Translate this page into:
Thalidomide: Current status
Correspondence Address:
Prashasti S Shanbhag
Department of Dermatology, RGMC, CSM Hospital, Kalwa, Thane 400605, Maharashtra
India
| How to cite this article: Shanbhag PS, Viswanath V, Torsekar R G. Thalidomide: Current status. Indian J Dermatol Venereol Leprol 2006;72:75-80 |
 |
 |
Thalidomide was marketed by Chemie Grunenthal, a German company, under the brand name Contergan[1] in 1956 in Europe and Canada as a sedative and antiemetic in pregnancy. It was withdrawn in 1961 owing to its disastrous teratogenic effects. Thereafter, for a long time it remained in use only for clinical research in various dermatological and oncologic conditions. Following Sheskin′s serendipitous discovery in refractory erythema nodosum leprosum (ENL) in 1961, it was later granted approval by the US FDA in 1998. We briefly review here the pharmacological and the therapeutic profile of thalidomide.
PHARMACOLOGY
Thalidomide[1],[2],[3] is a nonpolar synthetic glutamic acid derivative. Chemically, it is an a- N -pthalimidoglutarimide consisting of a single central asymmetric carbon atom with a left pthalidimide ring and a right glutarimide ring. The pthalidimide ring is thought to be responsible for the teratogenic effects whereas the glutarimide ring, which is structurally similar to other sedatives, mediates sedation. It exists as optically active R (+) and S (-) enantiomers, which interconvert rapidly in vivo and also as an optically inactive racemic mixture. It contains four amide bonds, which are susceptible to hydrolytic cleavage. It is insoluble in ethanol and water, making intravenous formulations impossible, is lipid soluble, and crosses the placental barrier easily. Thalidomide does not appear to have any acute toxicity, making a fatal dose nearly impossible.[1]
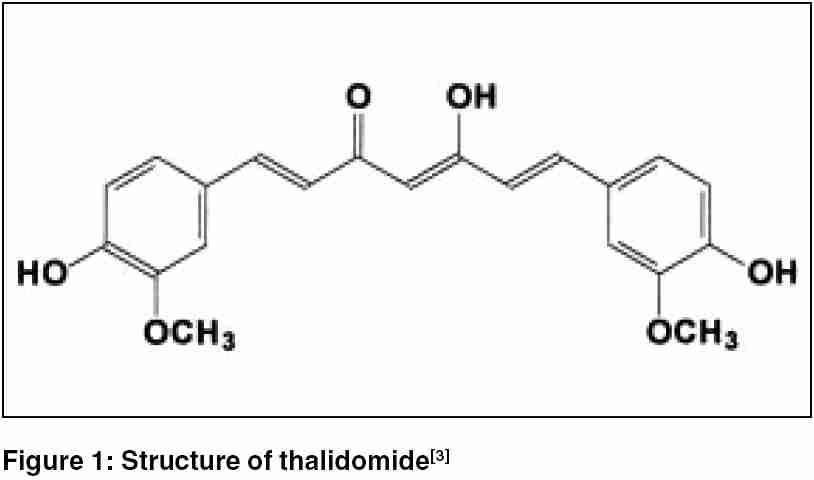
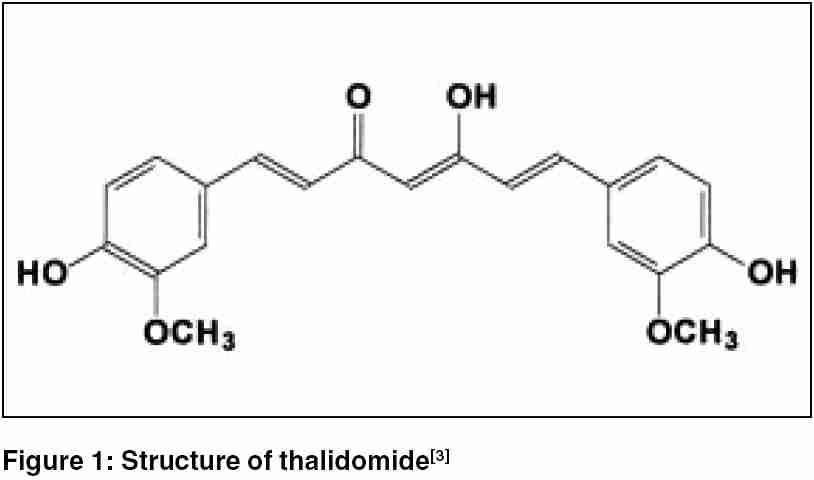
STRUCTURE
The structure[3] is described in [Figure - 1].
PHARMACOKINETICS
Thalidomide is slowly absorbed from the gastrointestinal tract.[1],[2],[3] Peak levels in blood are reached within 2-6 hours, which could be delayed with a high-fat meal. It is extensively distributed in all the tissues and fluids with higher concentrations in skin and kidneys. Bioavailability of thalidomide cannot be ascertained owing to its poor water solubility. It is primarily metabolized by nonenzymatic hydrolytic cleavage of its amide bonds. Cytochrome P-450 enzymes may have some role in metabolizing the antiangiogenic metabolite. Some of the drug is excreted in the bile, whereas less than 1% is excreted in the urine.
MECHANISM OF ACTION
The exact mechanism[1],[2],[3],[4],[5] of thalidomide′s actions is not determined. However, various theories have been proposed.
Anti-inflammatory It inhibits the chemotaxis of (and phagocytosis by) neutrophils, lymphocytes, and macrophages,[1],[2] stabilizes the lysosomal membranes,[1] and decreases the generation of superoxide and hydroxyl radicals that may cause tissue damage at sites of inflammation.[1]
Immunomodulatory effects Its main action is the inhibition of tumor necrosis factor-a (TNF-a)[1] by enhancing the degradation of its m-RNA.[2],[3] It also inhibits the production of Interferon-a and interleukin-12.[1],[2] It enhances the production of Th-2 cytokines such as IL-4 and IL-5, and also IL-2 which may counteract TNF-a and IFN-g. Thalidomide also suppresses formation of IgM antibodies,[1],[2] decreases circulating helper T-cells, and increases suppressor T-cells.[1],[2],[5] It inhibits cellular immunity by blocking lymphocyte proliferation to antigenic stimuli and mediates cytokine regulation further by converting the lymphocytic response from Th-1 to Th-2 type.[1]
Sedative properties It activates the forebrain sleep center unlike other hypnotics and therefore does not cause respiratory depression, incoordination, or hangovers. [1],[2],[3]
Miscellaneous It downregulates expression of cellular adhesion molecules [1],[4] and class-II major histocompatibility index antigens and antagonizes prostaglandins E2 and F2, histamine, serotonin, and acetylcholine. It decreases cellular proliferation, subperineural edema, and myelin phagocytosis,[2] and inhibits formation of new blood vessels by inhibiting basic fibroblast growth factor-induced angiogenesis.[2]
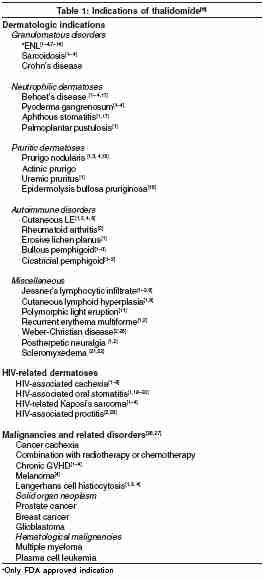
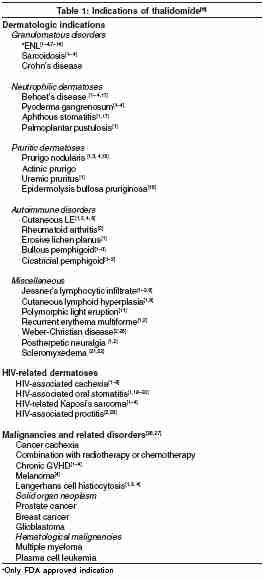
INDICATIONS
The indications[6] are listed in [Table - 1].
USES IN DERMATOLOGY
Dermatological conditions have been grouped into the following categories:[4]
(a) Very effective: ENL, aphthous stomatitis, Behcet′s disease, LE, and prurigo nodularis
(b) Moderately effective: Actinic prurigo, Langerhans cell histiocytosis, cutaneous sarcoidosis, erythema multiforme, graft- vs -host disease (GVHD), Jessner′s infiltrate, and uremic pruritus
(c) Possibly effective: Kaposi′s sarcoma, lichen planus, melanoma, and pyoderma gangrenosum
(d) Contraindicated: Toxic epidermal necrolysis (paradoxical increase in TNF-a activity)
Sheskin, in 1965, discovered the efficacy of thalidomide in ENLs and reviewed 4522 patients worldwide, of which 99% improved.[1] Resolution of lesions was seen within 24-48 hours after beginning the therapy,[1] as corroborated by Waters,[7] Convit et al.[8],[9] and Moreira et al .[10] Ramu and Girdhar stated that a combination of steroids, thalidomide and clofazimine, gave quicker results than thalidomide with steroids alone.[11],[12] Parikh et al. observed that if patients were on higher doses of steroids or if steroids were given for a longer time prior to thalidomide therapy, they took longer to improve with thalidomide.[12]
Most authors, viz, Sheskin and Convit[8] and Pearson and Vedagiri,[13] started thalidomide[14] in the dose of 400 mg/day for patients above 35-50 kg body weight. For those below this mark, thalidomide was administered in the dose of 6 mg/kg/day. Nowadays, it is recommended to start with 300 mg/day, to be tapered by 100 mg every 2-4 weeks with a maintenance dose of 50-100 mg for 6 months. Most authors reported a resolution of all the other symptoms of type-II reaction, including neuritis. It should be noted here that thalidomide does not affect the course of leprosy, nor does it have any effect on type-I lepra reaction. Pearson and Vedagiri[13] reported on three therapeutic failures in a series of patients who were later proven as type-I reaction on biopsy.
In our experience of thalidomide in 12 patients with refractory ENLs, 7 showed an excellent response, whereas 2 were therapeutic failures. We observed that relapses and failures were more if thalidomide was started late or in lower doses and in patients directly presenting with ENLs.
Thalidomide has been reported to be useful in few cases of prurigo nodularis,[1],[3],[4],[15] actinic prurigo,[1],[2],[4] uremic pruritus[1] and epidermolysis bullosa pruriginosa.[16] Although the exact mechanism of action in these diverse conditions is not known, it is purported that the sedative property causes decreased perception of peripheral stimuli, like pruritus, and interrupts the itch-scratch cycle.[15] Moreover, there may be a direct peripheral action on the proliferated neural tissue in prurigo lesions.[15]
Recalcitrant and necrotic aphthae show an excellent response to thalidomide in the dose of 100 mg/d for 5-28 days with fewer relapses. Patients with recurrent mucocutaneous aphthae have been shown to have a significantly increased chemotactic response. Thalidomide probably acts by blocking the chemotaxis.[1],[17]
Thalidomide is also remarkably effective in aphthosis associated with HIV,[18],[19] as found by Jacobson et al.[1] and Youle et al.[20] with no changes in the CD4 counts[18] or viral loads.[1] It has also been used with success in various other HIV-associated conditions[1],[2],[3],[4] such as Kaposi′s sarcoma, in which, probably, its antiangiogenic properties play a role. However, some authors sound a note of caution while using an immunomodulatory drug in an already immunocompromised population.
A randomized double-blind trial in 96 males with mucocutaneous Behcet′s disease showed complete response in 21% of patients with a 100-300 mg/day dose.[1] Another study reported on a complete resolution of mucocutaneous and arthritic components.[1] A 31-year-old male with Behcet′s disease associated with palmoplantar pustulosis showed complete resolution with a dose of 200mg/day for 2 weeks.[1] However, most authors reported no improvement in the ocular lesions.[1]
Various authors have reported astounding success in chronic GVHD cases recalcitrant to steroids, cyclosporine, and other immunosuppressive agents.[1] Thalidomide is usually administered in doses of 400-1600 mg/day. Most series report an excellent response in more than 75% patients. Standard-chronic-risk GVHD patients responded better than the high-risk category.
Thalidomide improves the cutaneous and articular features of lupus erythematosus[1],[2],[4],[6] without affecting the visceral components. Single case reports of Thalidomide′s success in palmoplantar pustulosis,[1] Jessner′s lymphocytic infiltrate,[1],[2],[3],[6] sarcoidosis,[1],[2],[3],[4] scleremyxedema,[21],[22] erosive lichen planus,[1] erythema multiforme,[1],[2] pemphigoid, [1],[2],[3] and a few other conditions have been reported.
It must be stated that all the aforementioned conditions were resistant to the routine line of therapy. Few conditions which did not respond to thalidomide include lichen planopilaris,[23] toxic epidermal necrolysis,[1] mycosis fungoides,[24] erythema nodosum,[3] psoriasis,[1] and balanitis circinata.[1]
THALIDOMIDE IN CHILDREN
Thalidomide has been used with success in children in conditions such as GVHD,[1] pyoderma gangrenosum,[2] Crohn′s disease,[1] and aphthosis[1] in doses ranging from 3 to 9.5 mg/kg/day. One series of 14 children with GVHD reported therapeutic failure associated with a high mortality rate.[1] In our experience, a 6-year-old girl with ENL, too, failed to respond and eventually succumbed.
ADVERSE EFFECTS
Teratogenicity Thalidomide is classified as a pregnancy category-X drug.[3] Severe deformities may result even if a single dose is taken at 20-40 days of gestation.[2],[3] They include amelia; phocomelia; absence or hypoplasia of bones; anotia; micropinna; absent auditory canal; anopthalmos; micropthalmos; congenital heart disease; anomalies of the genitalia, gastrointestinal, or urinary tracts; and facial palsy.[1],[3] It is also associated with a high mortality rate at birth.[1] The exact mechanism of teratogenicity is unknown but may be related to its antiangiogenic properties,[1],[2] cell injury, negative action on chondrogenesis, growth factors, integrins, or mesonephric signals for limb growth.[4]
Peripheral neuropathy Thalidomide may cause irreversible peripheral neuropathy presenting as symmetric painful paresthesias of extremities with sensory loss in the lower extremities with or without muscle cramps or weakness.[1],[2] Electophysiologic findings show an axonal neuropathy with reduced sensory nerve action potentials, and loss of large-diameter nerve fibers without segmental demyelination is seen on biopsy.[1] This is unrelated to the dose of thalidomide.[1]
Somnolence This was the purpose for which thalidomide was first marketed. It can be circumvented by administration at night. It may decrease over time or may need a dose reduction or discontinuation.[1]
Dermatological side effects These include exfoliative dermatitis,[2] dry mouth and skin,[1],[2] pruritus,[1] urticaria,[11] morbilliform eruption,[3] brittle nails,[2] red palms,[2] allergic vasculitis,[4] and thrombocytopenic purpura.[4]
Miscellaneous Constipation,[1],[3] pedal edema,[12] dizziness,[1] headache,[1] mood swings,[1] bradycardia or tachycardia,[1],[3] hypotension,[3] hypertension,[3] neutropenia,[3] hypothyroidism,[1] convulsions,[11] increased appetite and weight gain,[2] menstrual abnormalities,[2] and thromboembolic complications such as deep vein thrombosis and pulmonary embolism[4] have been reported by some.
DRUG INTERACTIONS
Thalidomide should be used cautiously with alcohol and other sedatives, viz, barbiturates, chlorpromazine, reserpine, etc, as it increases their activity.[1],[6] Combining thalidomide with drugs that induce cytochrome P-450 enzyme, such as HIV protease inhibitors, rifampicin, griseofulvin phenytoin, and carbamazepine, may interfere with efficacy of hormonal contraceptives, leading to risk of teratogenicity.[1],[6]
GUIDELINES
In other countries, thalidomide is available to only those physicians and pharmacists who are registered with the system for thalidomide education and prescribing safety (STEPS) program.[1] In Mumbai, Bombay Leprosy Project provides free thalidomide to patients. Alternatively, one may have access to thalidomide through CLRTI, Chennai.
However, one has to exercise extreme caution[25] while prescribing thalidomide in view of the disaster in the past. In India, with increased access, vigilant monitoring is necessary.
A written, informed consent is imperative. The patient must be explained about the adverse effects, must not share the drug with anyone else, and female patients must follow two methods of contraception (one highly effective method and another barrier method) and must not donate blood.[25] As effects of thalidomide on spermatogenesis is not known, male patients too must be advised to use barrier contraceptives.[1]
The absolute contraindications[1],[6] for thalidomide include sensitivity to the drug, pregnancy and existing severe peripheral neuropathy. In those with hepatic dysfunction, renal dysfunction, neurological disorders, gastrointestinal dysfunction, hypertension, and hypothyroidism, it may be used with caution.
Monitoring guidelines include a baseline pregnancy test, complete blood count with an absolute neutrophil count, HIV RNA, a clinical neurological examination, and an electromyography (EMG) or nerve conduction velocity (NCV) study.[1] Later, pregnancy testing is done weekly for a month and monthly thereafter, and clinical neurological testing monthly for 3 months and then every 6 months. EMG/NCV may be repeated biannually or with every 10 g increase in the cumulative dose.[25] In HIV patients, HIV RNA must be repeated at 1 month, 3 months, and every 3 months thereafter.[1]
One must withhold or discontinue therapy if a patient fails to comprehend or comply with the instructions, pregnancy test is positive, paresthesiae develop, there is decrease in sensory nerve action potential by more than 40%, or absolute neutrophil count falls below 750/mm[3].[1]
ONCOLOGY
Thalidomide has been found to be effective in many cases of refractory multiple myeloma and also breast cancer,[26] prostrate cancer, and leukemia. It can be combined with radiation and chemotherapy.
ANALOGS
Second-generation analogs[27] of thalidomide include lenalidomide (phase-II and -III clinical trials), revimid, and actimid, and are very potent in the treatment of multiple myeloma and other oncologic conditions.
CONCLUSION
Thalidomide is a double-edged weapon. The 1961 tragedy remains as a bitter lesson in our minds and serves as a reminder to exercise extreme caution and vigilance when using any new drug. However, if used judiciously, it can work miracles in many recalcitrant conditions.
| 1. |
Radomsky CL, Levine N. Thalidomide. Dermatol Clin 2001;19:87-103.
[Google Scholar]
|
| 2. |
Tseng S, Pak G, Washenik K, Pomeranz MK, and Shupack JL. Rediscovering thalidomide: a review of it's mechanism of action, side effects, and potential uses. J Am Acad Dermatol 1996;35:969-79.
[Google Scholar]
|
| 3. |
Perri AJ III, Hsu S. A review of thalidomide's history and current dermatological applications. Dermatology Online Journal; 9(3):5. Available at http://dermatology.cdlib.org/93/reviews/thalidomide/hsu.html
[Google Scholar]
|
| 4. |
Wu, JJ, Huang DB, Pang KR, Hsu S, Tyring SK. Thalidomide: dermatological indications, mechanism of action and side effects. Br J Dermatol 2005;153:254-73.
[Google Scholar]
|
| 5. |
Moncada B, Baranda ML, Gonzalez-Amaro R, Urbina R, Loredo CE. Thalidomide-effect on T-cell subsets a possible mechanism of action. Int J Lep 1985;53:201-5.
[Google Scholar]
|
| 6. |
Knable AL Jr. Miscellaneous systemic drugs. In : Wolverton SE, editor. Comprehensive Dermatologic Drug Therapy. 1st ed. Philadelphia: WB Saunders; 2001. p. 445-54.
[Google Scholar]
|
| 7. |
Waters MF. An internally-controlled double blind trial of thalidomide in severe erythema nodosum leprosum. Lepr Rev 1971;42:26-42.
[Google Scholar]
|
| 8. |
Sheskin J, Convit J. Results of a double blind study of the influence of thalidomide on the lepra reaction. Int J Lepr 1969;37:135-46.
[Google Scholar]
|
| 9. |
Convit J, Soto JM, Sheskin J. Thalidomide therapy in the lepra reaction. Int J Lepr1967;35:446-51.
[Google Scholar]
|
| 10. |
Moreira AL, Gilla K. Comparison of pentoxyphylline, thalidomide and prednisone in the treatment of ENL. Int J Lep 1998;66:61-5.
[Google Scholar]
|
| 11. |
Parikh DA, Maniar JK, Ganapathi R. Thalidomide in leprosy and some dermatological conditions-a review. Indian J Lep 1985;57:862-7.
[Google Scholar]
|
| 12. |
Parikh DA, Ganapathi R, Revankar CR. Thalidomide in leprosy-study of 94 cases. Indian J Lep 1986;58:560-6.
[Google Scholar]
|
| 13. |
Pearson JM, Vedagiri M. Treatment of moderately severe erythema nodosum leprosum with thalidomide- a double blind controlled trial. Lep Rev 1969;40:111-6.
[Google Scholar]
|
| 14. |
Sheskin J, Magora A, Sagher F. Motor conduction velocity studies in patients with leprosy reaction treated with thalidomide and other drugs. Int J Lep 1969;37:359-63.
[Google Scholar]
|
| 15. |
van den Broek H. Treatment of prurigo nodularis with thalidomide. Arch Dermatol 1980;116:571-2.
[Google Scholar]
|
| 16. |
Bulic OS, Fassihs H, Mellerio JE, McGrath JA, Atherton DJ. Thalidomide in the management of epidermolysis bullosa pruriginosa. Br J Dermatol 2005;152:1332-4.
[Google Scholar]
|
| 17. |
Letsinger JA, McCarty MA, Jorizzo JL. Complex aphthosis: a large case series with evaluation algorithm and therapeutic ladder from topicals to thalidomide. J Am Acad Dermatol 2005;52:500-8.
[Google Scholar]
|
| 18. |
Ghigliotti G, Repetto T, Farris A, Roy MT, De Marchi R. Thalidomide: treatment of choice for aphthous ulcers in patients seropositive for human immunodeficiency virus. J Am Acad Dermatol 1993;28:271-3.
[Google Scholar]
|
| 19. |
Radeff B, Kuffer R, Samson J. Recurrent aphthous ulcer in patient infected with human immunodeficiency virus: successful treatment with thalidomide. J Am Acad Dermatol 1990;23:523-5.
[Google Scholar]
|
| 20. |
Youle M, Clarbour J, Farthing C, Connolly M, Hawkins D, Staughton R, et al . Treatment of resistant aphthous ulceration with thalidomide in patients positive for HIV antibody. Br Med J 1989;298:432.
[Google Scholar]
|
| 21. |
Caradona S, Jacob H. Thalidomide as a potential treatment for scleromyxoedema. Arch Dermatol 2004;140:277-80.
[Google Scholar]
|
| 22. |
Sansbury JC, Cocuroccia B, Jorizzo J, Gubinelli E, Gisondi P, Girolomoni G. Treatment of recalcitrant scleromyxoedema with thalidomide in 3 patients. J Am Acad Dermatol 2004;51:126-31.
[Google Scholar]
|
| 23. |
Jouanique C, Reygagne P, Bachelez H, Dubertret L. Thalidomide is ineffective in the treatment of lichen planopilaris. J Am Acad Dermatol 2004;51:480-1.
[Google Scholar]
|
| 24. |
Brightman L, Demiere MF. Thalidomide in mycosis fungoides. J Am Acad Dermatol 2005;52:1100-1.
[Google Scholar]
|
| 25. |
Powell RJ, Gardner-Medwin JM. Guideline for the clinical use and dispensing of thalidomide. Postgrad Med J 1994;70:901-4.
[Google Scholar]
|
| 26. |
Quilitz R, Pharm D. Thalidomide in oncology: the peril and the promise. J Moffit Cancer Centre 1999;6(5). Available at http:// www.moffit.usf.edu/pubs/ccj/index.html
[Google Scholar]
|
| 27. |
Teo SK. Properties of thalidomide and its analogues: implications for anticancer therapy. AAPS J 2005;7:E14-E19. Available at http://www.aapsj.org
[Google Scholar]
|
Fulltext Views
6,960
PDF downloads
1,967





