Translate this page into:
MDT-MB therapy in paucibacillary leprosy: A clinicopathological assessment
2 Departments of Pathology, Rajah Muthiah Medical College Hospital Annamalai University, Annamalai Nagar, Tamil Nadu, India
Correspondence Address:
P V S Prasad
No. 88, AUTA Nagar, Sivapuri - Post, Annamalai Nagar - 608 002, Tamil Nadu
India
| How to cite this article: Prasad P V, Babu A, Kaviarasan P K, Viswanathan P, Tippoo R. MDT-MB therapy in paucibacillary leprosy: A clinicopathological assessment. Indian J Dermatol Venereol Leprol 2005;71:242-245 |
Abstract
BACKGROUND: The World Health Organization recommends treatment regimens for paucibacillary (PB) and multibacillary (MB) leprosy, which differ in their duration and components. Hence accurate classification of the disease is required. To overcome difficulties in classification Uniform Multi Drug Therapy (U-MDT) has been recommended. AIM : To evaluate the benefit of adding clofazimine to paucibacillary regimens in leprosy patients by measuring clinical and histological resolution. METHODS: Forty-four paucibacillary patients were included in the study. Twenty-two patients were given MDT-PB regimen and the remaining MDT-MB regimen for six months . Skin biopsies were done before the commencement and at the end of treatment. Clinical and histological resolutions were measured according to the standard criteria a laid down. The results were analyzed using Fishers' test and Crammers' V test. RESULTS: Clinical improvement was observed in 90.9% in the MB group as compared to 27.3% in the PB group. Regression in the nerve swelling was observed in 70% in the MB group and in 37.5% in the PB group while histological resolution was observed in 72.8% and 54.5% respectively. CONCLUSIONS: Addition of clofazimine helps to resolve leprosy lesions both clinically and histologically, thus justifying the concept of Uniform MDT regimen for all patients.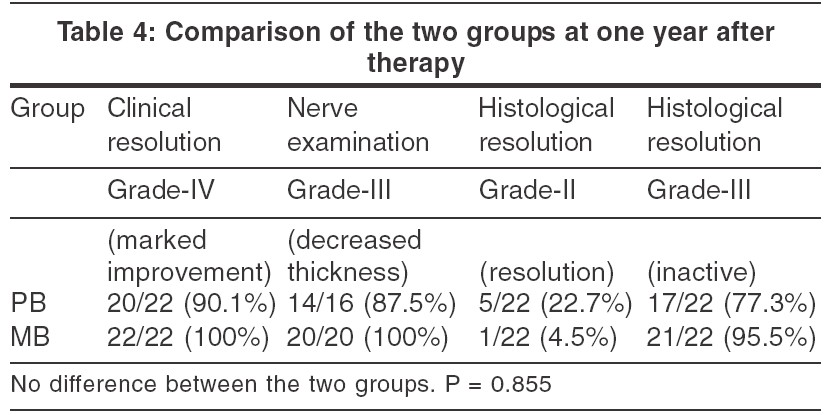
INTRODUCTION
Leprosy, is a chronic infectious disease affecting mainly the skin and nerves.[1] The World Health Organization (WHO) classified leprosy into paucibacillary (PB) and multibacillary (MB) on the basis of the number of patches on the skin and number of nerves involved. PB patients are those who have five or less than five patches and up to one nerve trunk involvement. WHO recommended Multi Drug Therapy (MDT) for the treatment of leprosy in the year 1981. MDT improved the compliance of patients. However, persisting activity, reactions and relapses have been observed in a section of these patients, and above all classification itself poses problems in the field setup at times.[2] To overcome this, and to benefit the field staff, Uniform MDT (U-MDT) has been advocated. Clofazimine-containing regimen have an added advantage that the same drugs may be given for varying durations depending upon the clinical classification.[3],[4] Hence this study was conducted to evaluate the clinical and histological advantages of adding clofazimine in PB patients.
MATERIALS AND METHODS
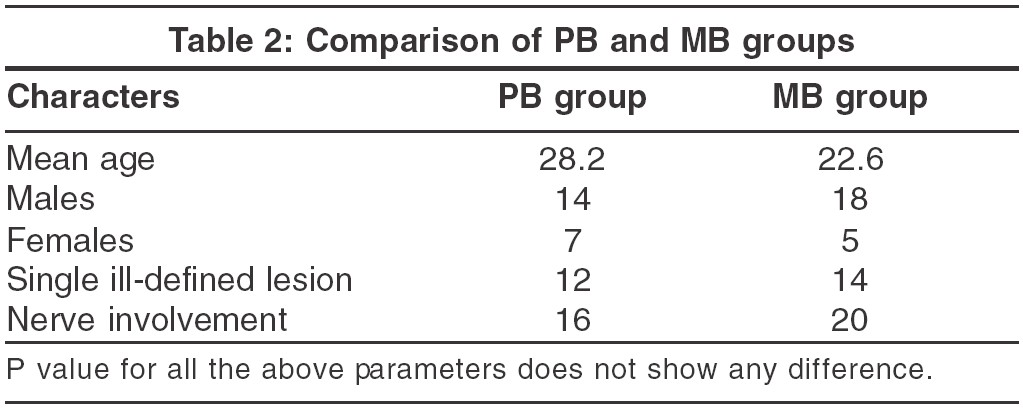
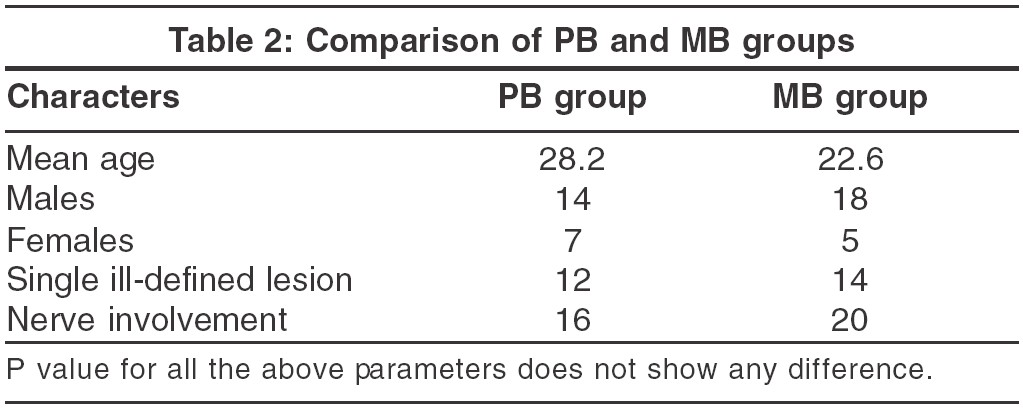
All new patients who were diagnosed to have PB leprosy attending the outpatient department of the Rajah Muthiah Medical College Hospital, Annamalai University, Chidambaram between January 2001 to June 2002 were included in the study. The patients were classified according to the WHO guidelines. The number and morphology of lesions and anaesthesia were recorded. The site and thickening of the nerve trunk was noted. Slit-skin smear was done from all patients and only smear-negative patients were included. Skin biopsy was done after obtaining a written consent from the margin of the lesion. Histology of PB leprosy was considered when there was a granuloma composed of epithelioid cells with a rim of lymphocytes along with dermal Langhan′s giant cells and cutaneous nerves showing granulomatous destruction with intact perineurium. After confirming the diagnosis alternate patients were started on PB and MB regimens. Patients were followed up every month when changes in the skin and nerve trunk lesions were recorded. A complete evaluation was done at the end of six months. Criteria for clinical resolution in the skin and nerve lesions, histological resolution in the dermal infiltrate and in the nerves are shown in [Table - 1]. The results were analyzed by Fisher′s exact test and by Cramer′s V test.
RESULTS
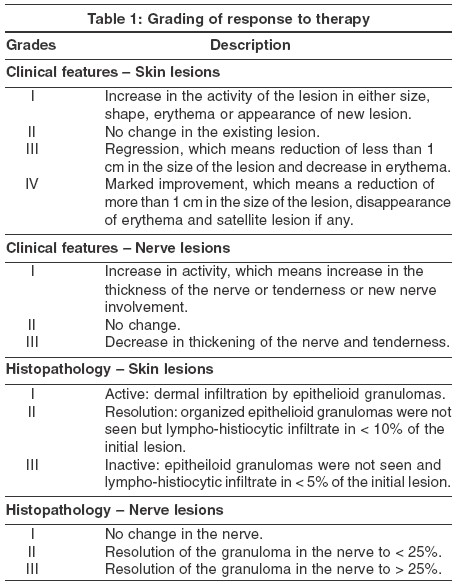
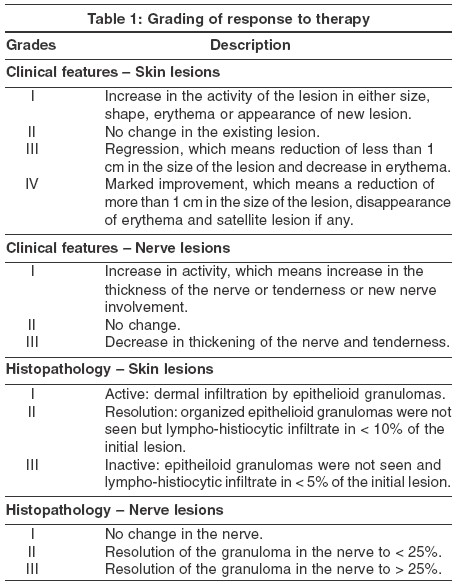
The number of new leprosy patients during the study period comprised 0.35% of all new dermatology outpatients. Fifty patients were enrolled in the study. One patient who was clinically diagnosed as PB leprosy showed many macrophages in the biopsy and hence was not included in the analysis. Another five patients dropped out of the study for various reasons. Forty-four patients completed the study including one year of follow-up. There were 32 males and 12 females with a ratio of 4:1.5. The age group ranged from 10 to 72 years with a mean age of 25.8 years. Twenty-eight patients (63.7%) were in the age group of 11-30 years. Twenty-six patients (89%) had single ill-defined plaque with satellite lesions. Six patients had two lesions and 12 patients had three lesions. Nerve trunk was thickened in 36 patients (81.8%) only. The two groups receiving PB and MB leprosy are compared as shown in [Table - 2].
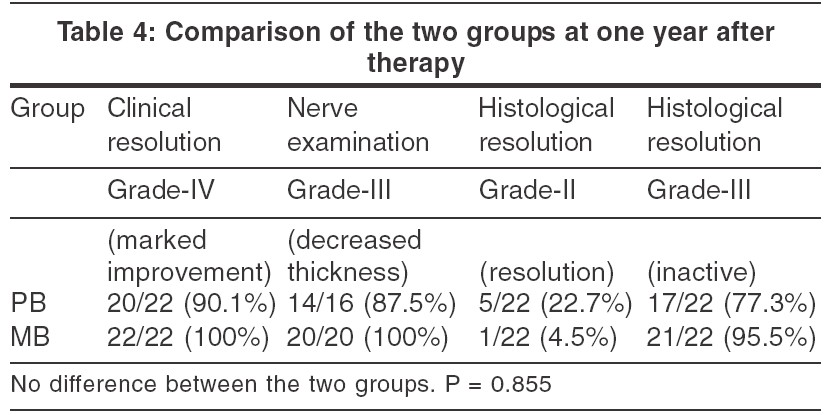
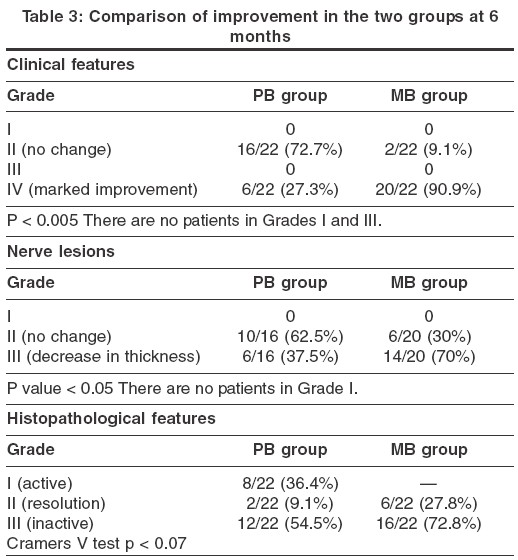
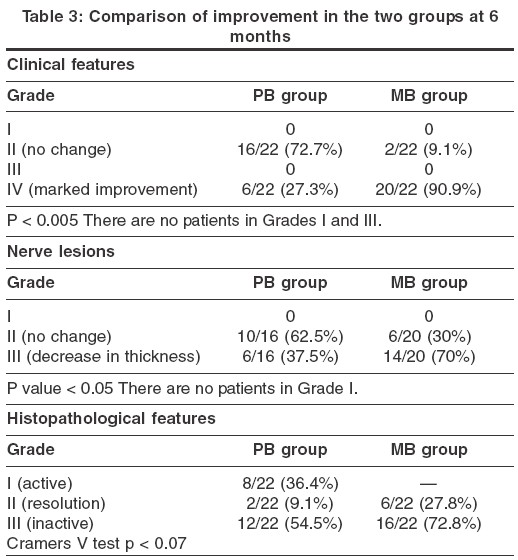
Clinical improvement shown in [Table - 3], revealed that out of 26 patients with Grade-IV resolution, 20 patients received MB regimen. Improvement in nerve thickening as shown in [Table - 3], revealed 70% improvement with the MB regimen. Histological changes at the end of therapy between the two groups were compared and are shown in [Table - 3]. Features of inactivity were seen in 12 out of 22 PB patients and in 16 out of 22 MB patients. We did not encounter side effects of anti-leprosy drugs in the study group. One patient on MB regimen developed reversal reaction, during the last month of treatment, which resolved with a short course of corticosteroids. The clinical and histological parameters for patients followed up for one year are shown in [Table - 4].
DISCUSSION
Epidemiologic parameters like age, sex and duration of the disease were comparable with other studies in the country.[5] There was also no statistical difference among the various parameters between the PB and MB groups. The criteria for clinical and histological resolution were modified from Kar et al.[6] In contrast to bacillary positive patients, the cure or end point of treatment of smear-negative patients has been more difficult to define. The PB regimen has been in use for more than 15 years. On the whole the experience of workers in several parts of the world has been quite encouraging. However, a few difficulties have been encountered. The continued visibility of a clinically active lesion in a proportion of patients at the end of 6 months′ therapy has been observed in practically all studies. The proportion of cases with active disease at the end of the stipulated six months of treatment varied from 10 to 67% in various studies at the field and institutional levels. On the follow-up of these patients clinical activity gradually subsided and the disease was cured in 30 to 80%. The remaining patients continued to have the disease beyond a period of 18 months. For this reason some workers recommended continuation of dapsone or continuation of PB regimen for six more months.[6] Late reversal reaction was another problem observed, which occurred after six months of stopping treatment. For this group also, extended therapy has been suggested. The same regimen for PB and MB patients is the first step in the simplification of the treatment of leprosy.
In our study, addition of clofazimine has proved its worth. Ninety-one per cent of patients have shown Grade-IV clinical improvement. Clofazimine is also a weak bactericidal drug, which has a long half-life of 70 days. It also has anti-inflammatory property. Clofazimine, which binds to mycobacterial DNA, inhibits mycobacterial growth and exerts a slow bactericidal effect on M. leprae . As continued inflammatory response results in persistent activity in leprosy, addition of clofazimine helps in PB patients.
We have adopted a criterion, to assess the improvement in the nerve, which is similar to the clinical criterion. There are no definite parameters available to assess cure for neuritic leprosy cases.[6] Criteria for assessment and cure are highly controversial. Among the 36 patients with one nerve trunk involvement, MB regimen showed 70% improvement and hence we considered it superior.
When the pathology is evident on the surface, whether it is right to call the disease as cured, has remained an issue. The basic misconception about the Fixed Duration Therapy (FDT) in PB leprosy, is the time taken for regression of granuloma. Job et al[7] in their study conducted in 1997 found that 11 out of 22 patients remained active after six months and only three after 18 months. He recommended anti-inflammatory drugs or chemotherapy whenever necessary. Ebenezer et al[8] followed up 24 patients and found that only eight patients remained active after six months. She stressed the need for sequential histopathological studies and longer follow-up of patients with active lesions at the time of completion of treatment. In our study we found that granulomas regressed faster if clofazimine was added to the PB regimen. All 22 patients showed resolution and 73% revealed Grade-III resolution in comparison to 55% in the PB group.
After one year of follow-up, the study group revealed that all patients in the MB regimen group showed clinical resolution. This included two patients who were in Grade-II initially. In the PB group, except two patients, others showed resolution. Both those cases were males who showed three ill-defined patches and one nerve trunk involvement. Histological resolution occurred much later than clinical resolution. Five out of eight patients with PB therapy moved from Grade I to II after one year of treatment. Similarly, five out of six patients with MB therapy moved from Grade II to III. These findings are comparable with similar studies by Job.[7] The final outcome in both the groups is almost similar and there is no statistical difference.
On the contrary, all 26 patients who initially showed erythematous ill-defined plaques responded well to treatment and the lesions showed a Grade III response at the end of one year post-treatment. Studies at the Central Jalma Institute of Leprosy have shown that a good number of patients diagnosed as PB leprosy clinically were acid-fast bacilli positive in the skin smear indicating their chances of getting inadequate treatment under the present program. Besides these patients would be prone for relapse.[9] Clofazimine is cost-effective, especially when compared to its advantages. To conclude, the addition of clofazimine in the PB regimen is fully justified adding strength to the concept of Uniform MDT (U-MDT).
| 1. |
WHO Expert Committee on Leprosy. Seventh Report. WHO Technical Reports Series no: 847. World Health Organization, Geneva 1998.
[Google Scholar]
|
| 2. |
Katoch K, Ramanathan U, Natarajan M, Bagga AK, Bhatia AS, Saxena RK, et al . Relapses in paucibacillary patients after short-term regimens containing rifampicin. Int J Lepr Other Mycobact Dis 1989;57:458-64.
[Google Scholar]
|
| 3. |
Katoch K, Nagarajan M, Katoch VM, Singh HB, Bhatia AS. Chemotherapy trial in paucibacillary leprosy using clofazimine. Indian J Lepr 1999;71:311-24.
[Google Scholar]
|
| 4. |
Katoch K. Therapeutic prospects for pauci-bacillary leprosy. Indian J Lepr 2000:72:351-61.
[Google Scholar]
|
| 5. |
Reddy BS, Parthasarathy A, Salt MA. Age at onset of leprosy. Indian J Dermatol Venereol Leprol 1996:56:23-5.
[Google Scholar]
|
| 6. |
Kar PK, Jha PK, Panayach JS, Snehi PS. A clinico-pathological study of multidrug regimen in paucibacillary leprosy. Indian J Lepr 1988;60:235-41.
[Google Scholar]
|
| 7. |
Job CK, Jayakumar J, Aschhof M. Delayed resolution versus treatment failure in paucibacillary patients under six months fixed duration therapy. Indian J Lepr 1997;69:131-42.
[Google Scholar]
|
| 8. |
Ebenezer G, Suneeetha S, Arunthathi S. Clinical and histological activity in paucibacillary patients after fixed duration therapy. Lepr Rev 1997;68:218-24
[Google Scholar]
|
| 9. |
Sengupta U. The research achievements of the Central Jalma Institute of Leprosy, Agra. ICMR Bulletin 2001;31:2.
[Google Scholar]
|
Fulltext Views
7,909
PDF downloads
2,206





