Translate this page into:
Vitiligo: A sign of systemic disease
Correspondence Address:
Richard H Huggins
Department of Dermatology, New Jersey Medical School, 185 South Orange Avenue, Newark, NJ 07103-2714
USA
| How to cite this article: Huggins RH, Janusz CA, Schwartz RA. Vitiligo: A sign of systemic disease. Indian J Dermatol Venereol Leprol 2006;72:68-71 |
Abstract
Vitiligo reflects a systemic process that has important implications beyond the skin. These include other autoimmune diseases and ocular and neurological abnormalities. Alezzandrini syndrome and Vogt-Koyanagi-Harada syndrome particularly exemplify this relationship. In addition, vitiligo may be confused with other systemic disorders, including tuberous sclerosis, progressive systemic sclerosis (scleroderma), melanoma, and, in endemic regions, leprosy. We describe these associations and emphasize the importance of depigmenting disorders.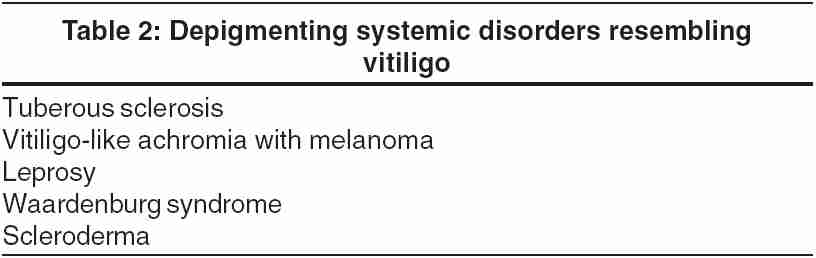


Vitiligo suggests a systemic disease that can extend beyond the skin. It may be linked with Hashimoto′s thyroiditis, diabetes mellitus, Addison′s disease, and other autoimmune processes. It may be associated with ocular abnormalities, exclusively, or as part of a constellation of symptoms, as it is in Alezzandrini syndrome or Vogt-Koyanagi-Harada (VKH) syndrome. Vitiligo should be distinguished from systemic disorders with skin changes resembling it.
SYSTEMIC MELANOCYTIC DESTRUCTION
Melanocytes are present not only within the skin and hair follicles, but also in the eyes and other parts of the central nervous system. As a result, vitiligo can be encountered alongside other melanocyte-related pathologies. Ocular findings, such as uveitis and major fundal pigmentary abnormalities, may be observed in as many as 66% of patients with vitiligo.[1] These signs include hypopigmented spots on the iris (23%), pigmentation on the anterior chamber (18%), retinal pigment epithelium hypopigmentation (9%), uveitis (5%), and chorioretinal degeneration (11%). There is usually no loss of visual acuity, so clinicians managing patients with vitiligo need to have a high index of suspicion. Chorioretinitis can often be diagnosed by detection of choroid or retinal pigmented epithelial lesions typical of this pathology.[2] The most specific sign of chorioretinitis, however, is the finding of a characteristic focal scar. The cutaneous loss of melanocytes is often accompanied by a similar depigmentation of the two pigment layers of the retina. This causes the retina to have alternating whitish streaks, coming from capillaries being visualized through the depigmented patches, and darkened areas of normal choroid pigment. As a result, the retina may have a tigroid appearance on ophthalmological examination. Alternatively, if a reactive proliferation of glial cells is triggered by choroid destruction, a homogeneous, yellowish discoloration of the retina may result.
In addition to ocular pathologies, other neurological abnormalities are associated with vitiligo in Alezzandrini and VKH syndromes. The former associates unilateral retinal degeneration, and ipsilateral vitiligo, poliosis, and, possibly, hearing abnormalities.[3] The process is thought to be initiated by either a viral or an autoimmune process. The initial complaint is usually a gradual loss of visual acuity in one eye. Facial vitiligo and poliosis of the eyebrows and eyelashes usually develop several years after the ocular insult. In VKH, bilateral ocular alterations are associated with neurological and cutaneous disturbances [Table - 1].[4] Usually limited to uveitis, in severe cases, the ocular pathology may progress to bilateral retinal detachment. Neurological abnormalities include tinnitus, vertigo, headache, and meningoencephalitis. Vitiligo and poliosis, as well as alopecia areata, are all possible cutaneous disturbances. The initiating event may be a cutaneous insult, such as generalized erythema or a physical trauma to the skin. The disease process usually begins in the meningoencephalic phase, which has primarily neurologic symptoms, advances to the ophthalmic phase, in which retinal detachment may occur, and ends in the convalescent phase, where the cutaneous pathologies develop.
AUTOIMMUNE DISORDERS WITH VITILIGO
Vitiligo is strongly associated with a number of autoimmune disorders. Autoimmune thyroiditis is the most strongly linked, having a prevalence of 21% in cases vs 3% in controls, respectively.[5] Childhood non-segmental vitiligo is also linked with autoimmune thyroiditis, though not with any other autoimmune disease.[6] In one series, vitiligo preceded the thyroiditis by 4-35 years in nearly 50% of the subjects,[5] indicating the potential usefulness of screening. Insulin-dependent diabetes mellitus is found in 1-7% of patients with vitiligo.[7] The converse relationship is also seen, with 4.8% of all diabetic patients also having vitiligo. Addison′s disease is present in approx 2% of vitiligo patients. Pernicious anemia, systemic lupus erythematosus and, possibly, inflammatory bowel disease are also linked with vitiligo.[8] Vitiligo is also commonly seen as a component of a number of autoimmune polyendocrinopathies.[9] Autoimmune polyendocrine syndrome type I (APS-I) has a particularly strong association, with 21% of patients being afflicted with vitiligo. The classic triad of APS-I is mucocutaneous candidiasis, hypoparathyroidism, and adrenocortical insufficiency.
VITILIGO AS PART OF A SYSTEMIC REACTION
Vitiligo is one of a number of skin disorders characterized by displaying a tendency to expand into traumatized or otherwise altered skin, an occurrence known as the Koebner phenomenon. Erythroderma is a dermatitis with almost total skin involvement. It is also known as the "red man syndrome." It may represent a severe drug reaction, a flare-up of a pre-existing dermatosis, a cutaneous T-cell lymphoma (Sθzary syndrome), or may be idiopathic. A patient with a small and possibly unnoticed patch of vitiligo may koebnerize to the entire cutaneous surface as a result of a cutaneous insult in the form of erythroderma.[10]
In the absence of pre-existent vitiligo, induction may occur secondary to a reaction to a variety of compounds. Vitiligo may be induced by chemicals typically from an occupational exposure to phenolic germicides.[2] It is unclear whether use of certain oral medications may also be associated with vitiligo. For example, as infliximab has been known to produce a lupus-like syndrome; it has also been described as inducing vitiligo, probably through the same or similar autoimmune mechanism.[11]
DEPIGMENTATION RESEMBLING VITILIGO IN SYSTEMIC DISEASES
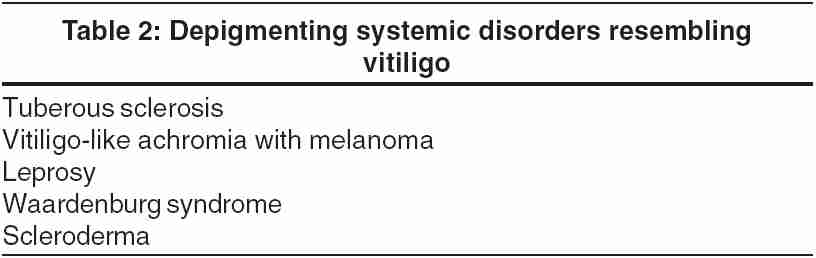
There are many similarities in the clinical appearances of vitiligo and melanoma-associated vitiliginous change, piebaldism of Waardenburg syndrome, diffuse scleroderma and tuberous sclerosis [Table - 2]. To diagnose vitiligo, one should be able to differentiate among a complete absence of pigment, hypopigmentation, and normal skin. Wood′s lamp examination can be helpful, especially with light-complexioned patients.[12] Vitiligo is the most likely diagnosis in cases in which there is a progressive depigmentation leading to symmetrically distributed, chalk-white macules on the face, neck, scalp, mucous membranes, or periorificial areas, and not accompanied by any other symptom.[13] In other cases the diagnosis may be more difficult. Characteristic systemic signs and symptoms as well as histological examination may be helpful in making the proper diagnosis.
Waardenburg syndrome is a rare autosomal-dominant disorder associated with piebaldism.[14] Affected individuals often have hypomelanotic macules. These may be differentiated from vitiliginous macules by the variability of the pigmentation of the lesions (ranging from amelanotic to hyperpigmented), their distribution (typically sparing the hands, feet, and periorificial areas), stability, and tendency to be congenital. Systemic components of Waardenburg syndrome include bilateral congenital deafness, heterochromic irides, a broadened nasal root, and a white forelock.
Tuberous sclerosis (TS) may be first evident through the appearance of characteristic depigmented spots.[15] TS macules are usually hypomelanotic, as opposed to chalk-white, have an ash-leaf shape, and may have a segmental distribution. They may be seen in a confetti-like pattern that is difficult to differentiate from vitiligo. The course of these ash-leaf lesions differs from that of vitiliginous ones in that these TS stigmata are congenital or develop within the few years of life, and remain stable. In TS, there is hamartoma formation in many organs, resulting in numerous systemic abnormalities, including low intelligence, epilepsy, and pituitary adrenal dysfunction.[16] A child with seizures may need to be examined in Wood′s light to detect any ash-leaf spots.
Sometimes, collagen vascular disorders may be associated with hypopigmentation. Diffuse scleroderma may result in areas of skin hyper- or hypopigmentation.[17] The presence of macules with any degree of pigmentation or macules with varied pigmentation would favor this diagnosis over vitiligo. A confetti-like pattern of depigmentation may also be seen with this disease, necessitating differentiation from confetti vitiligo. Systemic signs of the disease include essential vasomotor disturbances, such as Raynaud′s phenomenon, fibrosis, and abnormalities of the lungs, kidneys, digestive system, and heart. Discoid plaques of lupus erythematous may also appear, markedly devoid of pigmentation, but atrophy is usually evident.
Vitiligo may develop in patients with melanoma. The same process, autoimmune destruction of melanocytes, is thought to be responsible for both melanoma-associated vitiliginous depigmentation and common vitiligo.[18] They appear identical histologically. As immune system effectors circulate freely in the plasma, the sites of depigmentation do not necessarily have to be near the actual melanoma and, in fact, can be quite distant from it. The major difference between vitiligo resulting from melanoma and common vitiligo is the distribution. The former is said to usually begin centrally, on the chin, neck, and trunk, for example, and spread to the periphery. Generalized vitiliginous lesions usually begin distally, on the hands and feet, and then advance to involve the trunk.[19] Systemic signs and symptoms are not usually useful in differentiating them. Both common vitiligo vulgaris and melanoma-associated vitiligo may have uveitis and poliosis.
| 1. |
Biswas G, Barbhuiya JN, Biswas MC, Islam MN, Dutta S. Clinical pattern of ocular manifestations in vitiligo. J Indian Med Assoc 2003;101:478-80.
[Google Scholar]
|
| 2. |
Huggins RH, Janniger CK, Schwartz RA. Vitiligo. Acta Dermatovenerol Alp Panonica Adriat 2005;14: 137-45.
[Google Scholar]
|
| 3. |
Janniger CK, Koziorynska EI. Alezzandrini's syndrome. eMedicine Dermatology. Last updated 2.12.2005. http://author.emedicine.com/derm/topic728.htm Last accessed 20.12.2005.
[Google Scholar]
|
| 4. |
Federman DG, Kravetz JD, Ruser CB, Judson PH, Kirsner RS. Vogt-Koyanagi-Harada syndrome and ulcerative colitis. South Med J 2004;97:169-71.
[Google Scholar]
|
| 5. |
Zettinig G, Tanew A, Fischer G, Mayr W, Dudczak R, Weissel M. Autoimmune diseases in vitiligo: do anti-nuclear antibodies decrease thyroid volume? Clin Exper Immunol 2003;131:347-54.
[Google Scholar]
|
| 6. |
Iacovelli P, Sinagra JL, Vidolin AP, Marenda S, Capitanio B, Leone G, et al . Relevance of thyroiditis and of other autoimmune diseases in children with vitiligo. Dermatology 2005;210:26-30.
[Google Scholar]
|
| 7. |
Ortonne JP, Bahadoran P, Fitzpatrick TB, Mosher DB, Hori Y. Hypomelanoses and Hypermelanoses. In: Fitzpatrick's Dermatology in General Medicine. Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, editors. 6th ed. New York: McGraw Hill; 2003. p. 839-47.
[Google Scholar]
|
| 8. |
Alkhateeb A, Fain PR, Thody A, Bennett DC, Spritz RA. Epidemiology of vitiligo and associated autoimmune diseases in Caucasian probands and their families. Pigment Cell Res 2003;16:208-14.
[Google Scholar]
|
| 9. |
Hedstrand H, Ekwall O, Olsson MJ, Landgren E, Kemp EH, Weetman AP, et al . The transcription factors SOX9 and SOX10 are vitiligo autoantigens in autoimmune polyendocrine syndrome type I. J Biol Chem 2001;276:35,390-5.
[Google Scholar]
|
| 10. |
Schwartz RA, Trotter MG. Generalized vitiligo after erythroderma. Dermatologica 1983;167:42-6.
[Google Scholar]
|
| 11. |
Ramνrez-Hernαndez M, Marras C, Martinez-Escribano JA. Infliximab-induced vitiligo. Dermatology 2005;210:79,80.
[Google Scholar]
|
| 12. |
Schwartz RA. Superficial fungal infections. Lancet 2004;364:1173-82.
[Google Scholar]
|
| 13. |
Schwartz RA. Pigmentary disorders. In: Rakel RE, Bope ET, editors. Conn's Current Therapy 2005. Philadelphia: WB Saunders; 2005. p. 995-9.
[Google Scholar]
|
| 14. |
Dourmishev AL, Dourmishev LA, Schwartz RA, Janniger CK. Waardenburg syndrome. Int J Dermatol 1999;38:656-63.
[Google Scholar]
|
| 15. |
J�zwiak S, Schwartz RA, Janniger CK, Bialicka-Cymerman J. The usefulness of diagnostic criteria of tuberous sclerosis complex in pediatric patients. J Child Neurol 2000;15:652-9.
[Google Scholar]
|
| 16. |
J�zwiak S, Schwartz RA. Dermatologic and stomatologic manifestations of tuberous sclerosis. In : Curatolo P, editor. Tuberous Sclerosis Complex: From Basic Science to Clinical Phenotypes. London: International Child Neurology Association. Mac Keith Press; 2004. p. 136-69.
[Google Scholar]
|
| 17. |
Schwartz RA, Dziankowska-Bartkowiak B, Zalewska A, Sysa-Jedrzejowska A. Systemic sclerosis. eMedicine Dermatology. Last updated 23.08.2005. http://emedicine.com/derm/topic677.htm. Last accessed 20.12.2005.
[Google Scholar]
|
| 18. |
Yee C, Thompson JA, Roche P, Byrd DR, Lee PP, Piepkorn M, et al . Melanocyte destruction after antigen-specific immunotherapy of melanoma: direct evidence of t cell-mediated vitiligo. J Exp Med 2000;192:1637-44.
[Google Scholar]
|
| 19. |
Cummings M, Nordlund JJ. Vitiligo. In : Demis DJ, editor. Clinical Dermatology. 24th ed. Philadelphia: JB Lippincott; 1997. Unit 11-33, p. 1-7.
[Google Scholar]
|
Fulltext Views
11,630
PDF downloads
3,353





