Translate this page into:
Varicella gangrenosa: A rare chickenpox complication
Corresponding author: Dr. Sobhanakumari Kunjumani, Department of Dermatology, Government T. D. Medical College, Vandanam, lappuzha - 688 005, Kerala, India. drsobhanakumarik@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohan A, Suresh A, Sudhesan A, Kunjumani S, Celine MI. Varicella gangrenosum: A rare chickenpox complication. Indian J Dermatol Venereol Leprol 2022;88:771-3.
Abstract
Varicella gangrenosa is a rare but life-threatening dermatological complication of infection with varicella-zoster virus. A healthy 37-year-old male who had been diagnosed with varicella 20 days back was admitted to our hospital with complaints of fever and painful necrotic skin lesions. Physical examination revealed multiple round to oval ulcers covered with eschar predominantly over arms, lower limbs, back of trunk and flanks. Streptococcus pyogenes and Staphylococcus aureus grew in wound culture. Biopsy revealed ulceration and necrosis of epidermis, and edema, hemorrhage and granulation tissue formation involving the dermis and subcutaneous tissue. The patient was treated with acyclovir - parenteral followed by oral, antibiotics and supportive measures. The lesions healed and he was discharged after 20 days. We report this case to draw attention to the fact that varicella gangrenosum, even though a rare complication, may occur in the lesions of chicken pox and that the survival of patient depends on early diagnosis and aggressive treatment.
Keywords
Acyclovir
moist gangrene
streptococcus pyogenes
varicella
Introduction
Chickenpox is a very common disease due to primary infection with varicella-zoster virus characterized by vesicles on the skin and mucosa associated with fever, malaise, backache and headache. Varicella usually runs a benign course. But rarely, life-threatening complications like pneumonia, sepsis, osteomyelitis, myocarditis and encephalitis may occur. Hospitalization rates for varicella are about 3–6 per 1,000 cases, and the complication rate ranges between 2% and 4%.1 One of the dermatological complications is bacterial superinfection, sometimes leading to varicella gangrenosa. It is a type of necrotizing fasciitis which is a rare but life-threatening dermatological complication with a frequency of 0.05%–0.16%.2
We are reporting the case of a healthy 37-year-old male who presented with varicella and moderately severe lesions of moist gangrene.
Case Report
A 37-year-old healthy manual laborer was referred to our hospital, Government T. D. Medical College, Alappuzha, Kerala, with fever and painful necrotic skin lesions. He gave history of constitutional symptoms and generalized vesicular lesions which appeared 20 days back. His mother and brother had chicken pox 2 weeks prior to the onset of his symptoms. Four days after the development of lesions, he consulted a doctor in a nearby hospital and took acyclovir 800 mg orally thrice daily for 5 days. Within 1 week, the lesions on face, forearms and upper trunk healed, but rest of the lesions coalesced and ruptured to form painful ulcers with purulent slough which enlarged and became necrotic over these days.
On examination, he appeared ill and mildly irritable; his temperature was 39.5°C with tachycardia (pulse rate-110/ min), blood pressure was 100/60 mmHg and he had bilateral pitting pedal edema. He was admitted in medical intensive care unit. Dermatological examination revealed multiple round to oval ulcers of size ranging from 1 × 2 cm to 10 × 7 cm, covered with eschar, present predominantly on the upper arms, flexural and extensor aspect of both lower limbs, back of trunk and flank region [Figures 1]. Several healed scars of chickenpox were present on the face, upper trunk and extremities. No mucosal lesions were noted. Systemic examination including central nervous system did not reveal any abnormality. Routine lab investigations revealed anemia (hemoglobin-9.8g%), neutrophilic leukocytosis (66.1 × 109/L with 92.1% neutrophils) and elevated erythrocyte sedimentation rate (80 mm/1st hour). Platelet count was 364 × 109/L and C-reactive protein level was 64 mg/L. Liver function tests showed elevated liver enzymes (SGOT, SGPT and alkaline phosphatase 166, 421 and 510 IU/L respectively). Routine urine examination, renal function tests, random blood sugar, coagulation studies and ultrasound of the abdomen were normal. Pus culture from the ulcer yielded mixed bacterial growth mainly Streptococcus pyogenes and Staphylococcus aureus. Blood culture was sterile. HBsAg, anti-HCV and HIV serology were negative and there was no evidence of immunodeficiency.

- Lesions at the time of admission
With the provisional diagnosis of varicella gangrenosa, the patient was given intravenous piperacillin and tazobactam for 5 days. Acyclovir 10 mg/kg was administered intravenously every eighth hour initially for 10 days and later changed to oral acyclovir 800 mg five times daily for 5 days. Cefotaxime and cloxacillin were administered for 10 days as per pus culture and sensitivity. Mechanical debridement of the ulcers was also done. Biopsy from the ulcer margin revealed focal ulceration and necrosis of epidermis, and edema, hemorrhage and granulation tissue formation involving the whole of dermis up to subcutaneous tissue [Figure 2]. His condition gradually improved, skin lesions healed entirely and he was discharged after 20 days of hospitalization [Figures 3 and 4]. Based on the history, clinical features and investigations, the diagnosis of varicella gangrenosa (moist gangrene type) was confirmed.
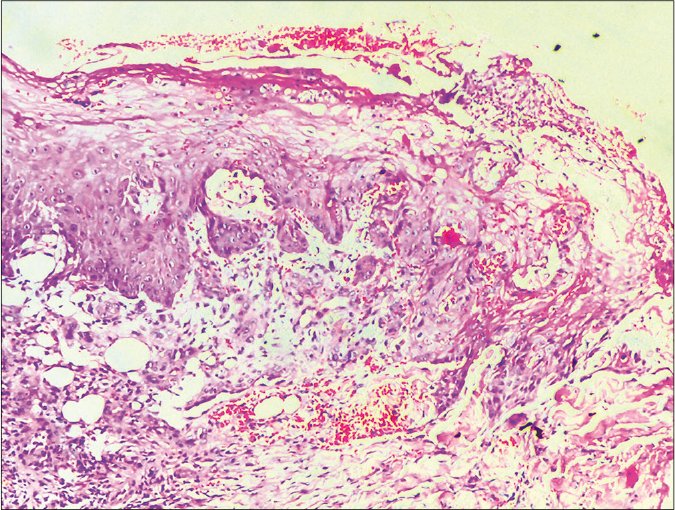
- Histopathology section from the ulcer margin (H and E, ×200) showing focal ulceration and necrosis of epidermis, and edema, hemorrhage and granulation tissue formation involving the whole of dermis up to subcutaneous tissue

- Lesions after 15 days of admission

- Lesions at discharge of the patient
Discussion
The term “varicella gangrenosa” was first coined and described by Jonathan Hutchinson in 1881.3 Very few cases have been reported in the literature till now.4 The types of varicella gangrenosa described in literature are: (a) moist gangrene, the prototype of varicella gangrenosa, is thought to be infective, most often caused by group A β-hemolytic Streptococcus or Staphylococcus aureus; (b) dry gangrene, secondary to arterial thrombosis; and (c) purpura fulminans, associated with disseminated intravascular coagulation.5
Varicella gangrenosa should be suspected in any patient with a history of varicella infection who develop pain out of proportion to physical findings, swelling in an extremity or other body area and gangrenous ulceration along with constitutional symptoms. It usually occurs between the fourth and seventh days following the onset of chickenpox.4 The rash is initially erythematous, turns blue within 24 to 48 h and eventually becomes necrotic. It is postulated that the rapidly multiplying varicella virus disrupts the epidermal integrity, allowing bacterial superinfection due to Streptococcus pyogenes or rarely, Staphylococcus aureus.4
The full-thickness dermal lesion created by the vesicle provides a route for entry and spread for bacteria to the subcutaneous tissue.6 The M surface protein in group A β-hemolytic Streptococci repels macrophages and complement factors. The pyogenic exotoxins A, B and C produced by group A β-hemolytic Streptococcus stimulate the release of tumor necrosis factor-α (TNF-α) and interleukin-1(IL-1), which in turn causes fever, rash, direct toxic effects to the endothelium, T-cell activation and eventually, septic shock. The bacteria also secrete hyaluronidase and streptolysin which lead to tissue invasion and damage. Therefore, it is necessary to remove the necrotic tissue which is the source of exotoxins that may cause circulatory collapse, multiple organ failure and eventually lead to death.7
Our patient presented with moderately severe lesions of moist gangrene. Since the patient was not immunodeficient, this may be due to inadequate dosage of the antiviral drugs initially administered, and improper hygiene. He was treated successfully with parenteral antibiotics and antiviral therapy, initiated from the day of admission along with close monitoring of clinical signs, fluid resuscitation, adequate nutrition and debridement. Based on available reports, initiation of acyclovir within 24 h after the onset of rash has shown to reduce morbidity and mortality.8 The latest WHO guidelines proppose the use of intravenous acyclovir in patients with varicella who are immunocompromised or have severe complications.9 In such cases, intravenous acyclovir followed by oral antivirals should be the treatment regime followed.10
Thus, early and prolonged administration of acyclovir is the cornerstone in the management of varicella gangrenosa. Also, systemic antibiotics with good streptococcal and staphylococcal coverage should be instituted initially itself in such patients to accelerate cutaneous healing and to avoid more severe complications. In addition, strict asepsis should be maintained and debridement should be undertaken to remove all infective foci. Survival is dependent on early diagnosis and adequate aggressive treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A global perspective of the epidemiology and burden of varicella zoster virus. Curr Pediatr Rev. 2009;5:207-28.
- [CrossRef] [Google Scholar]
- Periorbital varicella gangrenosa necessitating orbital exenteration in a previously healthy adult. South Med J. 1996;89:723-5.
- [CrossRef] [Google Scholar]
- Picture of the month. Varicella gangrenosum. Am J Dis Child. 1985;139:1151-2.
- [CrossRef] [Google Scholar]
- A case control study of necrotizing fasciitis during primary varicella. Pediatrics. 1999;103:783-90.
- [CrossRef] [Google Scholar]
- Necrotizing fasciitis versus pyoderma gangrenosum: Securing the correct diagnosis! A case report and literature review. Eplasty. 2011;11:e24.
- [Google Scholar]
- The use of oral acyclovir in otherwise healthy children with varicella. Pediatrics. 1993;91:674-6.
- [Google Scholar]
- Acyclovir for treating varicella in otherwise healthy children and adolescents. Cochrane Database Syst Rev. 2005;4:CD002980.
- [CrossRef] [Google Scholar]
- Harrison's Principles of Internal Medicine (19th ed). New York: The McGraw Hill Companies. Inc.; 2015. p. :1088.
- [Google Scholar]






