Translate this page into:
Primary cutaneous multifocal CD 30+ anaplastic large cell lymphoma
Correspondence Address:
M P Binitha
"Haritha", PO Beypore North, Calicut - 673 015, Kerala
India
| How to cite this article: Asha L K, Thomas D, Binitha M P, Nandakumar G. Primary cutaneous multifocal CD 30+ anaplastic large cell lymphoma. Indian J Dermatol Venereol Leprol 2006;72:376-378 |
Abstract
A 45-year-old male presented with asymptomatic tumors all over the body. The tumors showed no signs of ulceration or regression. There were generalized, nontender, firm to hard enlarged lymph nodes without hepatosplenomegaly. Biopsy and immunophenotyping revealed CD 30+ anaplastic primary cutaneous large cell lymphoma. Primary cutaneous anaplastic large cell lymphoma is characterized by single or grouped reddish-brown tumor nodules, which frequently tend to ulcerate. Secondary involvement of lymph nodes is seen in only 25%. The lesions responded dramatically to chemotherapy, but recurred.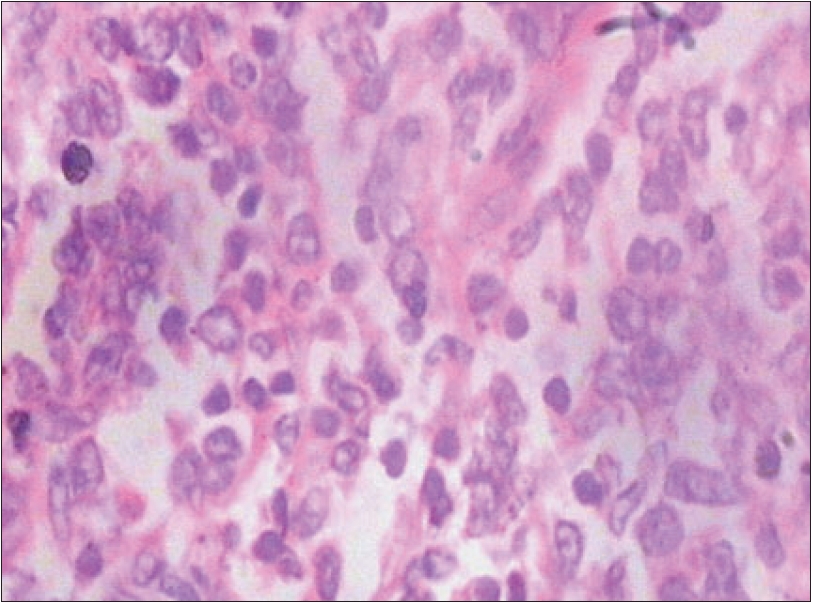 |
| Lymph node biopsy showing atypical lymphocytes some of which are in mitosis (H and E, 400x) |
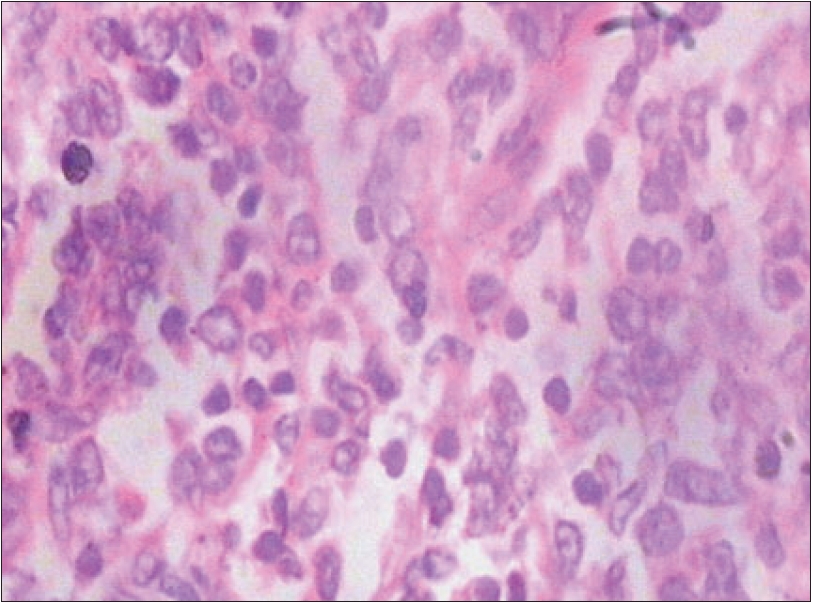 |
| Lymph node biopsy showing atypical lymphocytes some of which are in mitosis (H and E, 400x) |
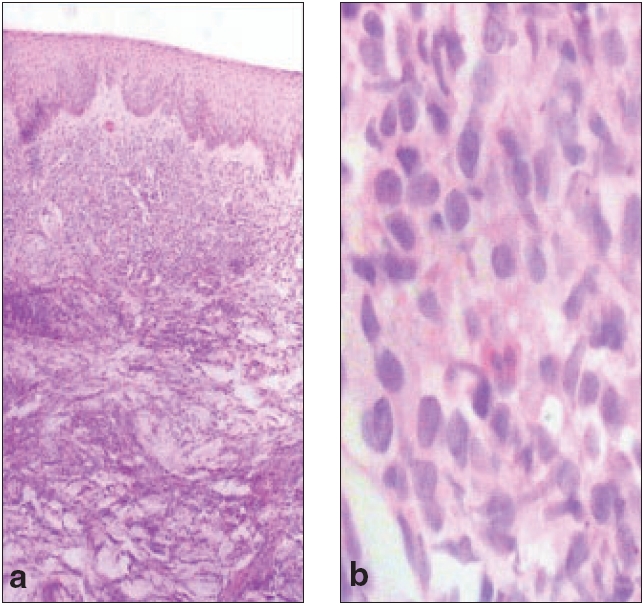 |
| (a) Diffuse dense monomorphic infiltrate of lymphocytes with interstitial extension (H and E, 100x) (b) High power view of abnormal lymphocytes (H and E, 400x) |
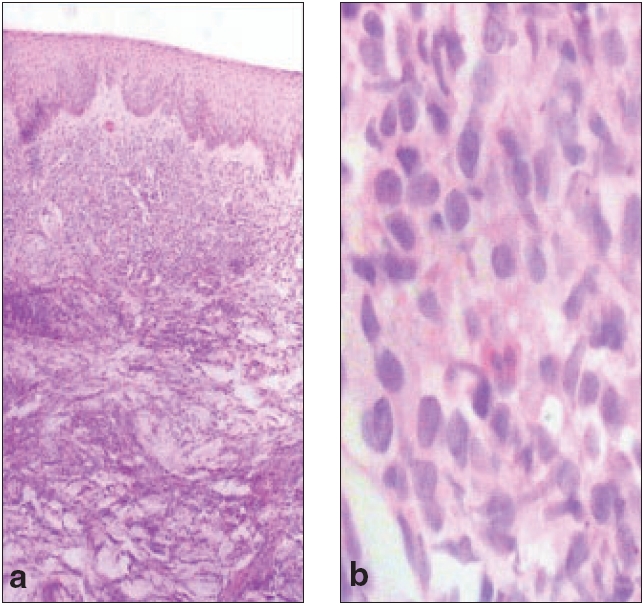 |
| (a) Diffuse dense monomorphic infiltrate of lymphocytes with interstitial extension (H and E, 100x) (b) High power view of abnormal lymphocytes (H and E, 400x) |
 |
| Tumors on upper arm and trunk |
 |
| Tumors on upper arm and trunk |
Introduction
Anaplastic large cell lymphoma (ALCL) is a neoplastic proliferation of lymphoid cells with highly pleomorphic cytological features, often present in a sinusoidal distribution and almost always expressing the lymphocyte activation marker CD 30.[1] It is rare, representing about 2 to 5% of Non Hodgkin′s lymphoma (NHL). There are two forms of ALCL, systemic and primary cutaneous. We report a case of primary cutaneous CD 30+ ALCL presenting with disseminated, large, skin tumors and generalized lymphadenopathy mimicking a primary systemic ALCL.
Case report
A 45-year-old male, a manual laborer, presented to us with asymptomatic raised lesions all over the body which were progressively increasing in size, number and thickness for the past three months. The lesions started on the right upper arm and gradually spread to other areas. The lesions did not show signs of regression or ulceration. There was no history of fever, weight loss or night sweats.
Examination revealed a moderately built and nourished, healthy man. He had bilateral cervical, axillary and inguinal, firm to hard lymph nodes 2 x 2 cm to 3 x 2 cm in size. They were discrete, nontender and mobile. There was no pallor or jaundice. The patient had multiple, reddish-brown, firm to woody hard, nontender plaques [Figure - 1] varying in size from 7 x 5 cm to 1 x 1 cm distributed bilaterally and asymmetrically over the extremities and trunk. The face and neck were relatively spared. Some of the plaques showed a central depression giving an annular configuration to the lesions. The larger lesions showed minimal scaling and a peau d′ orange appearance. The skin overlying the lesions could not be pinched. The peripheral nerves were not thickened. There was no hepatosplenomegaly and the other systems were within normal limits.
Investigations revealed a normal routine hemogram and urine examination. Peripheral smear was normal. Liver and renal function tests, serum calcium and blood sugar were within normal limits and serum ELISA for HIV was negative. Tissue smears showed large cells with bilobed nuclei. These were differentiated from Reed-Sternberg cells by the absence of prominent nucleoli. A skin biopsy showed diffuse dense infiltrate of large lymphoid cells with irregular folded nuclei and abundant cytoplasm. The cytoplasm of adjacent cells abutted closely giving a cohesive appearance [Figure - 2]. Eosinophils were also present. The collection of cells was clearly demarcated from the epidermis.
Lymph node biopsy showed completely effaced architecture and a diffuse population of immature large lymphoid cells with convoluted nuclei and six to eight mitoses per high power field [Figure - 3]. Immunophenotyping showed CD 3 and CD 30 positivity, while CD 15 and CD 20 were negative indicating a primary cutaneous origin. Bone marrow examination and X-ray chest did not reveal any obvious tumor infiltration. Ultrasound scan of liver, spleen, kidney and para-aortic areas was normal. The findings were confirmative of primary cutaneous multifocal CD 30+ anaplastic large cell lymphoma. The patient was referred to the Oncology department for further management.
Our patient was treated with the CHOP regime. All the lesions subsided almost completely with a single course of treatment. He was given five more courses of chemotherapy, following which he was completely free of symptoms. One month after completion of chemotherapy, he presented with multiple plaques on the face, trunk and limbs. They were identical to the previous lesions, but were more numerous. The left axillary lymph nodes were enlarged. Biopsies from the skin and lymph nodes showed the same histopathological findings. A chest X-ray and ultrasonogram of the abdomen showed no internal organ involvement. He was put on IEP regime with ifosfamide, etoposide and cisplatin in January 2006. He has completed two courses of chemotherapy with partial response.
Discussion
NHL is a heterogeneous group of malignancies of the lymphoid system, characterized by an abnormal clonal proliferation of B cells (70%), T cells (30%) or both.[2] The WHO classification categorizes ALCL under mature T cell neoplasms.[3] The European Organization for Research and Treatment of Cancer (EORTC) classifies ALCL as an indolent T cell lymphoma.[4]
Anaplastic large cell lymphoma can be CD 30+ or CD 30-. CD 30 is a member of the cell surface receptors for tumor necrosis factor. It was originally identified on Reed-Sternberg cells in Hodgkin′s disease. It is induced by activation and is seen in cells around lymph node follicle, HIV infected cells, embryonal carcinoma and CD 30+ lymphoma.
Irrespective of the morphology of the tumor cells (anaplastic, immunoblastic or pleomorphic large cells) the clinical presentation and behavior of ALCL are identical. CD30+ ALCL occurs mainly in adults with male to female ratio of 1.5:1. It can occur primarily in the skin or secondary cutaneous involvement can occur from systemic type. Primary cutaneous type presents with nodules and tumors with central ulceration and may undergo spontaneous regression. Systemic involvement is unusual. Secondary regional lymphadenopathy is seen in only a quarter of cases and is not necessarily associated with unfavorable prognosis.[6] Patients with CD 30- cutaneous large cell lymphoma also present with a similar clinical picture but lesions are more commonly widespread, with poorer prognosis.
Prognosis is generally excellent for CD 30+ primary cutaneous ALCL. Although not extensively reported, multifocal primary cutaneous ALCL tends to relapse after systemic chemotherapy and is generally considered more prone to progress to systemic disease. For solitary and localized skin lesions, radiotherapy is the preferred mode of treatment. Successful treatment with PUVA in combination with interferon has been reported. For more generalized skin lesions or extra-cutaneous dissemination, multiagent chemotherapy should be considered.
Acknowledgements
We gratefully acknowledge the expert advice and help rendered by Dr. K. P. Aravindan, Prof. and Head of the Dept., and Dr. Anupama Manjula, Assistant Professor, of the Dept. of Pathology, Medical College, Calicut and Dr. Rekha. A. Nair, Addl. Prof. of Pathology, Regional Cancer Centre, Thiruvananthapuram.
| 1. |
Weiss ML, Chan CW, Schnitzer B. Lymph nodes. In : Damjanov I, Linder J, editors. Anderson's Pathology. 10th ed. Missouri: Mosby; 1996. p. 1180.
[Google Scholar]
|
| 2. |
Prosnitz RL, Manch MP. Non Hodgkin's lymphoma. In : Perez CA, Brady LW, Halperin CE, Schmidt, Ullrich RK, editors. Principles and Practice of Radiation Oncology. 4th ed. Lippincott Williams and Wilkins: Philadelphia; 2004. p. 2064-111.
In : Perez CA, Brady LW, Halperin CE, Schmidt, Ullrich RK, editors. Principles and Practice of Radiation Oncology. 4th ed. Lippincott Williams and Wilkins: Philadelphia; 2004. p. 2064-111.'>[Google Scholar]
|
| 3. |
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, et al . The World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues. Report of the Clinical Advisory Committee meeting, Airlie House, Virginia, November, 1997. Ann Oncol 1999;10:1419-32.
[Google Scholar]
|
| 4. |
Williemze R, Kerl H, Sterry W, Berti E, Cerroni L, Chimenti S, et al . EORTC classification for primary cutaneous lymphomas. A proposal from the cutaneous lymphoma study group of the European Organisation for Research and Treatment of Cancer. Blood 1997;90:354-71.
[Google Scholar]
|
| 5. |
Sterry W, Mareus MJ. Other systemic lymphomas with skin infiltration. In : Freedberg MI, Eisen ZA, Wolff K, Austen FK, editors. Fitzpatrick's Dermatology in general medicine, 6th ed. McGraw-Hill: New York; 2003. p. 1558-67.
[Google Scholar]
|
| 6. |
Shehan MJ, Kalaaji NA, Markovic SN, Ahmed I. Management of multifocal primary cutaneous CD 30+ anaplastic large cell lymphoma. J Am Acad Dermatol 2004;51:103-10.
[Google Scholar]
|
Fulltext Views
2,756
PDF downloads
1,223





