Translate this page into:
Systemic contact dermatitis
2 Consultant Dermatologist, Lucknow, Uttar Pradesh, India
Correspondence Address:
A K Bajaj
3/6, Panna Lal Road, Allahabad, Uttar Pradesh
India
| How to cite this article: Bajaj A K, Saraswat A. Systemic contact dermatitis. Indian J Dermatol Venereol Leprol 2006;72:99-102 |
Systemic contact dermatitis (SCD), better termed systemically reactivated allergic contact dermatitis, is a type of contact hypersensitivity reaction in which ingestion or other systemic exposure to a contact allergen occurs in an already sensitized person. Although the initial sensitizing exposure is usually by topical application, re-exposure by the oral, intravenous or inhalation routes can cause SCD. Even percutaneous exposure through inflamed or broken skin may result in enough systemic absorption to cause SCD. These reactions may occur not only after ingestion of the primary allergen, but also after ingestion of other immunochemically related allergens.[1] Probably all allergens have the capacity to elicit SCD in the presence of sufficiently strong pre-existing sensitivity and a large enough administered dose. However, clinically significant SCD occurs only to certain allergens to which we are frequently exposed through a variety of routes.
Clinical features of systemic contact dermatitis
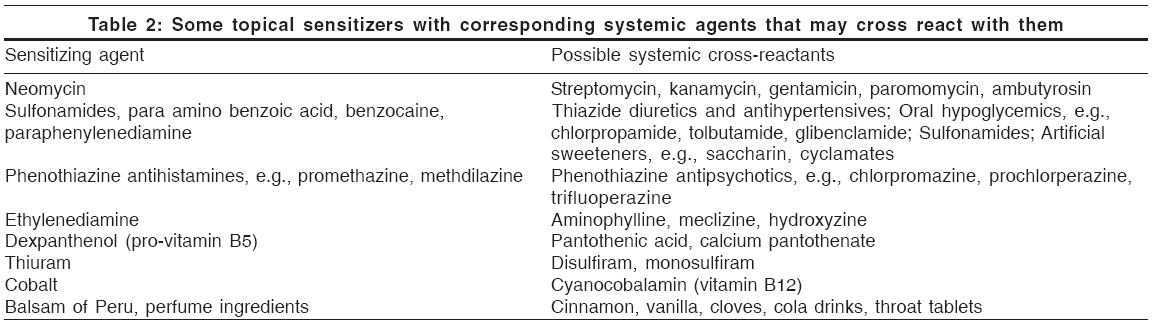
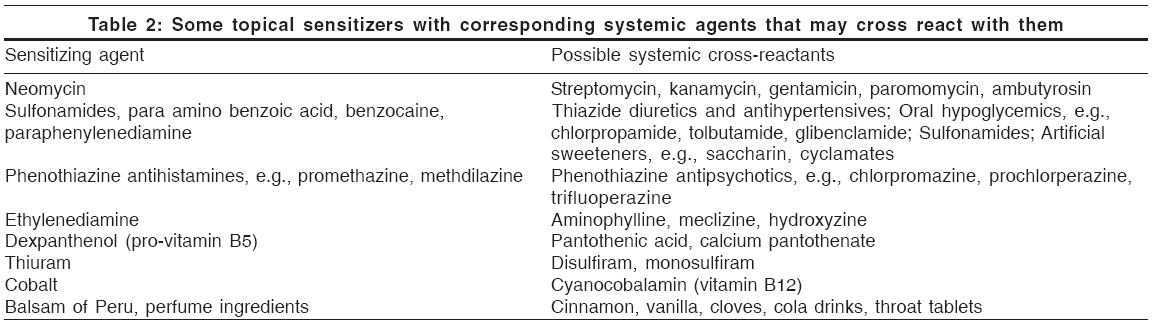
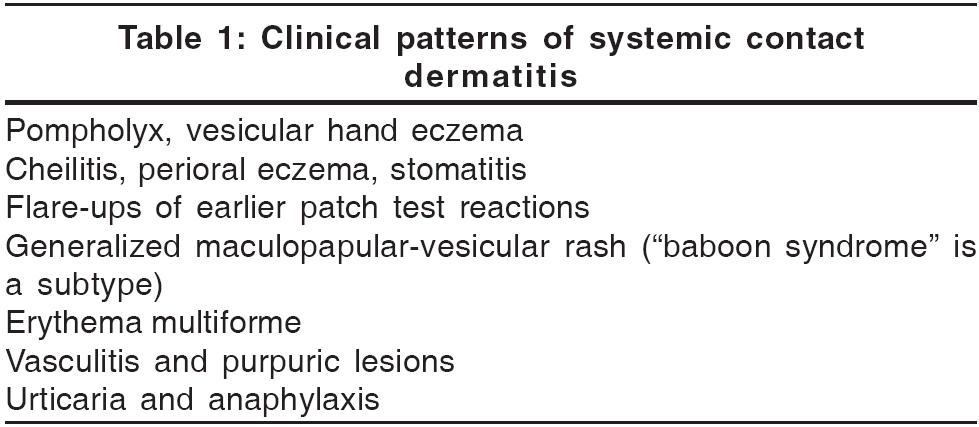
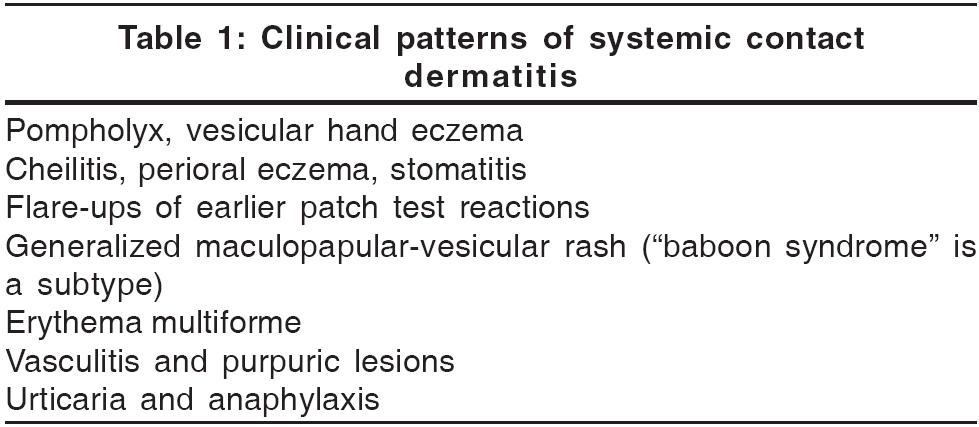
A variety of reaction patterns are seen in patients with SCD and a high index of suspicion is required to diagnose them. These patterns are presented in [Table - 1]. In addition to cutaneous lesions, general systemic effects may also accompany SCD. Headaches, fever and malaise may occur in sensitized patients on oral rechallenge with nickel and medicaments. In neomycin and chromate sensitive patients, oral provocation may produce nausea, vomiting and diarrhea.[2]
The most frequent types of reactions are focal flares of previous patch test sites. However, since Indian patients are patch-tested infrequently, flares at sites of previous dermatitis, e.g., atopic eczema, diaper dermatitis or drug rashes, may be more common manifestations of SCD.[3] Widespread eczema and erythema, sometimes associated with urticarial lesions, can also be seen in severe cases.[4]
Recurring itchy eruptions of deep-seated vesicles on the fingers and palms without clear external reasons may be due to nickel, cobalt or chromate ingestion.[5],[6] Atopic individuals are more prone to develop such reactions and diets low in metal-containing foods may help to control flares in them. Patch tests are not always positive in these cases and oral provocation tests may be needed to uncover the cause.[7] Balsam of Peru,[8] garlic, food colors, preservatives and antioxidants[9],[10] are also known to cause flares of vesicular hand eczema.
In severe cases, acrally located purpuric lesions, indicative of vasculitis or erythema multiforme-like lesions, may be seen.[11] A large variety of medicaments, laboratory chemicals and even common items like soap, hair dye, metals and spray cologne have been reported to cause these severe types of SCD.[12] Photosensitivity may accompany rare cases of SCD, as was seen in a patient who had occupational and systemic contact dermatitis due to vitamin B6.[13]
Another potentially serious type of SCD is urticaria and anaphylaxis, which can rarely be seen in conjunction with typical eczematous lesions.[4] Azo dyes, sulfonamides and antihistamines have been reported to cause urticarial SCD.
A clinically distinct type of SCD is termed ′baboon syndrome.′ This refers to the erythema of buttocks and upper inner thighs, reminiscent of the red rump of a baboon. In addition to these sites, the eyelids and other body folds may also be involved and severe cases may show pustules on a background of bright erythema. Initial reports implicated inhalation of mercury (from broken thermometers) and ingestion of nickel in previously sensitized patients as the cause of this distinct reaction.[14],[15] Since then, more than 100 cases have been reported, with systemic drugs being increasingly implicated as causative agents. However, it has recently been recognized that the term ′baboon syndrome′ has been used to describe two distinctly different subgroups of patients. A large majority of reported cases represented a peculiar intertriginous drug rash with some overlapping features of fixed drug eruption and acute generalized exanthematous pustulosis.[16] All these patients had negative patch tests with the implicated drugs and other cross-reacting agents, i.e., had no demonstrable previous cutaneous sensitization. The second, much smaller, group was that of patients with a true SCD who showed positive patch tests to the causative drugs or to immunochemically related allergens.[17],[18]
Since these two pathophysiologically distinct drug eruptions have identical clinical features, a new term - ′symmetrical drug related intertriginous and flexural exanthema (SDRIFE)′ - has recently been proposed for cases of drug-related baboon syndrome and diagnostic criteria have been suggested.[19]
Mechanism of systemic contact dermatitis
Sensitized individuals may develop skin eruptions within hours of systemic allergen exposure. This suggests that mechanisms other than type IV delayed-type hypersensitivity are involved. There is evidence that systemic reactions to ingested haptens can be mediated by a type III immunologic reaction.[20] Urticaria and anaphylaxis-type reactions, e.g., those occurring in latex-sensitive patients upon eating bananas, tomatoes, etc., involve IgE-mediated type I reactions.[21]
Agents commonly causing systemic contact dermatitis
Several drugs are known to cause SCD. Amongst them, antibiotics like penicillin, streptomycin and neomycin are the most common. Although the topical use of the former two is now rare, topical neomycin is still widely used. Halogenated hydroxyquinolines like vioform and quiniodochlor are commonly used both topically and systemically. Corticosteroid allergy is now well known and severe systemic reactions to oral, nasal or parenteral administration of corticosteroids have been reported in some patients.[22] Several systemic drugs may cross-react with topical allergens; an indicative list is presented in [Table - 2].
Nickel, chromium and cobalt are well known to cause recurrent pompholyx-type reactions. These metals are commonly found in minute amounts in oatmeal, wheat flour, rice, beans, nuts, sunflower seeds, dark chocolate, tea-leaves, canned fruits, pineapple, pears, plums, potatoes and green leafy vegetables. There are several reports of mercury causing the baboon syndrome type of SCD after exposure by inhalation (broken thermometers), ingestion (thiomerosal, dental amalgam fillings) or percutaneous absorption (mercurochrome).[23]
Systemic contact dermatitis induced by spices is well known, though rare. Nutmeg, mace, cardamom, cinnamon and curry are all known to cause these reactions.[24] Spices may cross-react with some known contact allergens [Table - 2].
Patch testing in systemic contact dermatitis
Patch testing with chemicals known to cause SCD can be valuable not only in determining the cause of an allergic contact dermatitis, but also in serving as a warning against their systemic administration. Knowledge of drugs that are immunochemically related to these allergens can help in predicting possible cases of SCD. For example, in subjects with contact allergy to ethylenediamine, intravenous administration of aminophylline (which contains ethylenediamine) or ingestion of structurally related antihistamines (meclizine, hydroxyzine) may produce widespread eczematous eruptions.
Patch testing may also help when several drugs have been given concurrently and an eczematous flare has occurred. In such cases, the drug showing a positive patch test reaction would be the likely cause. Patch testing would also be a much safer option than scratch or intracutaneous tests in these situations. The role of patch testing in non-eczematous drug eruptions is controversial and the significance of such testing is not known.
In conclusion, systemic contact dermatitis is an important entity to remember when faced with such diverse conditions as widespread ′nonspecific′ or ′allergic′ rashes, extensive eczematous eruptions, vesicular hand eczema, ′idiopathic′ urticaria, vasculitis or even erythroderma. The cornerstones of its diagnosis remain the same as in other cases of contact dermatitis: meticulous history taking, thorough examination and judicious patch testing. Oral provocation may be done in some cases, but only in an inpatient environment and with the understanding that severe reactions may result from this procedure.
One of the authors (AKB) has come across cases of SCD due to neomycin and enterovioform, which presented as widespread eczematous eruptions. In a country like India, where a large number of chemicals, especially antibiotics, are used both topically and systemically, the incidence of SCD should not be as uncommon as perceived from the paucity of published reports from the country.
| 1. |
Fisher AA. Systemic eczematous "contact type" dermatitis medicamentosa. Ann Allergy 1966;24:406-20.
[Google Scholar]
|
| 2. |
Menne T, Hjorth N. Reactions to systemic exposure to contact allergens. Semin Dermatol 1982;1:15-24.
[Google Scholar]
|
| 3. |
Shelley WB, Bennetts RG. Primary contact sensitization site: A determinant for the localization of a diphenhydramine eruption. Acta Derm Venereol (Stockh) 1972;52:376-8.
[Google Scholar]
|
| 4. |
Mancuso G, Masara N. Contact urticaria and severe anaphylaxis from rifamycin SV. Contact Dermatitis 1992;27:124-5.
[Google Scholar]
|
| 5. |
Christensen OB, Moller H. External and internal exposure to the antigen in the hand eczema of nickel allergy. Contact Dermatitis 1975;1:136-41.
[Google Scholar]
|
| 6. |
Kaaber K, Veien NK. The significance of chromate ingestion in patients allergic to chromate. Acta Derm Venereol (Stockh) 1977;57:321-3.
[Google Scholar]
|
| 7. |
Veien NK, Kaaber K. Nickel, cobalt and chromium sensitivity in patients with pompholyx (dyshidrotic eczema). Contact Dermatitis 1979;5:371-4.
[Google Scholar]
|
| 8. |
Veien NK, Hattel T, Justesen O, Norholm N. Oral challenge with balsam of Peru. Contact Dermatitis 1985;12:104-7.
[Google Scholar]
|
| 9. |
Burden AD, Wilkinson SM, Beck MH, Chalmers RJ. Garlic-induced systemic contact dermatitis. Contact Dermatitis 1994;30:299-300.
[Google Scholar]
|
| 10. |
Baer RL, Leider M. The effects of feeding certified food azo-dyes in paraphenylenediamine-hypersensitive subjects. J Invest Dermatol 1949;13:223-32.
[Google Scholar]
|
| 11. |
Meneghini CL, Angelini G. Secondary polymorphic eruptions in allergic contact dermatitis. Dermatologica 1981;163:63-5.
[Google Scholar]
|
| 12. |
Rietschel RL, Fowler Jr. JF. Systemic contact-type dermatitis. In: Rietschel RL, Fowler Jr. JF, editors. Fisher's Contact Dermatitis. 5th ed. Philadelphia: Lippincott Williams & Wilkins;2001. p. 89-101.
[Google Scholar]
|
| 13. |
Bajaj AK, Rastogi S, Misra A, Misra K, Bajaj S. Occupational and systemic contact dermatitis with photosensitivity due to vitamin B6. Contact Dermatitis 2001;44:184-5.
[Google Scholar]
|
| 14. |
Andersen KE, Hjorth N, Menne T. The baboon syndrome: Systemically induced allergic contact dermatitis. Contact Dermatitis 1984;10:97-100.
[Google Scholar]
|
| 15. |
Nakayama H, Niki F, Shono M, Hada S. Mercury exanthema. Contact Dermatitis 1983;9:411-7.
[Google Scholar]
|
| 16. |
Wolf R, Orion E, Matz H. The baboon syndrome or intertriginous drug eruption: A report of 11 cases and a second look at its pathomechanism. Dermatol Online J 2003;9:2.
[Google Scholar]
|
| 17. |
Isakssom M, Ljunggren B. Systemic contact dermatitis from ethylene diamine in an aminophylline preparation presenting as the baboon syndrome. Acta Derm Venereol 2003;83:69-70.
[Google Scholar]
|
| 18. |
Gallo R, Parodi A. Baboon syndrome from 5-amino salicylic acid. Contact Dermatitis 2002;46:110.
[Google Scholar]
|
| 19. |
Hausermann P, Harr T, Bircher AJ. Baboon syndrome resulting from systemic drugs: is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis 2004;51:297-310.
[Google Scholar]
|
| 20. |
Veien NK, Svejgaard E, Menne T. In vitro lymphocyte transformation to nickel: a study of nickel sensitive patients before and after epicutaneous and oral challenge with nickel. Acta Derm Venereol (Stockh) 1979;59:447-52.
[Google Scholar]
|
| 21. |
Rodriguez M, Vega F, Garcia MT, Panizo C, Laffond E, Montalvo A, et al . Hypersensitivity to latex, chestnut and banana. Ann Allergy 1993;70:31-4.
[Google Scholar]
|
| 22. |
Wilkinson SM, Smith AG, English JS. Erythroderma following the intradermal injection of the corticosteroid budesonide. Contact Dermatitis 1992;27:121-2.
[Google Scholar]
|
| 23. |
Lerch M, Bircher AJ. Systemically induced allergic exanthem from mercury. Contact Dermatitis 2004;50:349-53.
[Google Scholar]
|
| 24. |
Leifer W. Contact dermatitis due to cinnamon: Recurrence of dermatitis following oral administration of cinnamon oil. AMA Archives Dermatol Syphilol 1951;64:52-6.
[Google Scholar]
|
Fulltext Views
11,250
PDF downloads
3,846





