Translate this page into:
Current situation of leprosy in tribal areas of India in the post-elimination era
Corresponding author: Dr. Pushpendra Singh, ICMR-National Institute of Research in Tribal Health, Jabalpur, Madhya Pradesh, India. pushpendra.s@icmr.gov.in
-
Received: ,
Accepted: ,
How to cite this article: Sharma M, Dwivedi P, Singh P. Current situation of leprosy in tribal areas of India in the post-elimination era. Indian J Dermatol Venereol Leprol 2022;88:450-1.
Leprosy prevalence has reduced in the past decade and most states in India have achieved the prevalence of less than 1/10,000 (the defining feature of ‘elimination of a disease as a public health problem’). However, a substantial reduction in leprosy burden has not been observed since then.1 The prevalence rate of leprosy across different population subgroups provides an understanding of the transmission patterns and is also a measure of the influence and efficacy of current public health initiatives.2 Post-2005, very few studies have determined the prevalence of leprosy in tribal regions and very little is known about the prevalence of leprosy in the tribal (Adivasi) region of India. Accounting for 8.6% or 104 million people of India’s population (census 2011), adivasis (literal meaning adi = Indigenous; vasi = inhabitant) or tribals are still considered to be highly marginalised and discriminated.3
An independent report has analysed the government statistics and revealed that the rate of decline of leprosy cases in tribal population is much lower than the non-tribal population. From 13.3% in 2009, the proportion of new leprosy patients belonging to the adivasi group has increased to an alarming 18.8% in 2017.4 This trend suggests that leprosy would quickly become more of a disease of the marginalised population living in remote areas. Similarly, by comparing the prevalence of leprosy in tribal versus non-tribal areas, Katkar et al. recommended that even a single new case with Grade 2 disability/new case of child leprosy/female cases should be considered as an evidence of hidden endemicity of leprosy in tribal belt.5 Recognising the need for a roadmap for tribal health which is based on the understanding of the health situation of tribal people, India’s first comprehensive tribal health report was presented before public in 2018. The report is the result of years of research by an expert committee that explored how tribal communities in India are suffering from healthcare inequity and how to bridge that gap.6 The proportion of tribals in the total population of India is only 8.6%. However, the proportion of new leprosy cases among the tribal population was found to be 18.5%, ‘revealing a disproportionate burden of leprosy among the tribal population.’6
Together, the report suggested that in states such as Odisha, Madhya Pradesh, Maharashtra, West Bengal and Jharkhand, nearly half of the new cases of leprosy belonged to the tribal and/or dalit communities.7 In addition, statistical figures from Gujarat suggest that 64.8% of leprosy patients in the state belong to scheduled tribes, while the proportion of scheduled tribe population in the state is a mere 14.8%.3 These figures highlight a disproportionate distribution of leprosy among the tribals, who represent deprived and remotely located population where accessibility to healthcare facilities need to be improved. Similarly, tribals of Madhya Pradesh represent only 21% of the total population of the state but account for 39.4% of the new leprosy cases in the state. Maharashtra, with tribal population under 10%, reported 33.7% of all new community cases of leprosy among them. Tribals in West Bengal record 20.3% of all new leprosy cases while they only account for 5.8% of the state’s total population. In Tripura and Dadra and Nagar Haveli, tribals constitute 31.8% and 52% of the total population, but record 64.7% and 98.2% of the new leprosy cases, respectively.4 These observations and facts clearly corroborate the disproportionate burden of leprosy cases among tribals. It also reveals that a substantial reduction in leprosy cases among tribals has remained elusive despite much acclaimed success in other sections of the society [Figure 1]. The situation persists most likely due to poor health access and awareness among the tribal population which negatively impacts their health-seeking behaviour at an early stage, thereby allowing transmission to continue.8 It is, therefore, important to devise ways to properly counsel and follow up the patients during and after the treatment.
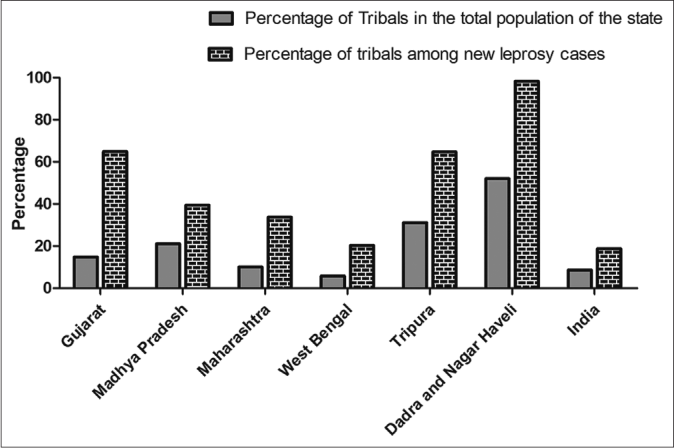
- Proportion of tribals (adivasis) among new leprosy cases in 2017 (4): The most affected states that is, Gujarat, Madhya Pradesh, Maharashtra, Tripura, West Bengal and Union territory Dadra and Nagar Haveli have reported a disproportionately higher number of new leprosy cases among tribals when compared to their proportion in overall population of the state. Last bar is showing a similar trend at the national level.
If the aim of zero leprosy is to be achieved, it is of paramount importance that the leprosy situation in tribal population is addressed with appropriate measures customised to suit the ground realities of the lives of tribal people. Mobile units with necessary clinical expertise need to be deployed in the pockets of endemicity.
Scientists have systematically used molecular epidemiological methods to help explain the nature of primary and secondary drug resistance in different populations across the world. However, despite the knowledge of high burden of leprosy in tribal areas, such surveillance activities have not been performed in these neglected groups of people. Semi-skilled tribal people undertake short-term migrations to adjoining districts and states for working as a labourer at the time of crop harvest. This compromises their treatment adherence, thereby increasing the chances of drug resistance. Further, it can potentially contribute to transmission of drug-resistant strains in other communities in different locations as well. Hence, extra efforts need to be deployed for control of leprosy in tribal population because control of infectious diseases in these population has broader health benefits for non-tribal communities also. This extra effort can have far-reaching and long-term implication for the leprosy control activities in India. Accurate and timely detection of leprosy in these underprivileged communities is an important step for achieving the goal of leprosy eradication in the near future. Strong support for patient supervision and follow-up must be conducted from the outset to ensure treatment compliance. Participation of local people such as traditional healers and the previously treated leprosy patients as the ‘agents of change’ can be very helpful. Increased awareness among the tribal population about the signs and symptoms of the disease is important for achieving the target of ‘leprosy-free India.’
Financial support and sponsorship
The authors are grateful to ICMR and DBT: MS, PD and PS are the recipients of ICMR-RA, SRF and DBT Ramalingaswami fellowships, respectively.
Conflicts of interest
There are no conflicts of interest.
References
- Current situation of leprosy in India and its future implications. Indian Dermatol Online J. 2018;9:83.
- [CrossRef] [PubMed] [Google Scholar]
- Leprosy-a raging persistent enigma. J Family Med Prim Care. 2019;8:1863-6.
- [CrossRef] [PubMed] [Google Scholar]
- Health of tribal populations in India: How long can we afford to neglect? Indian J Med Res. 2019;149:313-6.
- [CrossRef] [PubMed] [Google Scholar]
- Leprosy and Inequities in India's Healthcare: Beyond the Persistent Rhetoric of 'Elimination' Vol 184. New Delhi: Observer Research Foundation; 2019.
- [Google Scholar]
- Epidemiological perspective of national leprosy eradication programme in Maharashtra: Focusing on “tribal hot-spot” of tribal district. Indian J Community Med. 2017;42:174-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tribal Health in India: Bridging the Gap and the Roadmap of the Future, Executive Summary and Recommendations New Delhi: Ministry of Health and Family Welfare and Ministry of Tribal Affairs, Government of India; 2018.
- [Google Scholar]
- Why Leprosy has Resurfaced in India. 2019. Available from: https://www.downtoearth.org.in/blog/health/why-leprosy-hasresurfaced-in-india-63403 [Last accessed on 2021 Jun 14]
- [Google Scholar]
- Tribal population in India: A public health challenge and road to future. J Family Med Prim Care. 2020;9:508-12.
- [CrossRef] [PubMed] [Google Scholar]





