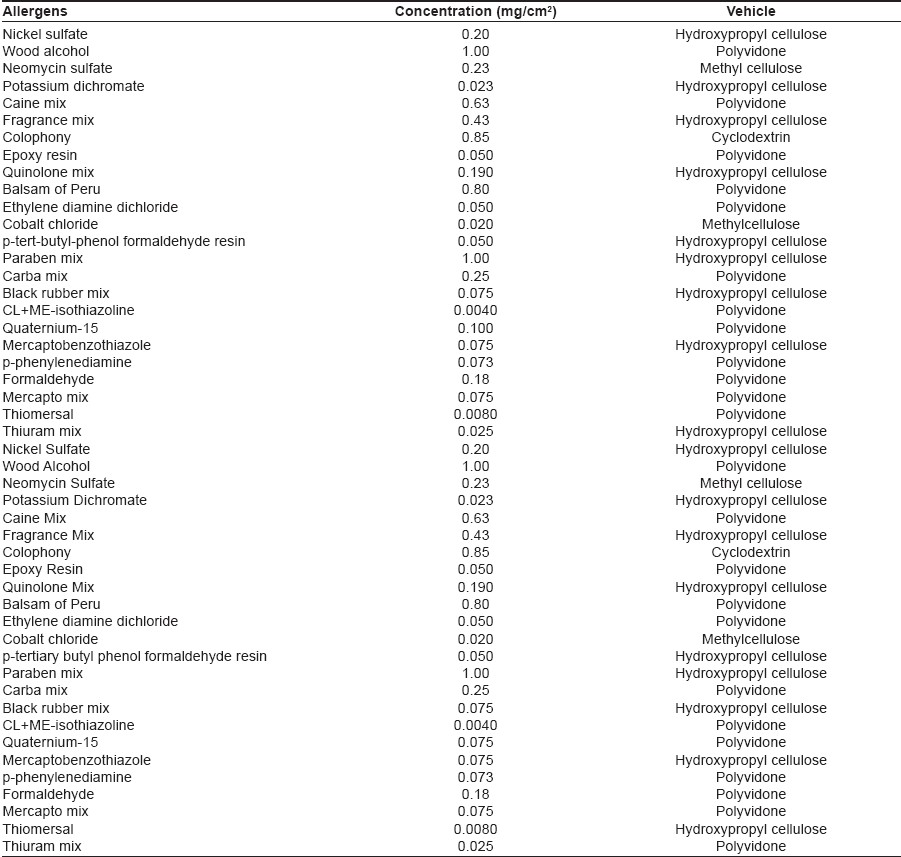
TRUE test is supplied in boxes of 10 standard tests. The 24 patches are split into two tape strips; panel 1 and panel 2, each packed in an airtight pouch. In fact, there are 23 patches containing 42 unique antigens (some of them in combination as mix patches such as carba mix, fragrance mix, etc.) [Table1]; the twenty-fourth patch is a negative control. The patches should be stored between 2 and 8°C. Shelf life under these conditions is 24 months.
Meta Analysis
The concordance of the positive reactions between TRUE tests and the Finn chamber tests, as reported by various studies, ranges from 57 to 78%. [13],[14],[15],[16],[17],[18],[19],[20],[21] The accuracy of a test reaction is defined as the relation between the patch-test reaction and the allergic sensitization of a patient to the actual allergen. The accuracy can be controlled by reproducibility of the test reaction on re-testing. [22] Although one study showed that the incidence of nonreproducible results was twice as high in the Finn chamber method than the TRUE test method, the difference between the reproducibilities in both the test systems was not statistically significant. [17]
The relevance of the test reaction is the relation between an accurate patch test reaction and the disease, and it is best confirmed by the history of the patient. [22] Based on significance-prevalence index number (SPIN), [23] an index that measures the true positivity rate of sensitivity to individual allergens; the clinically most important allergens tested by the TRUE test are nickel, cobalt, fragrance mix, colophony and thiuram mix.
There have been wide discrepancies in the reported allergen prevalences. One study found that Finn chamber method was more sensitive for the detection of allergy to fragrance mix, Balsam of Peru and thiuram mix, and the TRUE test was more sensitive for nickel and neomycin. In the studies by Lachapelle et al. and Goh et al. , Finn chamber method was superior to TRUE test in detecting the sensitivity to neomycin and the TRUE test was more effective for cobalt mix. [15],[18] Vozmediano et al. reported Finn chamber method to be superior in detecting potassium chromate, nickel and cobalt. A number of studies have shown that TRUE test performs suboptimally in the detection of fragrance allergy. Although both the methods are crucial in detecting relevant reactions to formaldehydes and carbamates, the overall better performance of the TRUE test is interesting given the use of the proallergen for formaldehyde in the TRUE test.
A meta-analysis of 15 years of TRUE test data shows that nickel (14.7%), thiomersal (5.0%), cobalt (4.8%), fragrance mix (3.4%) and Balsam of Peru (3.0%) are the most prevalent allergens. In contrast, the data from the North American Contact Dermatitis Group during the same period showed the most prevalent allergens to be nickel (14.3%), fragrance mix (14%), neomycin (11.6%), Balsam of Peru (10.4%) and thiomersal (10.4%).This suggests that clinically important data may be lost if TRUE test is used alone.
Merits and Demerits : True Test
Merits of TRUE test are as follows: (1) it is an easy, convenient, ready-to-use test. Even paramedical personnel can be easily trained to apply these patches; (2) for most of the allergens, the equivalence dose of TRUE test is 10-50% of Finn chamber dose; hence, the allergen dose per square area is lower; (3) the vehicle ensures an even spread, a correct dosage and high bioavailability of the antigen; (4) wide-spread reactions are more common with petrolatum tests because of the efflux of the test material around the test site often due to an incorrect dose. TRUE test reactions are mostly within the limits of the patch site; (5) studies have shown tape adhesiveness to be better in TRUE test; (6) consistent panel-to-panel location of each substance avoids confusion and mistakes.
Demerits of TRUE test are: (1) it is more vulnerable to washing and profuse sweating due to its hydrophilic material and minimum quantities of antigens used; (2) it is a very expensive test; (3) it is just a screening series with limited number of antigens. Important steroid antigens are not included; (4) TRUE test performs suboptimally to certain allergens, particularly fragrance mix. Hence, a patient whose dermatitis persists despite a negative test must be tested by other methods.
Conclusion
Studies have shown that TRUE test is a well standardized technique of patch testing; it is easy to handle, with few side effects and gives good accuracy. It is particularly valuable in routine clinical practice where conditions are not as well controlled as in clinical trials. However, it has its own set of pitfalls, particularly regarding the limited number of antigens currently available in its battery and the questionable predictive value of few of the antigens, as indicated by certain studies. It can best be summed up as an improved but not a perfect patch test. The hunt for the ideal patch test continues.
| 1. |
Fregert S, Hjorth N, Magnusson B, Bandmann HJ, Calnan CD, Cronin E, et al . Epidemiology of contact dermatitis. Trans St Johns Hosp Dermatol Soc 1969;55:17-35.
[Google Scholar]
|
| 2. |
Fisher AA. Practical aspects of patch testing. In : Fisher's contact dermatitis. 5 th Rietschel LR, Fowler JF Jr, editors. 5 th ed. Philadelphia: Lippincott Williams and Wilkins; 2000. p. 9-26.
th Rietschel LR, Fowler JF Jr, editors. 5 th ed. Philadelphia: Lippincott Williams and Wilkins; 2000. p. 9-26.'>[Google Scholar]
|
| 3. |
Foussereau J. History of epicutaneous testing: The blotting paper and other methods. Contact Dermatitis 1984;11:219-23.
[Google Scholar]
|
| 4. |
Sulzberger MB. The patch test- Who should and who should not use it and why. Contact Dermatitis 1975;1:117-9.
[Google Scholar]
|
| 5. |
Groot AC. Patch testing. Test concentrations and vehicles for 3700 allergens. 2 nd ed. Amstrdam: Elsevier; 1994.
[Google Scholar]
|
| 6. |
Fisher T. The art of patch testing. Contact Dermatitis 1990;23:221-3.
[Google Scholar]
|
| 7. |
Hjorth N. Routine patch tests. Trans St Johns Hosp Derm Soc 1963;49:99-107.
[Google Scholar]
|
| 8. |
Lepine EM. Results of routine office Patch testing. Contact Dermatitis 1976;2:89-91.
[Google Scholar]
|
| 9. |
Young E, Honwing RH. Patch test results with standard allergens over a decade. Contact Dermatitis 1987;17:104-7.
[Google Scholar]
|
| 10. |
Mitchell JC, Adamas RM, Glenndenning WE, Fisher A, Kanof N, Larsen W, et al . Results of patch tests with substances abandoned. Contact Dermatitis 1982;8:336-7.
[Google Scholar]
|
| 11. |
Product information. Indian Standard Battery Allergens, manufactured by Systopic Laboratories, 208, Samrat Bhawan Commercial Complex, Ranjit Nagar, New Delhi-110 008, India.
[Google Scholar]
|
| 12. |
Allergen Patch test. Thin-Layer Rapid Use Epicutaneous test. Product information 4122054. Manufactured by Melkos Laboratories A/S, Hillerod, Denmark.
[Google Scholar]
|
| 13. |
Ruhnek-Forsbeck M, Fischer T, Meding B, Pettersson L, Stenberg B, Strand A, et al . Comparative Multi centre study with TRUE test and Finn Chamber patch test methods in eight Swedish Hospitals. Acta Derm Venerol 1988;68:123-8.
[Google Scholar]
|
| 14. |
TRUE test study group: Comparative multi-centrer studies with TRUE test and Finn chambers in eight Swedish hospitals. J Am Acad Dermatol 1989;21:646-9.
[Google Scholar]
|
| 15. |
Lachapelle JM, Bruynzeel DP, Ducombs G, Hannuksela M, Ring J, White IR, et al . European Multi center study of TRUE test. Contact Dermatitis 1988;19:91-7.
[Google Scholar]
|
| 16. |
Wilkinson JD, Bruynzeel DP, Ducombs G, Frosch PJ, Gunnarsson Y, Hannuksela M, et al . European multi center study of TRUE test, Panel 2. Contact Dermatitis 1990;22:218-25.
[Google Scholar]
|
| 17. |
Gollhausen R, Przybilla B, Ring J. Reproducibility of Patch test results: Comparison of TRUE test and Finn Chamber test results. J Am Acad Dermatol 1989;21:843-6.
[Google Scholar]
|
| 18. |
Goh CL. Comparative study of TRUE test and Finn chamber patch test techniques in Singapore. Contact Dermatitis1992;27:84-9.
[Google Scholar]
|
| 19. |
Fernandez-Vozmediano JM, Hita JC. Concordance and discordance between TRUE test and Finn Chamber. Contact Dermatitis 2000;42:182-3.
[Google Scholar]
|
| 20. |
Preliminary studies of the TRUE test patch system in the United States: TRUE test study group. J Am Acad Dermatol 1989;21:841-3.
[Google Scholar]
|
| 21. |
Prue C, Martinson ME, McAnally PM, Stagner WC. Post marketing survey results of TRUE test, a new allergen patch test. Am J Contact Dermat 1998;9:6-10.
[Google Scholar]
|
| 22. |
Fischer MD, Maibach HI. Easier Patch testing with TRUE test. J Am Acad Dermatol 1989;20:447-53.
[Google Scholar]
|
| 23. |
Maoud M, Fleischer AB Jr, Sherertz EF, Feldman SR. Significance Prevalence Number: A reinterpretation and enhancement of data from the North American Contact Dermatitis Group. J Am Acad Dermatol 1999;41:573-6.
[Google Scholar]
|
Fulltext Views
10,061
PDF downloads
2,271





