Translate this page into:
Tzanck cytology smear in diagnosis of cutaneous talaromycosis (penicilliosis)
Corresponding author: Dr. Shau-Kong Lai, Department of Pathology, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, 43400 Serdang, Selangor, Malaysia. pathsklai@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Lai SK, Rauf NA, Preet KR, Tan LJ. Tzanck cytology smear in diagnosis of cutaneous talaromycosis (penicilliosis). Indian J Dermatol Venereol Leprol 2023;89:233-6.
Abstract
Talaromyces marneffei infection is an AIDS-defining illness in South and Southeast Asia. Travel-related talaromycosis is being increasingly recognized in non-endemic areas too. It is a potentially fatal infection with rapid deterioration, if left untreated. Usage of Tzanck cytology smear for rapid diagnosis of T. marneffei is rarely described. In this case study, we report a man who presented with altered behaviour, headache, fever and cutaneous lesions. Tzanck smear test, skin biopsy and blood culture showed presence of T. marneffei. The cytomorphology findings of T. marneffei in Tzanck cytology smear were described. In conclusion, Tzanck smear is a simple and inexpensive test in establishing a rapid clinical diagnosis of talaromycosis before the culture is reported.
Keywords
Cytology
penicilliosis
skin
talaromycosis
Tzanck
Introduction
Cutaneous cytology was first used by Arnault Tzanck in 1947 for diagnosing skin diseases. Although it was suggested as a reliable technique, the practice of Tzanck smears for the following six decades after its discovery, was limited.1 Tzanck smear test is mostly used for the diagnosis of infection by herpes simplex or varicella-zoster virus. Recently, the diagnostic usage has been expanded to erosive-vesiculobullous, pustular, granulomatous, pigmented and neoplastic diseases, but usage for Talaromyces marneffei detection is rarely described.2
Talaromycosis is an infection caused by dimorphic fungus Penicillium marneffei, which is now renamed as Talaromyces marneffei. T. marneffei is an AIDS-defining illness in South and Southeast Asia, ranked just after tuberculosis and cryptococcosis. Travel-related talaromycosis is increasingly recognized in non-endemic areas too.3 We report a case of T. marneffei infection in a young patient, describing its clinical features and pathology findings.
Case Report
A 33-year-old Malaysian man, with underlying diabetes mellitus and history of melioidosis, presented with altered behaviour for a month, associated with fever and headache. He was found unresponsive at home and was brought to the emergency department. His Glasgow Coma Scale score was 7/15 on arrival and he was intubated. His serology test was positive for human immunodeficiency virus (HIV) infection. Computerised tomography of the brain revealed obstructive hydrocephalus with mixed density over the posterior fossa.An external ventricular drain was inserted. He was empirically treated with anti-fungal, anti-tuberculosis and anti-toxoplasma medication. He also had multiple umbilicated papules over the face, upper chest and the proximal upper limbs. A Tzanck smear test and skin biopsy were performed.
The Tzanck smear was air dried and then fixed in methanol for 15 minutes. The smear was subsequently stained with Giemsa working solution for 20 minutes. After being rinsed with tap water, it was placed in phosphate buffer working solution for a few seconds. The smear was left to air dry again, before being mounted with a coverslip. The skin biopsy underwent standard histopathologic processing by being formalin-fixed, paraffin embedded, with hematoxylin and eosin (H&E) staining.
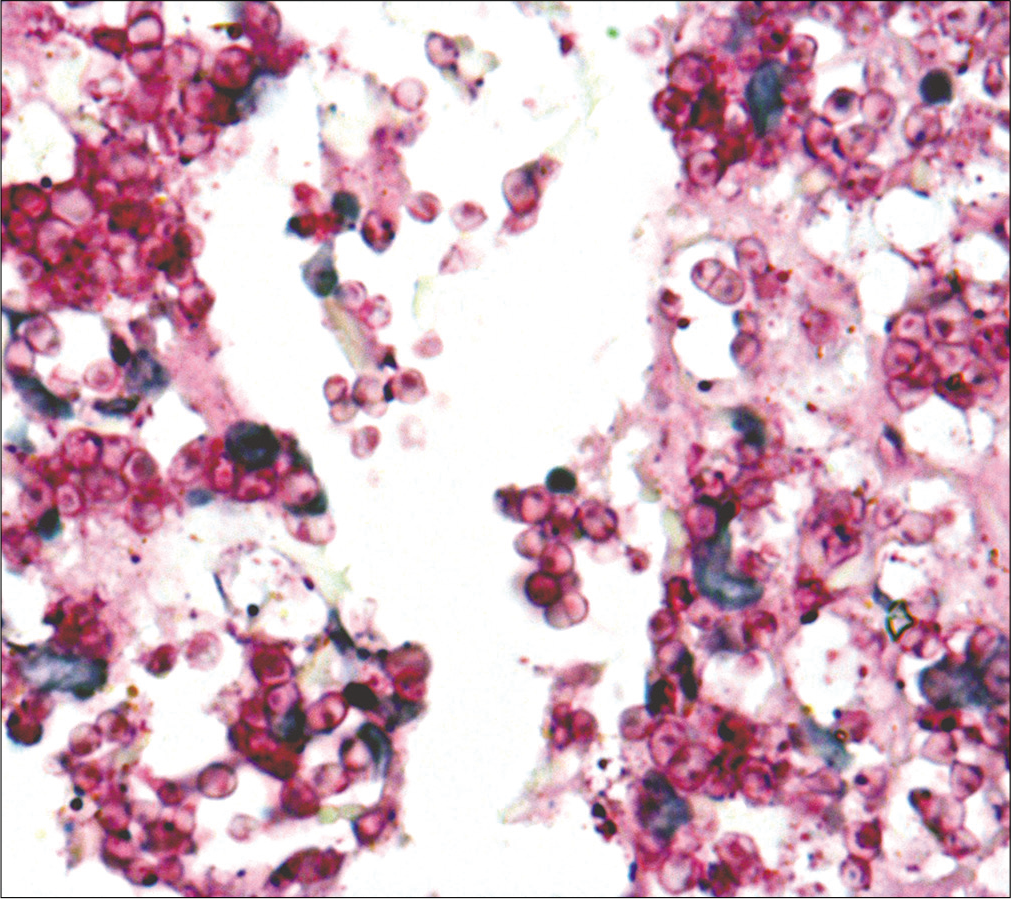
Microscopic examination of the smear showed many yeast cells located within and outside of the histiocytes. The yeast cells were round to oval and measuring 2-5 μm in diameter. Occasional clear cross wall septa were seen [Figure 1]. Microscopic examination of the skin biopsy revealed mildly acanthotic epidermis. The upper dermis displayed numerous round to oval yeast cells, that are free lying and within the cytoplasm of histiocytes. Foci of necrosis and mild neutrophilic infiltration were noted. The deep dermis and subcutaneous tissue were unremarkable. There was no granuloma present. Periodic acid Schiff stain showed distinctive central septa of the fungal yeast [Figure 2].

- Tzanck smear shows abundant unicellular round to oval T. marneffei yeast cells located within and outside of the histiocytes (Giemsa stain, ×400)
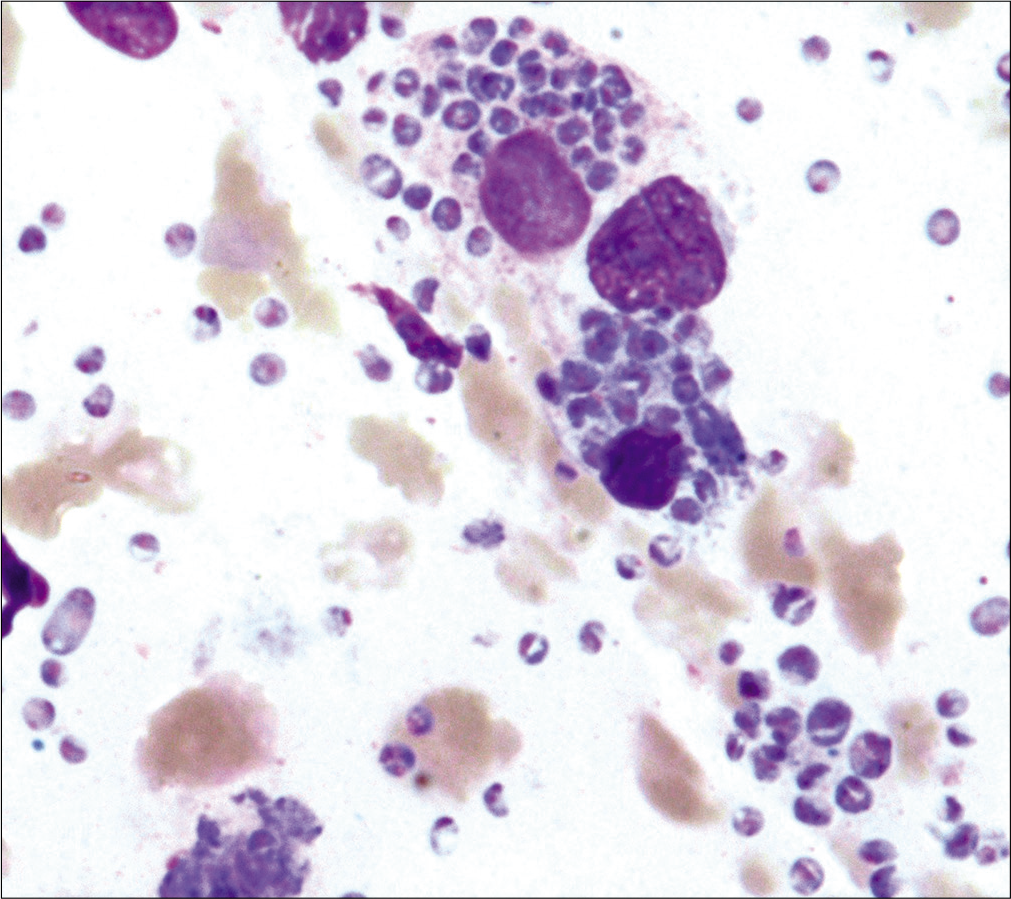
- Tzanck smear shows T. marneffei yeast cells displaying clear cross wall septa (Giemsa stain, ×1000)
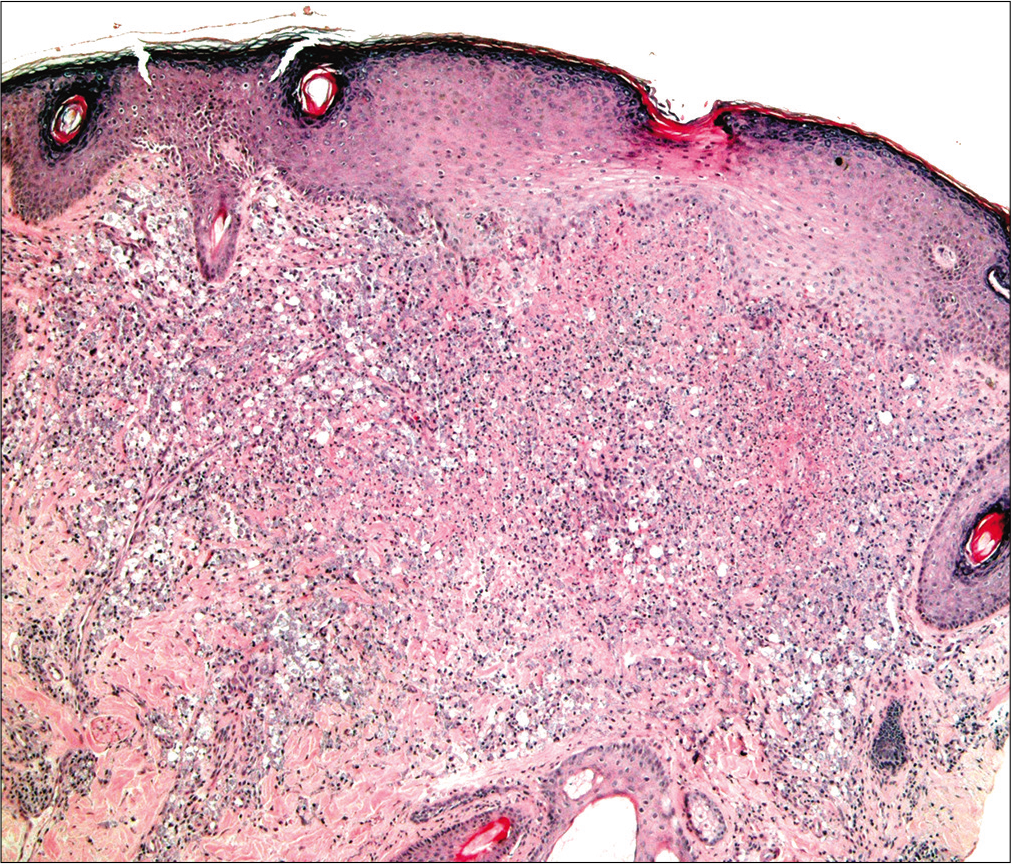
- Skin biopsy shows the upper dermis displaying numerous T. marneffei yeast cells with foci of necrosis (H and E, ×20)
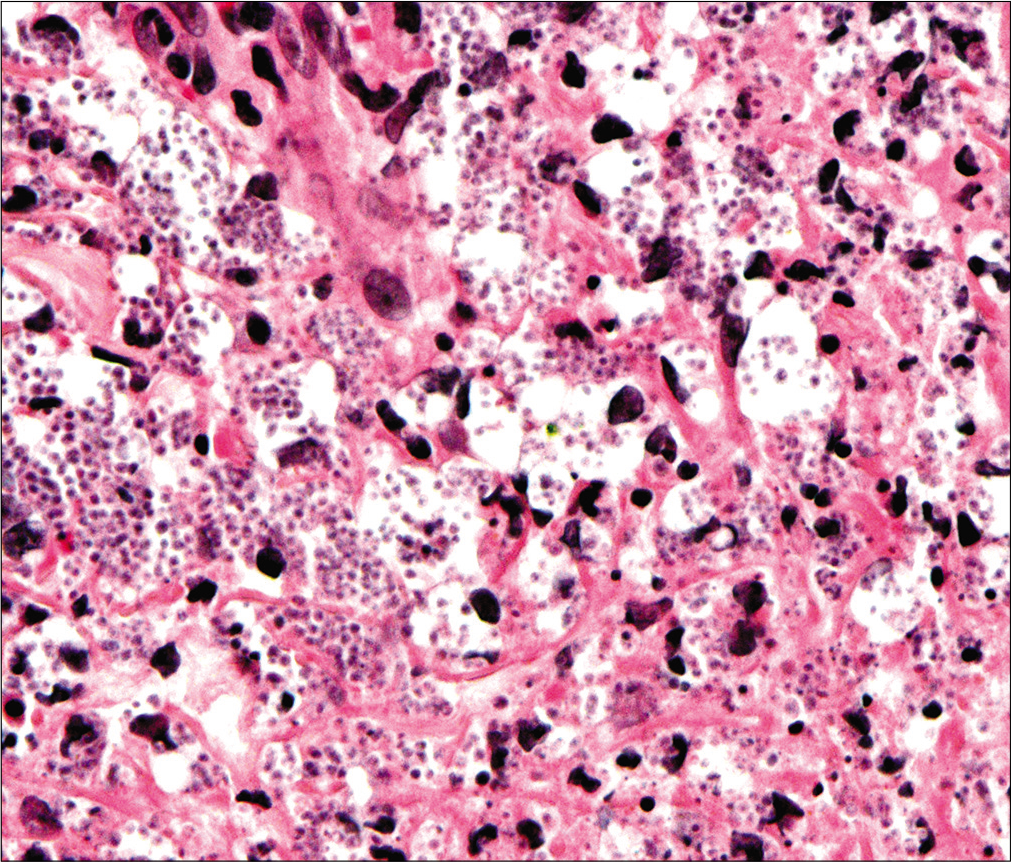
- Many T. marneffei yeast cells are within the cytoplasm of histiocytes (H and E, ×400)
-
T. marneffei yeasts displaying distinctive central septa with pill-like appearance (Periodic acid Schiff, ×1000)
The patient blood cultures repeatedly yielded typical T. marneffei growth. He eventually passed away, 9 days after admission, despite treatment.
Discussion
Talaromycosis is a potentially fatal infection with rapid deterioration, if left untreated.4,5 Bamboo rat is the enzootic reservoir.6 Human infection occurs through inhalation of T. marneffei conidia. It is phagocytized by alveolar macrophages and grows into intracellular yeast. Subsequently, the organism disseminates to other organs.The hyphal form was never reported in vivo, as the phagocytized conidia develops directly into yeast phase without first forming hyphae.3
The clinical spectrum of talaromycosis ranges from isolated cutaneous infection to disseminated infection. Cutaneous talaromycosis commonly presents as multiple dome-shaped, skin-coloured, umbilicated papules, with or without central necrosis on the face and trunk.7 Dermoscopic appearances may aid in early diagnosis.8 T. marneffei can be detected from the cutaneous lesion by cytology smear, skin biopsy or culture. Concurrent opportunistic infection such as candidiasis, tuberculosis, toxoplasmosis or Pneumocystis jirovecii infection was reported in up to 40% of cases.7 These other infections may also present with cutaneous lesions. Laboratory detection of the causative organism is therefore important for the correct diagnosis.
Laboratory diagnosis of talaromycosis requires isolation of the fungus from clinical specimens and microscopic demonstration of intracellular T. marneffei organism in the infected tissue.3 The organism can be demonstrated by cytology or in the histology specimen. Commonly, cytology smears are taken from skin lesions, ulcer secretions, pus or marrow aspirations.5 Microscopically, T. marneffei appears as a unicellular, round to oval, often curved or sausage-like organism, ranging from two to five μm in diameter. The yeast cells are located both inside and outside of the histiocytes. T. marneffei yeast characteristically divide by cross wall formation, as it multiplies by fission rather than budding.3,5 The histopathology of the skin lesion frequently shows microabscesses in the upper and middle dermis, with necrotic areas containing many lymphocytes and neutrophils. The characteristic yeasts are frequently found in large numbers, both intracellular and extracellular. Periodic acid-Schiff stain (PAS) and Gomori methenamine silver stain (GMS) are positive and highlight the cross-wall formation.5
The most important differential diagnoses of talaromycosis are histoplasmosis and leishmaniasis, as they are intracytoplasmic organisms of similar size. Histoplasma capsulatum yeast cells are oval, measuring two to five μm in diameter, and predominantly found within the cytoplasm of histiocytes, rather than in the extracellular space. In Tzanck smear with Giemsa stain, H. capsulatum shows characteristic narrow based budding and blue cell wall, with clear halo around the yeast cells,thus differentiating it from talaromycosis.2 The leishmaniasis amastigotes are oval cells measuring two to five μm with an eccentric nucleus, present inside and outside of histiocytes. A small kinetoplast near the nucleus and the presence of the promastigote form distinguishes it from talaromycosis.2,9
Fungal culture is the gold standard method for the diagnosis of talaromycosis. One study reported high sensitivity of cultures from bone marrow aspiration (100%), skin biopsy (95%) and blood (84%).10 The ability to grow as a mycelium at 25°C and as a yeast at 37°C is the unique thermal dimorphism feature of T. marneffei.3 However, the median time of positive skin or blood cultures was four to five days. The culture may take up to 14 days and this results in diagnostic delay, with increased mortality.10 In contrast, Tzanck smear test is faster and readily available within hours.
Conclusion
Talaromyces marneffei displays characteristic microscopic appearance in Tzanck smear. Tzanck smear is an easy and inexpensive test. It can be very useful in rapid diagnosis of cutaneous talaromycosis before the culture is reported.
Declaration of patient consent
Patient's consent not required as patient's identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Tzanck smear, an old test for the new millennium: When and how. Int J Dermatol. 1999;38:830-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous Cytology and Tzanck Smear Test In: Cham Switzerland Cham. Switzerland: Springer; 2019.
- [CrossRef] [Google Scholar]
- Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev. 2006;19:95-1.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical presentations and outcomes of Penicillium marneffei infections: A series from 1994 to 2004. Hong Kong Med J. 2008;14:103.
- [Google Scholar]
- Fifteen cases of penicilliosis in Guangdong, China. Mycopathologia. 2004;158:151-5.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Rhizomys pruinosus as a natural animal host of Penicillium marneffei in Guangdong, China. Microbial Biotechnol. 2015;8:659-64.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective review on successful management of Penicillium marneffei infections in patients with advanced HIV in Hospital Sungai Buloh. Med J Malaysia. 2012;67:66-70.
- [Google Scholar]
- Dermoscopic manifestations of Talaromyces (Penicillium) marneffei infection in an AIDS patient. Indian J Dermatol Venereol Leprol. 2019;85:348.
- [CrossRef] [PubMed] [Google Scholar]
- Is the amastigote form of Leishmania the only form found in humans infected with cutaneous leishmaniasis? Lab Med. 2008;39:38-41.
- [CrossRef] [Google Scholar]
- Epidemiology, seasonality, and predictors of outcome of AIDS associated Penicillium marneffei infection in Ho Chi Minh City, Viet Nam. Clin Infect Dis. 2011;52:945-52.
- [CrossRef] [PubMed] [Google Scholar]






