Translate this page into:
An expanding annular plaque on the leg
Corresponding author: Alejandro García-Vázquez, Department of Dermatology, Clinical University Hospital of Valencia, University of Valencia, Spain. alejandrogv92@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: García-Vázquez A, Guillen-Climent S, Pons Benavent M, Porcar Saura S, Ramón-Quiles MD. An expanding annular plaque on the leg. Indian J Dermatol Venereol Leprol 2023;89:280-2.
A man in his 30s presented with a centrifugally expanding lesion on the anterolateral aspect of his right leg for the past three months. It started as a small papule which progressed to form a circinate plaque of raised erythematous edges with normal skin of a brown-yellow hue in the center [Figure 1]. The edges were firm, infiltrated and slightly painful on palpation. The patient denied previous bug bites or the introduction of new medications. He had no systemic symptoms.

- Annular plaque on the leg with raised erythematous edges and yellowish coloration in the center
A biopsy from the erythematous edge of the lesion was taken, showing a lymphohistiocytic inflammatory infiltrate in the subcutaneous tissue with mainly septal involvement, granuloma formation and fibrous septal thickening. The dermis showed mild non-specific changes and there were no vasculitis or collagen abnormalities [Figures 2-5].
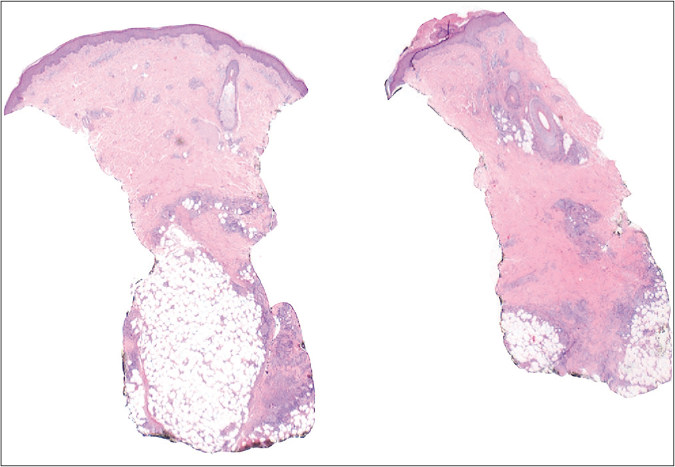
- Inflammatory infiltrate mainly affecting the subcutaneous tissue (hematoxylin-eosin, ×10 )
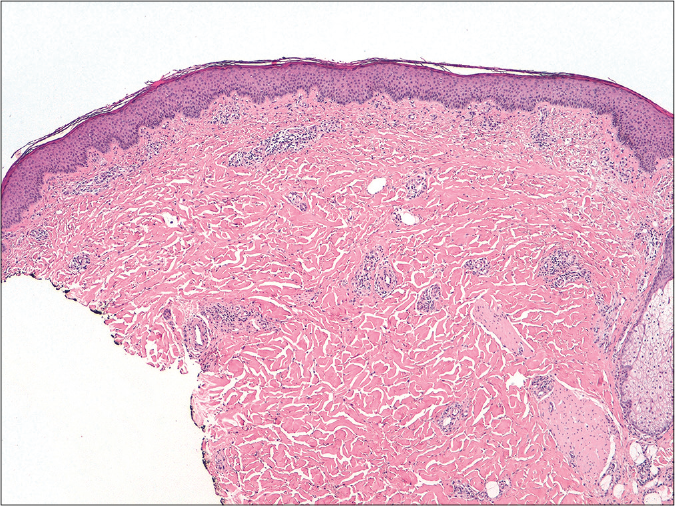
- Mild perivascular inflammatory infiltrate, without significant epidermal alterations, collagen degeneration or palisade granulomas that could suggest necrobiosis lipoidica (hematoxylin-eosin, ×40 )
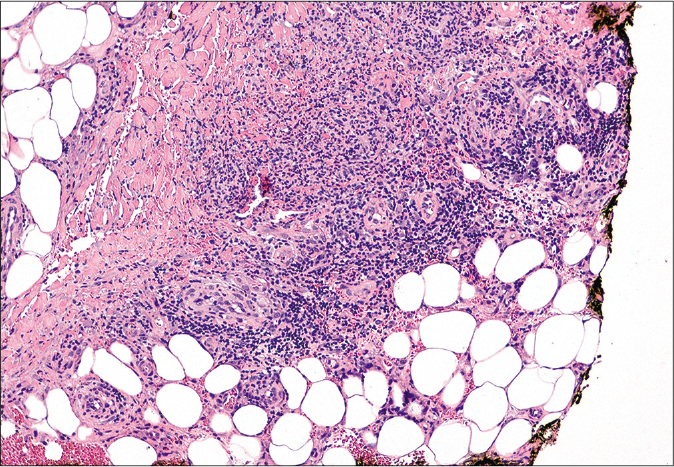
- Lymphohistiocytic inflammatory infiltrate in the subcutaneous tissue, affecting mainly the septa with fibrous thickening and granuloma formation. There was no vasculitis (hematoxylin-eosin, ×100)
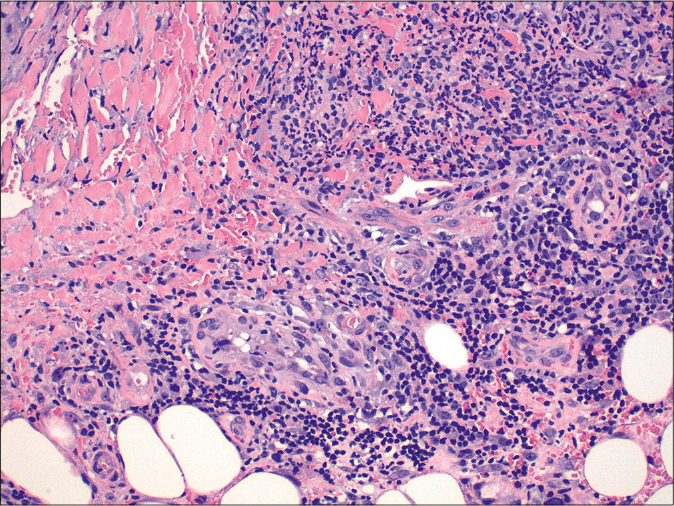
- Lymphohistiocytic infiltrate with granulomas (hematoxylin-eosin, ×200)
Question
What is your diagnosis?
Answer
Erythema nodosum migrans
Discussion
Along with the clinical picture, the histology was compatible with the diagnosis of erythema nodosum migrans. Blood tests, including complete blood count, antistreptolysin O titers, angiotensin-converting enzyme levels, Borrelia burgdorferi serologies and interferon-gamma release assays, were all normal. The X-ray of the chest was also unremarkable. Treatment with oral indomethacin 25 mg twice a day was initiated, in addition to bed rest during the initial days, obtaining complete resolution of the lesion in two months.
Erythema nodosum is the most frequent form of panniculitis. It is considered an unspecific reactive secondary process to a wide variety of stimuli such as infections, rheumatologic and autoimmune diseases or malignancies. It usually appears as erythematous firm nodules and plaques on the extensor area of both the lower extremities with a tendency to spontaneous resolution without ulceration, scarring or atrophy.1
Erythema nodosum migrans, also known as subacute nodular migratory panniculitis or Vilanova disease, is a rare clinical variant of erythema nodosum. The differences from classic erythema nodosum are mostly clinical. Erythema nodosum migrans is described predominantly in women, as localized nodular lesions on the leg that progress by confluence or centrifugal extension, forming annular plaques with central clearing.2 The edges are erythematous, whereas the center may have a yellowish hue.1,2 Lesions are usually unilateral, single or few in number, relatively painless and associated with few systemic symptoms. While lesions in classic erythema nodosum heal spontaneously within three–four weeks in most cases,1 in erythema nodosum migrans, they tend to last from months to years if left untreated.1-5 Furthermore, erythema nodosum migrans may not respond to conventional drugs for erythema nodosum.5 A correct differentiation between both entities is, therefore, important, as it may affect both the prognosis and the choice of treatment. Although an underlying etiology cannot normally be identified, triggers similar to those in classic erythema nodosum have been described2,3 and should be investigated for.
Histologically, erythema nodosum migrans may be indistinguishable from classic erythema nodosum, showing an inflammatory infiltrate in the septa with no vasculitis.1However, erythema nodosum migrans tends to show greater septal thickening and prominent granulomatous inflammation, along with the absence of phlebitis or hemorrhage.2-5
The main differences between classic erythema nodosum and erythema nodosum migrans are summarized in Table 1.
| Classic erythema nodosum | Erythema nodosum migrans | |
|---|---|---|
| More frequent in women between their second and fourth decade of life1 | More frequent in women between 15 and 65 years2,3 | |
| Multiple erythematous nodules1 | One or few erythematous nodules or plaques1,2,3,5 | |
| Clinical features | Symmetric, bilateral distribution1,3 | Asymmetric, unilateral distribution1,2,3,5 |
| Anterior aspects of both legs1 | Lateral side of one leg1,5 | |
| Lesions are tender or painful1 | Lesions are less tender or painless1,2,3,5 | |
| Usually associated with fever, fatigue, arthralgia and other systemic syptoms1 | Few or no systemic symptoms2,5 | |
| Evolution and prognosis | Lesions turn purplish and resolve like a deep bruise1 | Lesions spread centrifugally in an annular shape with a yellowish center1,2,3,5 |
| Tend to spontaneous resolution within 3–4 weeks without atrophy of scarring1,3 | Persistent, lasts months or years without treatment2-5 | |
| Etiology | Idiopathic, infections, drugs, autoimmune diseases, malignancy, pregnancy1,3 | Idiopathic, infections, drugs, autoimmune diseases, malignancy, pregnancy2,3,5 |
| Histological features | Septal panniculitis with no vasculitis, superficial and deep perivascular inflammatory lymphocytic infiltrate in the dermis1,3 | Septal panniculitis with greater septal thickening and a prominent granulomatous inflammation of subcutaneous septa1-5 |
| Treatment options | Bed rest, potassium iodide, NSAIDs, intralesional corticosteroids, heparinoid ointment, colchicine, hydroxychloroquine, dapsone1,5 | Bed rest, potassium iodide, NSAIDs (indomethacin), intralesional corticosteroids, topical heparin, topical corticosteroids, hydroxychloroquine, dapsone2,3,5 |
NSAIDs: Nonsteroidal anti-inflammatory drugs
The differential diagnoses include other chronic annular dermatoses, such as erythema migrans or necrobiosis lipoidica. The biopsy is usually sufficient to establish the diagnosis.
Treatment includes management of underlying conditions if they exist, bed rest and compression stockings. Potassium iodide is described as a first-line drug, although intralesional corticosteroids and oral indomethacin can be considered as valid alternatives.2,3,5 Other options include naproxen, dapsone, hydroxychloroquine, clobetasol propionate cream or even topical heparin5 which have given variable results.
Conclusion
Erythema nodosum migrans represents an infrequent form of panniculitis with histologic findings that can be identical to those of classic erythema nodosum, but with a particular clinical presentation. Its recognition is important, given its long course without adequate treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Erythema nodosum migrans successfully treated with indomethacin: A rare entity. Adv Biomed Res. 2014;3:264.
- [CrossRef] [Google Scholar]
- An unusual presentation of Vilanova disease (erythema nodosum migrans) with superficial histologic changes. JAAD Case Rep. 2016;2:41-3.
- [CrossRef] [Google Scholar]
- Septal granulomatous panniculitis: Comparison of the pathology of erythema nodosum migrans (migratory panniculitis) and chronic erythema nodosum. J Am Acad Dermatol. 1990;22:477-83.
- [CrossRef] [Google Scholar]
- Exploring the combination of SSKI and topical heparin in a case of erythema nodosum migrans. Dermatol Ther. 2018;31:e12610.
- [CrossRef] [Google Scholar]





