Translate this page into:
A persistent crusted erythematous plaque on the forearm
Corresponding author: Dr. Maira E. Herz-Ruelas, Department of Dermatology, Universidad Autónoma de Nuevo León, Hospital Universitario ‘Dr. José Eleuterio González,’ Monterrey, Nuevo León, México. mairaherz@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Figueroa-Morales AL, Kubelis-López DE, Pérez-Garza DM, Rodríguez-Tamez G, Vázquez-Martínez OT, Ocampo-Candiani J, et al. A persistent crusted erythematous plaque on the forearm. Indian J Dermatol Venereol Leprol 2023;89:277-9.
An 85-year-old female, resident of northeast Mexico, presented with a seven-month history of an itchy, progressively growing, crusted plaque with purulent discharge and focal ulceration on her right forearm [Figure 1]. History of fever, chills, respiratory or other systemic symptoms were denied. Further questioning revealed that she performed gardening as a leisure-time activity. A skin biopsy was taken for histopathological examination and culture [Figures 2 and 3].
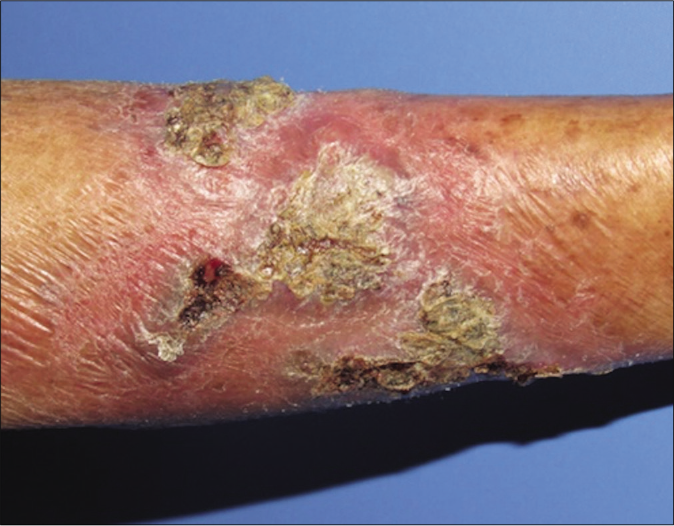
- Erythematous plaque with overlying haematic and yellow crusts, before treatment
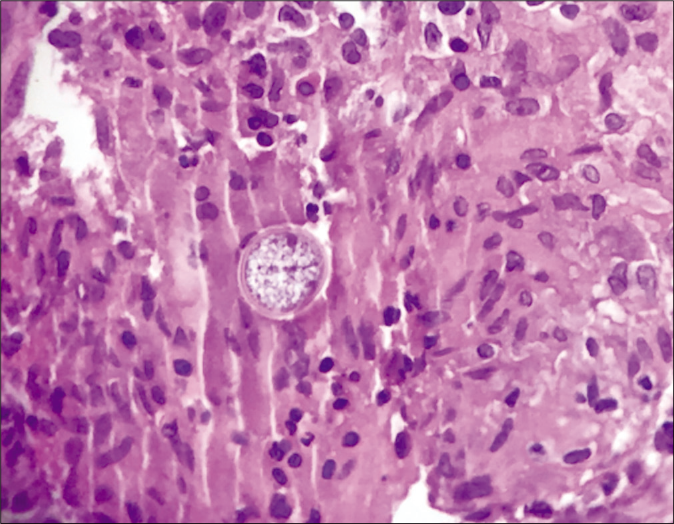
- Histopathology showing a spherule (H&E ×100)

- Direct KOH of the skin biopsy showing spherules
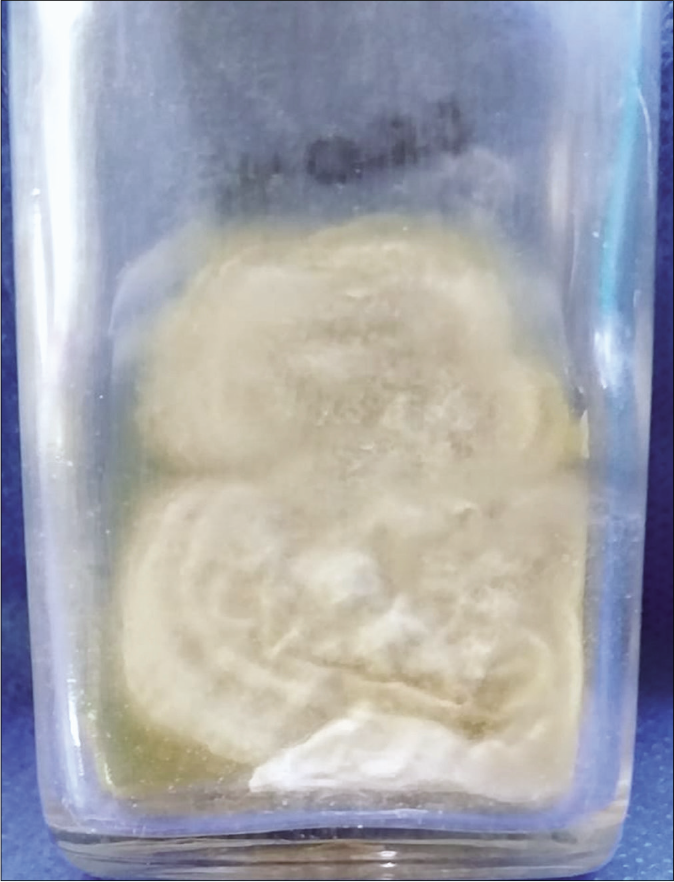
- Fungal culture in Sabouraud agar exhibiting a white colony
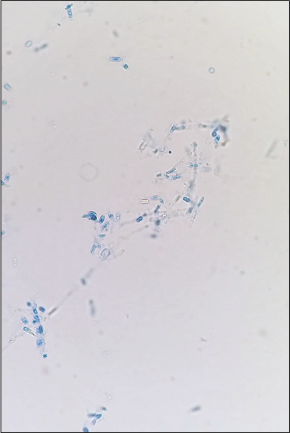
- Direct KOH of the culture visualising barrel-shaped arthroconidia and septate hyphae
Question
What is the diagnosis?
Diagnosis
Primary cutaneous coccidioidomycosis.
Investigations and Follow-up
The histopathology revealed necrotising granulomatous inflammation with endospore-containing spherules [Figure 2]. Direct KOH of the skin biopsy showed spherules [Figure 3]. Fungal skin culture developed a white colony [Figure 3]. Direct KOH examination of the culture showed septate hyphae and barrel-shaped arthroconidia [Figure 3]. Blood tests were unremarkable, except for anaemia. Chest radiograph was normal. A diagnosis of primary cutaneous coccidioidomycosis was made. Treatment was started with oral itraconazole 200 mg twice daily for six months. The lesion completely resolved with scarring and post-inflammatory hyperpigmentation [Figure 4].

- Scarring and post-inflammatory hyperpigmentation after six months of treatment
Discussion
Coccidioidomycosis is a subcutaneous mycosis caused by a dimorphic, soil-dwelling fungus of two different species, Coccidioides immitis or Coccidioides posadasii. Southwest USA, Northern Mexico and some countries in Central and South America are considered endemic areas for this infection.1 Cutaneous coccidioidomycosis can be seen in three different scenarios: In acute pulmonary infection as an acute pulmonary exanthema, in disseminated infection with secondary skin involvement or as a primary cutaneous infection.2 Primary cutaneous coccidioidomycosis is an extremely rare condition with less than 85 cases reported in literature.3 It is caused by direct inoculation into the skin, as a consequence of an abrasion or injury by an external source containing the infectious arthroconidia. Cutaneous coccidioidomycosis is a great mimicker because of the wide variety of clinical presentations. It typically manifests as a painless plaque or nodule with ulceration on an extremity. Other presentations are papules, verrucous plaques, erythematous plaques surrounded by pustules, sporotrichoid nodules and scars, chancriform lesions and fistulising abscesses.1,3 The differential diagnosis ranges from fungal infections (histoplasmosis, blastomycosis, sporotrichosis and chromoblastomycosis), mycobacterial infections (tuberculosis and atypical mycobacteria) and sarcoidosis to malignancy (squamous cell carcinoma, basal cell carcinoma and cutaneous lymphoma).1,3 In the present case, our differentials were fungal infections and squamous cell carcinoma. Diagnostic methods may include culture, microscopy, serology, polymerase chain reaction, intradermal skin test and skin biopsy. Culture is the gold standard for diagnosis. Some of the media used for culture are the brain heart infusion agar, potato dextrose agar, Sabouraud dextrose agar, blood agar and chocolate agar. A white cottony mould grows after two–three weeks of incubation at room temperature.1,2 Direct microscopic examination with potassium hydroxide or Calcofluor shows the presence of double-walled refractile spherules, septate hyphae and barrel-shaped arthroconidia.1,2 Serologic tests to detect IgM and IgG anticoccidioidal antibodies have an 98.5% specificity and a 95.5% sensitivity for diagnosis.3 In the skin biopsy, the histopathology shows the presence of double-walled spherules with endospores. The spherules can be detected with ordinary stains such as haematoxylin and eosin or with special stains such as periodic acid-Schiff, Gridley and Grocott-Gomori’s methenamine silver stains.1,2
During workup, it is essential to perform a complete history and physical examination with emphasis in pulmonary symptoms to exclude disseminated disease; a chest radiograph or CT scan may be appropriate as well.3 In a limited setting where culture or serologic studies are not available, the diagnosis of primary cutaneous coccidioidomycosis could be stabilised with the clinical history, physical examination, histopathological findings (spherules and endospores) and a normal chest X-ray.3,4
The first-line therapy currently recommended for soft-tissue coccidioidomycosis without bone involvement is oral fluconazole 400–800 mg/day or oral itraconazole 200 mg twice daily. Amphotericin B is recommended in case of azole failure. Regardless of the treatment chosen, the duration of therapy is six to twelve months, because of the high relapse rates.5 Coccidioidomycosis is a great mimicker and skin lesions could a wide variety of presentations. Identification of risk factors such as travel to endemic areas or activities related to fungal exposure is important along with biopsy and cultures for an accurate diagnosis. Moreover, systemic involvement must be always ruled out, as it would change the diagnosis and treatment.3
Declaration of patient consent
The patient's consent is not required as the patient's identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Coccidioidomycosis and the skin: A comprehensive review. An Bras Dermatol. 2015;90:610-9.
- [CrossRef] [PubMed] [Google Scholar]
- Primary cutaneous coccidioidomycosis: An update. Am J Clin Dermatol. 2020;21:681-96.
- [CrossRef] [PubMed] [Google Scholar]
- Primary and disseminated cutaneous coccidioidomycosis: Clinical aspects and diagnosis. Curr Fungal Infect Rep. 2016;10:132-9.
- [CrossRef] [Google Scholar]
- 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016;63:e112-46.
- [CrossRef] [PubMed] [Google Scholar]





