Translate this page into:
Generalized erythematous and hypopigmented papules and nodules in a young female
Corresponding author: Dr. Geeti Khullar, Department of Dermatology and Sexually Transmitted Diseases, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110 029, India. geetikhullar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Khunger N, Khullar G, Mann KK, Yadav AK. Generalized erythematous and hypopigmented papules and nodules in a young female. Indian J Dermatol Venereol Leprol 2022;88:527-30.
A 22-year-old woman presented with a 4-year history of asymptomatic papules and nodules all over her body. The lesions started on her legs and gradually spread to thighs, upper extremities, trunk and face. She denied any current or past history of systemic complaints. Cutaneous examination revealed multiple discrete to confluent, firm, erythematous to violaceous papules and nodules, measuring 0.5 to 1 cm in size on the face, trunk, upper and lower extremities [Figure 1a]. Multiple discrete to confluent, ill-defined infiltrated hypopigmented papules were also present on the upper lateral and lower back and arms [Figure 1b]. Mucosa, scalp, palms and soles were spared. There was no lymphadenopathy. Sensory, motor, peripheral nerves, ocular and other systemic examination revealed no abnormality. The differential diagnoses considered clinically were post kala-azar dermal leishmaniasis, sarcoidosis, non-Langerhans cell histiocytosis and lepromatous leprosy. Ziehl-Neelsen and Giemsa stains performed on slit skin smears from ear lobes, erythematous nodule and hypopigmented papule were negative. Histopathological examination from both types of lesions demonstrated sheets of histiocytic cells with irregular-shaped elongated vesicular nuclei and abundant pale eosinophilic cytoplasm in the upper and mid-dermis. Some of these cells had reniform nuclei and intranuclear longitudinal grooves. These cells were interspersed with lymphocytes, few eosinophils and multinucleated giant cells [Figures 2a and b]. Epidermotropism was absent. Immunohistochemical analysis revealed that the histiocytes were diffusely and strongly positive for CD1a, S-100 protein, CD68 and negative for CD207 (Langerin) [Figures 3a and b]. Hemogram, peripheral blood smear and biochemical investigations including serum calcium and angiotensin-converting enzyme levels were within normal limits. Immunochromatographic strip test for rK39 antigen was negative. Mantoux test was positive with an induration of 10 mm. Computed tomography scan of the chest and abdomen and skeletal survey did not reveal any abnormality.

- Multiple erythematous to violaceous papules and nodules on the right upper limb

- Discrete to confluent skin-colored to hypopigmented ill-defined infiltrated papules on the upper lateral and lower back
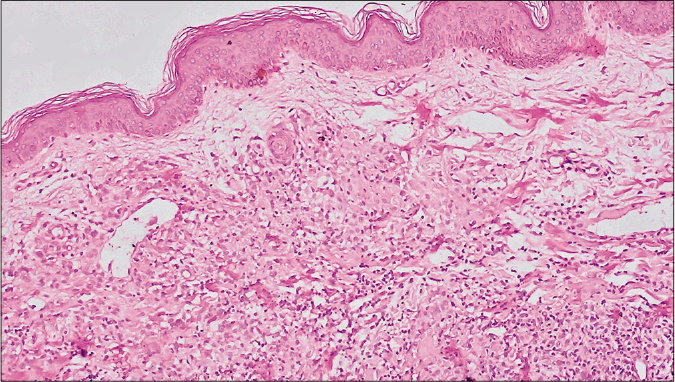
- Epidermis is unremarkable. A thin grenz zone separates the epidermis from the dermal infiltrate. There is diffuse infiltrate of pale staining cells interspersed with darkly stained cells in the dermis (H and E, ×100)
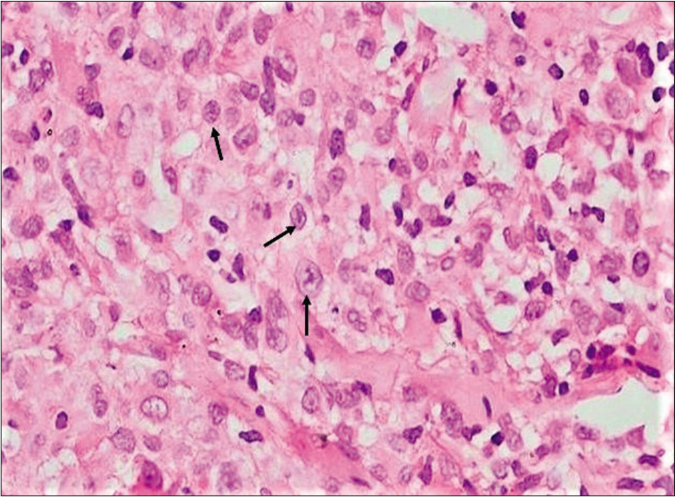
- There is dense dermal infiltrate of large histiocytic cells with abundant pale eosinophilic cytoplasm and vesicular elongated nuclei, some of these having intranuclear longitudinal grooves giving a coffee-bean appearance (black arrows) (H and E, ×400)
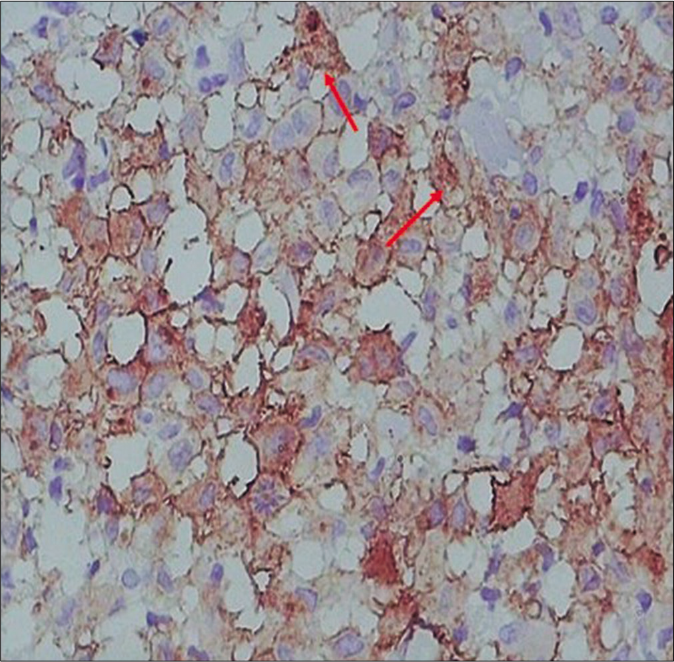
- The histiocytes are strongly positive for CD1a (red arrows) (CD1a, ×400)
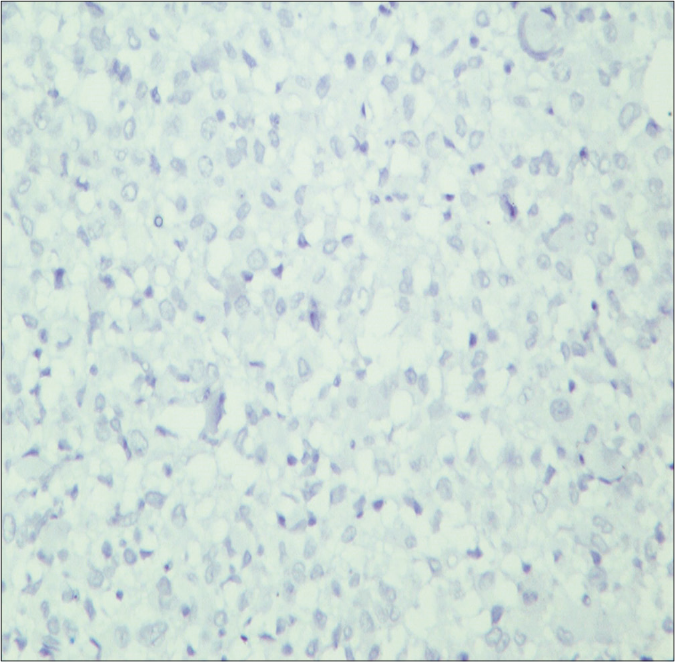
- The histiocytes are negative for langerin (CD207, ×400)
What is your diagnosis?
Diagnosis
Indeterminate cell histiocytosis
Discussion
Indeterminate cell histiocytosis is a rare proliferative disorder of dendritic cells characterized by immunophenotypic features of both Langerhans cell histiocytosis and non Langerhans cell histiocytosis, with absence of Birbeck granules on electron microscopy. 1 In 2008, indeterminate cell histiocytosis was included in the World Health Organization classification of tumors of hematopoietic and lymphoid tissue and in the revised classification in 2016, it was placed under the ‘L (Langerhans)’ group of histiocytosis.2
Due to paucity of reported cases, the exact pathogenesis of indeterminate cell histiocytosis is not understood. It is considered to arise from proliferation of indeterminate cells that get locally arrested in the dermis before migration to the epidermis or to the regional lymph nodes.1 Based on this, indeterminate cells are considered as immature dendritic cells which further differentiate into Langerhans cells and interstitial dendritic cells. Another theory suggests that indeterminate cell histiocytosis possibly arises from dedifferentiation of B- lymphocytes, as it has been reported to be associated with development of B-cell lymphoma.1 It has also been reported to be triggered by scabies and pityriasis rosea, suggestive of a reactive process.1
Indeterminate cell histiocytosis is predominantly seen in adults as either solitary, localized or widespread, usually asymptomatic reddish-brown papules or nodules on the trunk and extremities. Extracutaneous manifestations although uncommon, have been reported to involve lymph nodes, bone, cornea and conjunctiva.3 Histologically, it demonstrates diffuse or nodular dermal aggregates of histiocytic cells with abundant, pale eosinophilic cytoplasm and oval to elongated irregular nuclei. Some of these cells exhibit intranuclear grooves. Immunoreactivity for CD1a and S-100 is described in 96% of cases of indeterminate cell histiocytosis and CD68 in 91% of the cases.2
Lack of significant number of eosinophils, infrequent epidermotropism and absence of expression of langerin on immunohistochemistry reliably distinguish indeterminate cell histiocytosis from Langerhans cell histiocytosis.2,3 Langerin staining has been used as a surrogate marker for Birbeck granules seen ultrastructurally. Clinically, generalized eruptive histiocytosis and progressive nodular histiocytosis may also be considered as differential diagnoses, however both of them show only CD68 positivity and lack the expression of CD1a and S-100 protein. The histological, immunophenotypic and ultrastructural findings of indeterminate cell histiocytosis and its differential diagnoses are described in Table 1.2,3
| Microscopic feature | Langerhans cell histiocytosis | Indeterminate cell histiocytosis | Progressive nodular histiocytosis (non-Langerhans cell histiocytosis) |
|---|---|---|---|
| Hematoxylin-eosin stain | Infiltrate comprises of round to oval large epithelioid cells, about 2-3times the size of lymphocyte with coffee-bean shaped vesicular nucleus having longitudinal grooves and inconspicuous nucleoli and abundant pink cytoplasm. These cells are admixed with abundant eosinophils. Epidermotropism is usually present. | Dermal histiocytic infiltrate with Langerhans cell-like morphology. Eosinophils are sparse. Epidermotropism is uncommon. |
Dermal infiltrate of xanthomatized histiocytes, which in late lesions become spindle shaped and are arranged in storiform pattern. Some admixed lymphocytes and giant cells present. No epidermotropism seen. |
| Immunohistochemical markers | Positive for CD1a, S-100, CD68 and langerin (CD207) | Positive for CD1a (96%), S-100 (96%) and CD68 (91%). Negative for langerin | Positive for CD68 and factor XIIIa. Negative for CD1a, S-100 and langerin |
| Electron microscopy | Birbeck granules present | Birbeck granules absent | Birbeck granules absent |
The clinical behaviour of indeterminate cell histiocytosis is usually benign, exhibiting either spontaneous remission, waxing and waning course or stable disease.4 Our patient showed spontaneous partial regression of the lesions. However, long term follow up is needed as it may be rarely complicated by hematologic malignancies.2,5 Various treatment modalities have been described, of which phototherapy (broadband and narrowband ultraviolet B, psoralen and ultraviolet A) has shown good outcome.2 There are anecdotal reports on thalidomide, low dose methotrexate, isotretinoin, pravastatin, total skin electron beam therapy and 5-fluorouracil with coal tar cream for generalised lesions.2,5
Unique features in our case were younger age of onset, presence of hypopigmented lesions and widespread distribution including the face. Although indeterminate cell histiocytosis occurs in all age groups, the median age is 45 years which is higher than that of the present case. The classic lesions are erythematous to yellowish- brown in color and to our knowledge, hypopigmented lesions have not been reported in literature. Facial involvement is also uncommon and may manifest as leonine facies.6
Acknowledgement
Dr. Manoj Kumar Singh, Professor, Department of Pathology, All India Institute of Medical Sciences, New Delhi- 110029, for performing immunohistochemistry for Langerin and providing its photomicrograph.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Indeterminate cell tumor: A rare dendritic neoplasm. Am J Surg Pathol. 2008;32:1868-76.
- [CrossRef] [PubMed] [Google Scholar]
- Indeterminate dendritic cell neoplasm of the skin: A 2 case report and review of the literature. J Cutan Pathol. 2017;44:958-63.
- [CrossRef] [PubMed] [Google Scholar]
- Indeterminate dendritic cell tumor: A report of two new cases lacking the ETV3 NCOA2 translocation and a literature review. Am J Dermatopathol. 2018;40:736-48.
- [CrossRef] [PubMed] [Google Scholar]
- Indeterminate cell histiocytosis: fact or fiction? J Cutan Pathol. 2005;32:552-60.
- [CrossRef] [PubMed] [Google Scholar]
- Indeterminate cell histiocytosis in association with later occurrence of acute myeloblastic leukaemia. Br J Dermatol. 2007;156:1357-61.
- [CrossRef] [PubMed] [Google Scholar]
- Indeterminate cell histiocytosis presenting with leonine facies. Acta Derm Venereol. 2018;98:463-4.
- [CrossRef] [PubMed] [Google Scholar]





