Translate this page into:
Linear plaque over the face
Correspondence Address:
S Veeranna
Department of Dermatology, JSS Hospital, Mysore, Karnataka 570004
India
| How to cite this article: Veeranna S. Linear plaque over the face. Indian J Dermatol Venereol Leprol 2006;72:83-84 |
 |
 |
 |
 |
 |
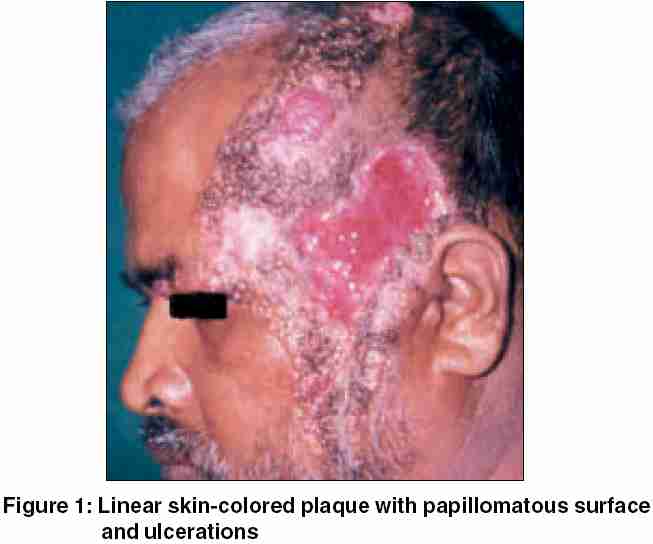 |
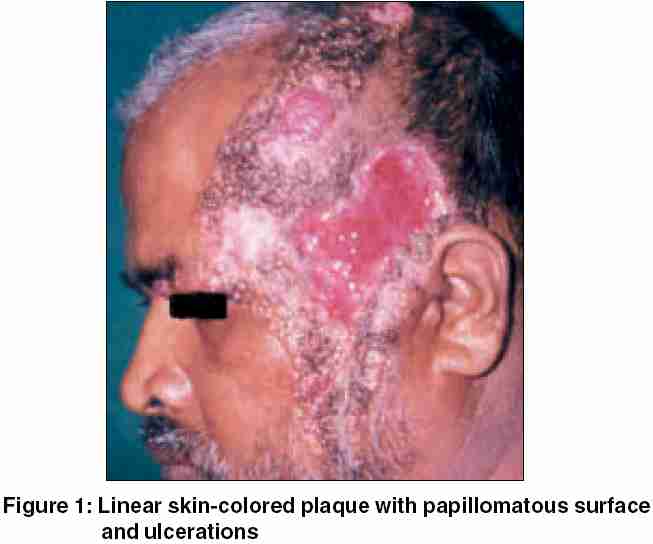
A 50-year-old man presented with skin lesions over left side of the face and scalp. The lesions appeared during childhood over the left temporal area, followed by a spurt of growth at puberty and thereafter slowly progressed to involve the left side of face and forehead. It was asymptomatic without any pain, itching, or bleeding. Six months prior to presentation, he had sustained an injury over the lesions, which led to persistent ulcers. There was no history of diabetes or hypertension.
Examination revealed linear plaque with papillomatous surface over left side of scalp, extending to forehead and down the cheeks [Figure - 1]. Three large ulcers covered with granulation tissue were present over the temporal area. The biopsy was taken from the edge of the ulcer, including papular growth. Histopathological features are shown in [Figure - 2][Figure - 3].
WHAT IS YOUR DIAGNOSIS?
Diagnosis: Syringocystadenoma papilliferum associated with nevus sebaceous
Histopathology showed acanthotic epidermis with papillomatosis and areas of ulceration. There were cystic invagination s extending downward from the epidermis. At the lower end of these invaginations, papillary projections lined by two layers of cells, outer cuboidal and inner columnar, were observed [Figure - 2]. Many plasma cells [Figure - 3] and large sebaceous glands were present in the dermis.
DISCUSSION
Syringocystadenoma papilliferum is a benign lesion usually occurring on the scalp, but may involve face and other parts of the body. In one-third of the cases it may be associated with nevus sebaceous.[1]
The lesions are present at birth or appear in early childhood. These occur either as nodular plaque, linear group of papulonodules, or as a solitary nodule. The plaque form is most commonly seen as a hairless area on the scalp, whereas linear form is more often seen on the neck or face. These lesions generally become more prominent, verrucous, or crusted during puberty.[2]
Histogenesis of this lesion is controversial. Both apocrine and eccrine differentiations were hypothesized.[1] It is possible that the lesions originate from undifferentiated pluripotent cells. This probably explains its localization to areas normally devoid of apocrine glands in 90% of the cases.[3]
Histopathology shows acanthotic epidermis with varying degree of papillomatosis. Several cystic invaginations extend downward from the epidermis. At the lower end of the invaginations, numerous papillary projections, lined by outer cuboidal and inner columnar cells, extend into the lumen. Below the cystic invaginations, in the deep dermis, groups of tubular glands with large lumina are seen. Dense infiltrate of plasma cells in the stroma is a highly characteristic feature.[4]
Our patient had clinical and histological features of both nevus sebaceous and syringocystadenoma papilliferum. This condition has to be differentiated clinically from epidermal nevus, sebaceous nevus, basal cell carcinoma, and eccrine spiradenoma. Histopathologically, it resembles tubular apocrine adenoma, papillary eccrine adenoma, and apocrine hidrocystoma. Surgical excision is the main treatment option. Occasionally, basal- or squamous-cell carcinoma develops on a pre-existing syringocystadenoma papilleferum.[2]
| 1. |
Koh HK, Bhawan J. Tumors of the skin. In : Moschella SC, Hurley HJ, editors. Dermatology. 3rd ed. Philadelphia: WB Saunders; 1992. p. 1744-5.
[Google Scholar]
|
| 2. |
Atherton DJ, Moss C. Naevi and other developmental defects. In : Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7th ed. Oxford: Blackwell Science; 2004. p. 15.1-15.114.
[Google Scholar]
|
| 3. |
Amladi ST, Jerajani HR. Nevi and other developmental defects. In : Valia RG, editor. IADVL Text Book and Atlas of Dermatology. 2nd ed. Mumbai: Bhalani; 2001. p. 142-89.
[Google Scholar]
|
| 4. |
Elder D, Elenitsas R, Ragsdale BD. Tumors of epidermal appendages. In : Elder D, Elenitsas R, Jaworksy C, Johnson B, Jr, editors. Lever's Histopathology of the Skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p. 747-804.
[Google Scholar]
|
Fulltext Views
2,237
PDF downloads
2,286





