Translate this page into:
Risk factors for poorly controlled and recurrence-prone ingrown toenails treated with nail braces: A retrospective observational study of 238 cases
Corresponding author: Dr. Yu-Chen Huang, Department of Dermatology, Wan Fang Hospital, Taipei Medical University, No. 111, Section 3, Hsing-Long Rd, Taipei 116, Taiwan. dhist2002@yahoo.com.tw
-
Received: ,
Accepted: ,
How to cite this article: Wang HH, Huang YC. Risk factors for poorly controlled and recurrence-prone ingrown toenails treated with nail braces: A retrospective observational study of 238 cases. Indian J Dermatol Venereol Leprol 2022;88:636-40.
Abstract
Background
Nail braces are reportedly effective for treating both acute inflamed and chronic dystrophic type ingrown toenails.
Aims
In this study, risk factors for poorly controlled and recurrence-prone ingrown toenails treated with nail braces were identified.
Methods
We performed a retrospective study on patients with ingrown toenails between June 1, 2015, and May 31, 2018. The last follow-up date was January 31, 2019. Multivariate logistic regression was performed to evaluate the possible factors associated with poorly controlled status (ongoing paronychia during treatment) and recurrence.
Results
There were 120 (244 sides) and 118 patients (167 sides) with chronic dystrophic and acute inflamed type ingrown toenails, respectively. The mean treatment duration and follow-up period were 161.2 ± 98.3 days and 432.7 ± 320.9 days, respectively. Poor control and recurrence were seen in 7.3% (17/232) and 12.2% (27/221) of the patients, respectively. In the multivariate analysis, acute inflamed ingrown toenails, previous nail avulsion, proximal nail fold hypertrophy and more than one affected side remained significantly associated with poorly controlled ingrown toenails. Foot bone deformity was significantly associated with recurrence.
Limitations
This study was a retrospective study so that confounding factors such as comorbidities, body mass index, accompanying nail changes and lifestyle could not be evaluated.
Conclusion
Several risk factors related to poor control and recurrence were identified. Patients could therefore benefit from more suitable treatment plans with reasonable expectation.
Keywords
Ingrown toenails
nail brace
paronychia
recurrence
risk factors
Plain Language Summary
Ingrown nail, which develops when the nail plate edge grows abnormally toward the nail fold, is a disorder commonly seen in skin clinics. This typically causes pain and inflammation and restricts the daily lives of affected individuals. Besides conventional surgical intervention, nail brace has been used as a noninvasive and effective option for treating ingrown nail. In this study, we aimed to investigate the risk factors of poorly controlled and recurrence-prone cases of ingrown toenail treated with nail braces. This study included patients with ingrown toenails treated with nail braces at the Dermatology Clinic at Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan, between June 1, 2015, and May 31, 2018. From this study, we found that acute inflamed type of ingrown toenails, previous nail avulsion, proximal nail fold hypertrophy and more than one affected side remained significantly associated with poorly controlled ingrown toenails. Foot bone deformity was significantly associated with recurrence. These findings could inform patient prognosis and should be communicated to the patients before beginning the treatment.
Introduction
Nail brace application has been used as a noninvasive and effective option for treating ingrown nail,1-5 showing good efficacy for ingrown toenails of both the hallux1,2,4,6 and the lesser toes.7 In a prospective study, up to 95% of patients treated with nail braces showed major improvement, reduced pain and high patient satisfaction.2 However, recurrence rates vary between 7.4% and 28%.2,3,5 Some patients even experience temporal deterioration of the condition during nail brace therapy which makes the disease difficult to control.1,8
In this study, we aimed to investigate the risk factors for poorly controlled and recurrence-prone cases of ingrown toenail treated with nail braces.
Methods
Study population
This retrospective case series included patients with ingrown toenails treated with nail braces at the dermatology clinic at Wan Fang Hospital, Taipei Medical University, between June 1, 2015 and May 31, 2018. The last follow-up day was January 31, 2019. The study was approved by the joint institutional review board of Taipei Medical University.
Treatment protocol
We used the hook-type brace, COMBIped® brace (3TO GmbH, Deisenhofen, Germany), or a combination of COMBIped® and an adhesive device, Podofix® nail braces (3TO GmbH, Deisenhofen, Germany).2 For patients with large granulation tissue, Podofix® or cotton tamponade was initially applied for 2–4 weeks and oral antibiotics were prescribed for one week to wait for granulation tissue resolution, followed by COMBIped® nail brace application. Patients were followed up on a monthly basis during the treatment period. If the nail brace dropped off within the first month, it was reapplied. If the nail brace dropped off after the first month, the need for a second treatment cycle was evaluated by the doctor. Subsequently, the patients were followed up every three months after the dropping-off of the nail brace.
Data collection and definition
We reviewed the clinical records, collated all follow-up photographs of the patients and collected information regarding sex, age, risk factors, involved sides of the toes, the type and grade of ingrown toenail, total length of the treatment period, length of follow-up, poor control and recurrence. We classified the ingrown toenails into two clinical types: Acute inflammed infected-type and chronic dystrophic type ingrown toenails according to our previous studies.1,2 Acute inflamed ingrown toenails were graded using the Heifetz staging.9 The follow-up period referred to the brace-free period between nail brace removal (end of the treatment) and January 31, 2019. Poor control was defined as more than one episode of periungual inflammation or paronychia during the nail brace treatment period. Recurrence was defined as recurrent pain of the toenail during the follow-up period.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 24. For comparisons, one-way analysis of variance and chi-square tests were used for continuous and categorical variables, respectively. Multivariate logistic regression models were used for further adjustment. Probability (P) values < 0.05 indicate statistical significance.
Results
Patient characteristics and outcomes
We reviewed 238 patients with 320 ingrown toenails (411 sides) treated with nail braces. The demographic data of all patients are shown in Table 1. Six patients (11 sides) were either not treated for more than one month or did not attend at least one follow-up. Two hundred thirty two patients (400 sides) were followed until the last follow-up day. Eleven (22 sides) of 232 patients are still receiving treatment to date. Records of treatment duration, follow-up period and recurrence of 221 patients (378 sides) were available [Figure 1]. Mean treatment duration and follow-up period were 161.2 ± 98.3 days and 432.7 ± 320.9 days, respectively. Poor control and recurrence were observed in 7.3% (17/232) and 12.2% (27/221) of the patients, respectively. Regarding treated sides, 6.5% (26/400) and 7.7% (29/378) showed poor control and recurrence, respectively.
| Demographic data | Total (n=238) | CD type (n=120) | AI type (n=118) | P |
|---|---|---|---|---|
| Age (year) | ||||
| <20 | 34 (14.3) | 2 (1.7) | 32 (27.1) | <0.001 |
| 20–65 | 160 (67.2) | 89 (74.2) | 71 (60.2) | |
| >65 | 44 (18.5) | 29 (24.1) | 15 (12.7) | |
| Sex | ||||
| Male | 92 (38.7) | 33 (27.5) | 59 (50.0) | <0.001 |
| Female | 146 (61.3) | 87 (72.5) | 59 (50.0) | |
| Previous trauma | 23 (9.7) | 11 (9.2) | 12 (10.2) | 0.483 |
| Hallux valgus | 24 (10.1) | 14 (11.7) | 10 (8.5) | 0.274 |
| Proximal nail fold hypertrophy | 20 (8.4) | 1 (0.8) | 19 (16.1) | <0.001 |
| Previous nail avulsion | 36 (15.1) | 13 (10.8) | 23 (19.5) | 0.046 |
| Affected sides | 0.003 | |||
| One | 127 (53.4) | 53 (44.2) | 74 (62.7) | |
| More than one | 111 (46.6) | 67 (55.8) | 44 (37.3) | |
| Affected area | n=411 | n=244 | n=167 | |
| Right medial | 129 (31.4) | 79 (32.6) | 50 (29.9) | 0.106 |
| Right lateral | 85 (20.7) | 41 (16.8) | 44 (26.3) | |
| Left medial | 123 (29.9) | 75 (30.7) | 48 (28.7) | |
| Left lateral | 74 (18.0) | 49 (20.1) | 25 (15) | |
| Grade† | ||||
| I | NA | 68 (40.7) | ||
| II | NA | 68 (40.7) | ||
| III | NA | 31 (18.6) | ||
| Treatment duration (days)‡ | 161.2 (98.3) | 188.4 (106.1) | 125.0 (72.8) | <0.001* |
| Follow-up duration (days)‡ | 432.7 (320.9) | 402.0 (319.5) | 482.8 (318.0) | 0.015* |
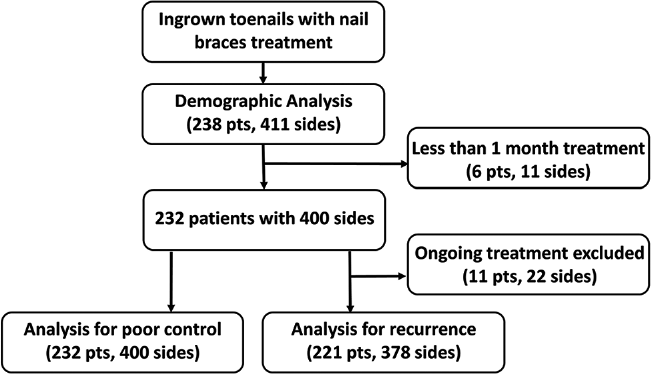
- Flow chart of inclusion and subdivision for analyses
Patients with poorly controlled ingrown toenails
Among the 17 poorly controlled patients, ten patients received cotton tamponades only or with nail brace again. Only one of them could not be cured. Remaining patients received partial nail avulsion with matricectomy. However, recurrence was observed again for two sides, requiring a second nail avulsion surgery.
Data on the comparisons of demographics and potential risk factors between patients with poorly controlled and properly controlled ingrown toenails are shown in Table 2. A higher proportion of younger (<20 years old) and male patients was found in the poorly controlled group. The proportions of patients with a history of trauma, proximal nail fold hypertrophy and previous nail surgery were significantly higher among patients with poorly controlled ingrown toenails. These patients also had a higher occurrence of the acute inflamed ingrown toenails, multiple side involvement and lateral side involvement than the properly controlled patients. After adjustment for sex, type of ingrown toenails, affected sides and other risk factors, the acute inflamed ingrown toenails (OR, 278.4; 95% confidence intervals [CI], 1.7–45027.3), previous nail avulsion (OR, 137.3; 95% CI, 4.0–4685.3), proximal nail fold hypertrophy (OR, 35.1; 95% CI, 5.0–248.0) and more than one affected side (OR, 118.6; 95% CI, 4.2–3342.9) remained significantly associated with poorly controlled ingrown toenails.
| Risk Factors | Recurrence (n=27) | Nonrecurrence (n=194) | P | Poor control (n=17) | Proper control (n=215) | P |
|---|---|---|---|---|---|---|
| Age (year) | ||||||
| <20 | 3 (11.1) | 29 (22.9) | 0.736 | 12 (70.6) | 21 (9.8) | <0.001* |
| 20–65 | 18 (66.7) | 132 (28.6) | 5 (29.4) | 154 (71.6) | ||
| >65 | 6 (22.2) | 33 (37.1) | 0 (0) | 40 (18.6) | ||
| Sex | 14 (23.0) | 4 (11.4) | ||||
| Male | 15 (55.4) | 72 (37.1) | 0.053 | 13 (76.5) | 76 (35.3) | 0.001* |
| Female | 12 (44.6) | 122 (62.9) | 4 (23.5) | 139 (65.7) | ||
| Trauma | 5 (18.5) | 16 (8.2) | 0.094 | 5 (29.4) | 17 (7.9) | 0.014* |
| Hallux valgus | 5 (18.5) | 16 (8.2) | 0.094 | 0 (0) | 22 (10.2) | 0.172 |
| Proximal nail fold hypertrophy | 5 (18.5) | 15 (7.7) | 0.078 | 9 (52.9) | 26 (12.1) | <0.001* |
| Previous nail extraction | 7 (25.9) | 28 (14.4) | 0.109 | 13 (76.5) | 7 (3.3) | <0.001* |
| Type | ||||||
| AI | 14 (12.4) | 99 (87.6) | 0.550 | 16 (14.0) | 98 (86.0) | <0.001* |
| CD | 13 (12) | 95 (88) | 1 (0.8) | 117 (99.2) | ||
| Affected sides | ||||||
| One | 12 (44.4) | 109 (56.2) | 0.173 | 3 (17.6) | 121 (56.3) | 0.002* |
| More than one | 15 (55.6) | 85 (43.8) | 14 (82.4) | 94 (43.7) | ||
| Affected area | n=29 sides | n=349 sides | 0.002* | n=26 sides | n=374 sides | 0.002* |
| Right medial | 8 (27.6) | 110 (31.5) | 5 (19.2) | 121 (32.4) | ||
| Right lateral | 7 (24.1) | 74 (21.2) | 11 (42.3) | 72 (19.3) | ||
| Left medial | 14 (48.3) | 99 (28.4) | 2 (7.7) | 117 (31.3) | ||
| Left lateral | 0 (0) | 66 (18.9) | 8 (30.8) | 64 (17.1) | ||
| Treatment duration (days) | 156.1 (69.8) | 161.7 (100.4) | 0.771 | 175.6 (133.2)† | 160.2 (95.4)† | 0.441 |
| Follow-up duration (days) | 653.2 (311.1) | 418.7 (315.5) | <0.001* | 270.3 (223.3)† | 449.0 (323.8)† | 0.006* |
Patients with recurrent ingrown toenails
Among the 27 patients with recurrent ingrown toenails, nine patients received a new nail brace, Naspan® platinum nail brace (Gerlach GmbH, Germany), for maintenance [Figures 2a-d]; the other patients received another cycle of COMBIped® nail brace therapy. The patients with recurrent ingrown toenails showed different proportions of affected areas in comparison with patients with nonrecurrent ingrown toenails. The patients with recurrent ingrown toenails also had a significantly longer follow-up period [Table 2]. Using a multivariate logistic regression model, hallux valgus [Figure 3] was found to be significantly associated with recurrent ingrown toenails (OR, 3.6; 95% CI, 1.1–11.7).

- A patient with chronic dystrophic ingrown toenails and was treated with COMBIped® nail braces

- The patient was treated for 8 months and the ingrown toenails significantly improved

- One year after removal of COMBIped® nail braces, ingrown toenails recurred and he was then treated with Naspan® nail braces

- After 11-month maintenance therapy, the ingrown toenails also showed improvement

- A patient with severe hallux valgus who has been treated with COMBIped® nail brace but with recurrence one year later
Discussion
In this retrospective study of 238 cases with 411 treated sides, 6.5% of the treated sides were poorly controlled during nail brace application. During the brace-free follow-up period, 7.7% of the treated areas showed recurrence. Acute inflamed ingrown toenails, previous nail avulsion, proximal nail fold hypertrophy and multiple affected sides were shown to be independent risk factors for poor control under treatment. On the other hand, hallux valgus was significantly associated with recurrence after nail brace removal.
Even though the efficacy of nail brace treatment was generally favorable, a small proportion of the patients in this study experienced pain and granulation tissue during the treatment. This poorly controlled status would appear as a continuous or fluctuating inflammation. Liu et al. reported three patients with acute inflamed ingrown toenails experiencing deterioration with pyogenic granuloma due to wire irritation after brace initiation.1 However, poor control at the beginning of the treatment did not necessarily lead to poor treatment outcome. During the initial poorly controlled status, measures such as temporal removal of the hook-type brace, partial distal nail removal, cotton tamponade use and adhesive-type nail brace use could still eventually lead to good treatment responses and cure of the ingrown nails.1,8
In this study, patients with a poorly controlled status during brace therapy were more likely to be younger. Younger males were probably more likely to be active in sports activities.10-12 A history of matricectomy was reported to be an independent risk factor for recurrence after nail brace treatment.13 However, in our study, a history of nail surgery was a significant risk factor for poor control, but not for recurrence after nail brace therapy. Poor control could be due to the lifted nail plate adding further irritation to the already vulnerable, inflamed nail folds. Proximal nail fold hypertrophy was an important novel observation in patients with poorly controlled disease. The nail brace could rapidly and forcefully lift up the nail plate which would further pierce the already prominent, pushable, proximal nail fold. Nail brace application for patients with the aforementioned risk factors could require a longer treatment period to lead to improvement.
During the follow-up brace-free period of 432.7 ± 320.9 days, 12.2% of the patients experienced recurrence after nail brace removal. Our follow-up period was sufficiently long to enable relevant risk factor analysis. In the multivariate analysis, hallux valgus was significantly associated with recurrent cases of ingrown toenails. Cho et al. reported a higher prevalence of valgus deformities (64.3%) in the ingrown nail population.14 The presence of a hallux interphalangeal angle greater than or equal to 14.5° has also been reported as a predisposing factor for developing ingrown hallux nail, indicating that bone misalignment could provoke the development of ingrown nail.15 Therefore, dermatologists should consider not only treating ingrown nails but also correcting associated bone deformities, especially when managing recurrent cases.
Limitations
The main limitation was a retrospective design so that confounding factors such as comorbidities, body mass index, accompanying nail changes and lifestyle could not be evaluated. Further prospective studies and clinical trials are required to determine whether the focus on reducing the risk factors or the proposed treatment algorithm could optimize intervention outcomes for ingrown nails.
Conclusion
In conclusion, by knowing these potential risk factors of poor control and recurrence of nail brace treatment, patients could know the prognosis and therefore benefit from more suitable treatment plans with reasonable expectation.
Acknowledgments
The authors thank the Taipei Medical University for financial support under grant no. TMU108-AE1-B11 which made this study possible.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Taipei Medical University grant no. TMU108-AE1-B11.
Conflicts of interest
There are no conflicts of interest.
References
- Efficacy of a new nail brace for the treatment of ingrown toenails. J Dtsch Dermatol Ges. 2018;16:417-23.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of nail braces for acute and chronic ingrown toenails: A prospective study. Dermatol Surg. 2020;46:258-66.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of nail brace application in diabetic patients with ingrown nails. Dermatol Surg. 2008;34:84-6.
- [CrossRef] [Google Scholar]
- Nail braces as an alternative treatment for ingrown toenails: results from a comparison with the Winograd Technique. J Foot Ankle Surg. 2015;54:620-4.
- [CrossRef] [PubMed] [Google Scholar]
- Nail brace application: A noninvasive treatment for ingrown nails in pediatric patients. Dermatol Surg. 2019;45:323-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of symptomatic incurved toenail with a new device. Foot Ankle Int. 2009;30:1083-7.
- [CrossRef] [PubMed] [Google Scholar]
- A new one-sided nail brace for ingrown toenails of lesser toes. J Am Acad Dermatol. 2019;81:1024-5.
- [CrossRef] [Google Scholar]
- Combination of two types of nail brace for the treatment of complicated ingrown toenails. Indian J Dermatol Venereol Leprol. 2017;83:722-5.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and sociodemographic characteristics of patients with ingrown nails. J Am Podiatr Med Assoc. 2019;109:201-6.
- [CrossRef] [Google Scholar]
- Clinical and sociodemographic characteristics of ingrown nails in children. J Am Podiatr Med Assoc. 2019;109:272-6.
- [CrossRef] [PubMed] [Google Scholar]
- Relation between nail consistency and incidence of ingrown toenails in young male runners. J Am Podiatr Med Assoc. 2017;107:137-43.
- [CrossRef] [PubMed] [Google Scholar]
- Previous nail surgery is a risk factor for recurrence of ingrown nails. Dermatol Surg. 2014;40:1152-4.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and bone-related comorbidities of ingrown nail: A nationwide population-based study. J Dermatol. 2018;45:1418-24.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between the presence of abnormal hallux interphalangeal angle and risk of ingrown hallux nail: A case control study. BMC Musculoskelet Disord. 2015;16:301.
- [CrossRef] [PubMed] [Google Scholar]






