Translate this page into:
Lichenoid pseudovesicular papular eruption on nose through the dermatoscope
Corresponding author: Dr. Suman Patra Department of Dermatology, Venereology & Leprology, All India Institute of Medical Sciences Jodhpur, Jodhpur 342005, Rajasthan, India. patrohere@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jassi R, Singh S, Sharma T, Kaur M, Patra S. Lichenoid pseudovesicular papular eruption on nose through the dermatoscope. Indian J Dermatol Venereol Leprol 2022;88:660-4.
Sir,
Lichenoid pseudovesicular papular eruption on nose (LIPEN) is a newly described entity in dermatology characterized by relatively asymptomatic grouped vesicle-like/pseudovesicular papules on the nose and adjoining facial areas and occasionally on the extensors of arms and dorsum of hands. These lesions histopathologically show a dense focal and/or nodular lichenoid infiltrate in the upper dermis.1 We report four cases with newly described dermatoscopic features.
All four patients presented to the dermatology outpatient department of All India Institute of Medical Sciences Bhopal and Kubba Skin Clinic, New Delhi with asymptomatic erythematous papules on the nose and upper lip. The age of the patients (one man, three women) ranged between 21 and 43 years (mean = 32.3 years). There was no history of photosensitivity, episodic flare of erythema, excessive sweating over the papules or any other history suggestive of connective tissue disease or rosacea. Cutaneous examination showed pinhead-sized erythematous to skin-coloured shiny papules on the tip and alae of the nose and upper lip below the nasolabial fold [Figure 1]. In two of our cases, the forehead and malar areas were involved with confluent plaques and other two cases had extra-facial involvement with tiny papules on the dorsum of the hand, upper back and forearm [Table 1].

- Multiple tiny pseudovesicular papules over nose and upper lip

- Multiple tiny pseudovescicular papules over nose, bilateral cheek and upper lip

- Multiple tiny pseudovescicular papules over nose and upper lip
| S. No. | Age/Sex | Duration | Sites over face | Extra-facial sites | Symptoms | Dermatoscopy | Histopathology | Treatment | Response |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 32 y/man | 6 years | Nose, few papules below the nasolabial fold, | Dorsum of hands | Asymptomatic | Multiple structureless amorphous red clustered clods with scalloped margin, white dots, dark grey globules | Denied | Topical tacrolimus, Oral hydroxychloroquine 400 mg BD, Sun protection |
Lost to follow-up |
| 2 | 21 y/woman | 5 years | Nose, below the nasolabial fold | None | Asymptomatic | Multiple structureless red clustered clods with scalloped margin, white dots, dark grey globules | Basal cell damage, upper dermal moderately dense infiltrate of predominantly lymphocytes and occasionally histiocytes | Topical tacrolimus, Hydroxychloroquine 400 mg bd, sun protection | Minimal improvement |
| 3 | 43 y/woman | 1 year | Nose, forehead, upper lip, | forearm, upper back | Facial lesion asymptomatic. Trunk and extremity mildly itchy |
Amorphous irregular amoeboid shaped orange to red-coloured clods. white areas, white dots, dark grey globules of varying size, linear and arcuate capillaries | Atrophic epidermis. Basal cell damage with pigment incontinence. Upper and mid dermal dense lymphocytic infiltrate | Sun protection, topical tacrolimus | Mild improvement in two months |
| 4 | 45 y/woman | 2 years | Nose, cheeks | none | Asymptomatic | Round to oval yellowish- orange clustered clods with brownish tint in some and pale areas, White dots | Not available | Sun protection and topical tacrolimus | Moderate improvement in three months |
A dermatoscopic evaluation (Heine Delta 20 dermatoscope,® 10×, polarised) of all the four cases showed round to oval, variably sized, yellowish-orange to red clustered clods with pale areas in between, probably corresponding to the lesions and intervening normal skin. There were scattered multiple white dots in both the areas and those at the periphery of red clods, giving the appearance of a scalloped margin [Figures 2a and d]. In addition, there were focal brown dots and a network [Figure 2b]. Linear and arcuate capillaries were seen occasionally in two cases and structureless white areas [Figure 2c] in one case. The white areas were seen only in the patient with larger lesions.
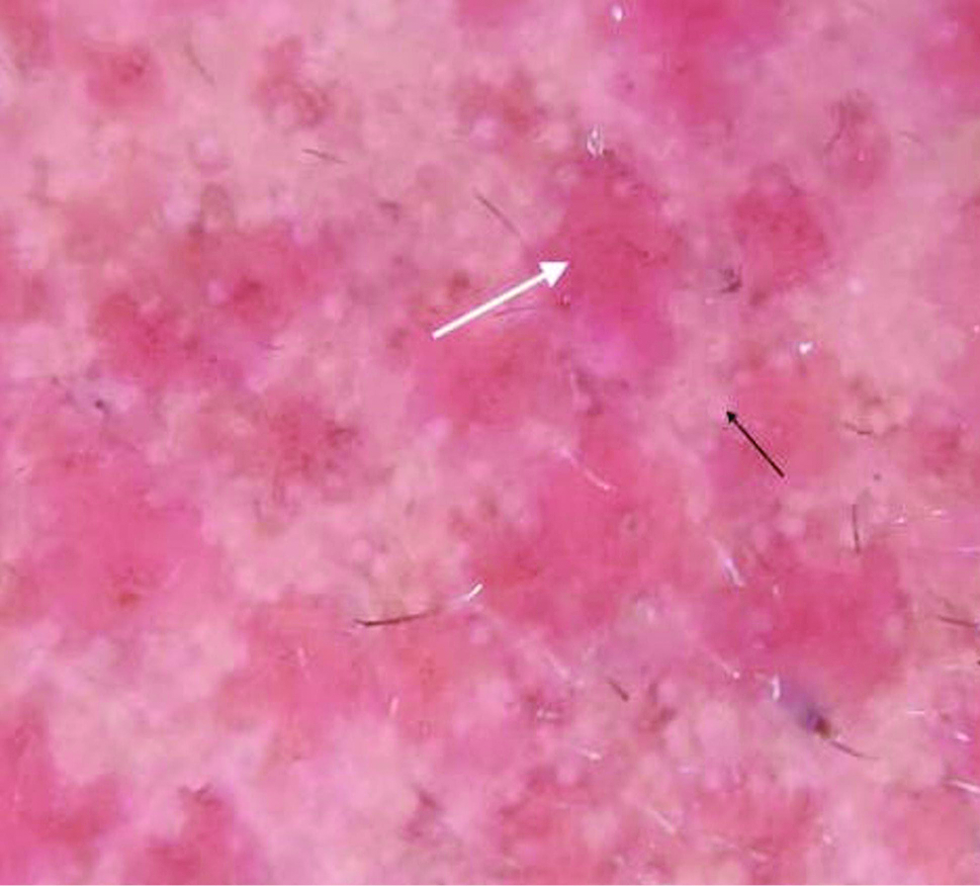
- Dermatoscopic image patient showing structureless red clustered clods (white arrow) with intervening uninvolved areas, scattered white dots at the periphery (black arrow), (Heine delta 20 dermatoscope)

- Dermatoscopic image showing focal brown dots and network (red circle) and linear capillaries (white arrow), ×10 magnification, polarized light, (Heine delta 20 dermatoscope)

- Dermatoscopic image showing red clods along with pale areas (red circle) ×10 magnification, polarized light, (Heine delta 20 dermatoscope)
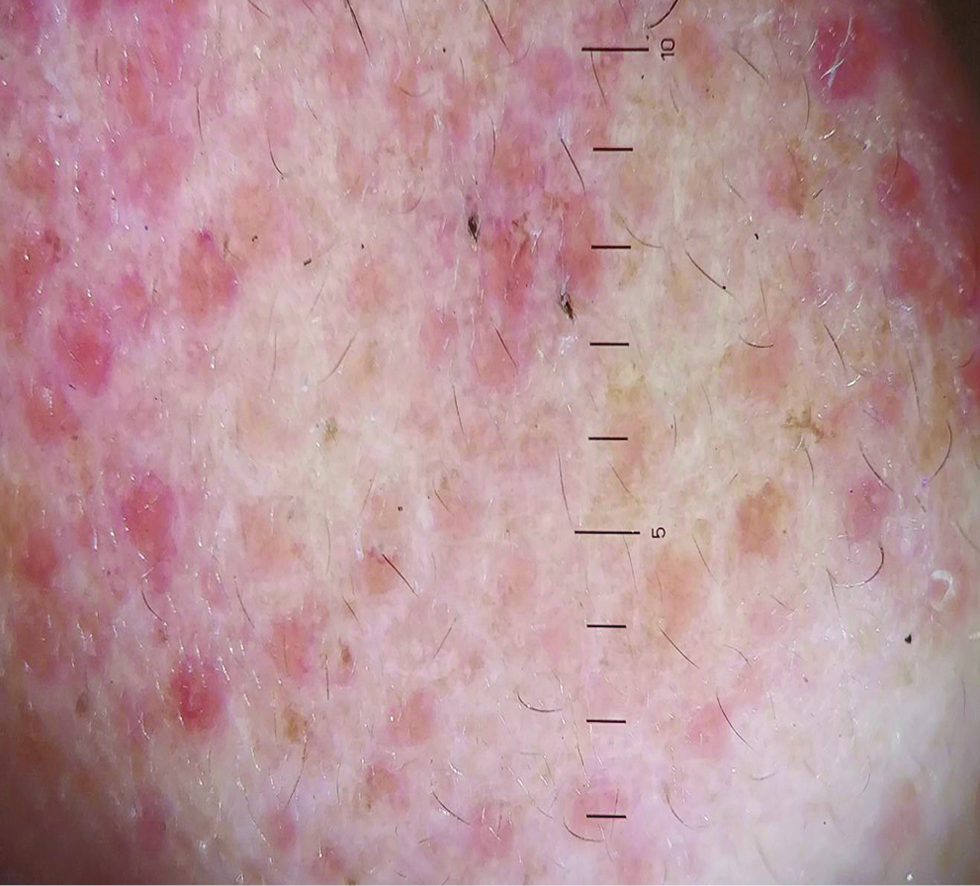
- Dermatoscopic image of fourth patient showing red clustered clods, white dots and pale areas; ×10 magnification, polarized light, (Heine delta 20 dermatoscope)
All routine blood investigations including antinuclear antibodies were within the normal limits. Histopathology was performed in two cases and both showed atrophic epidermis and basal cell vacuolar degeneration of the epidermis. There was significant pigment incontinence in the upper dermis with moderately dense predominantly lymphohistiocytic infiltrate in the upper and mid dermis [Figure 3].
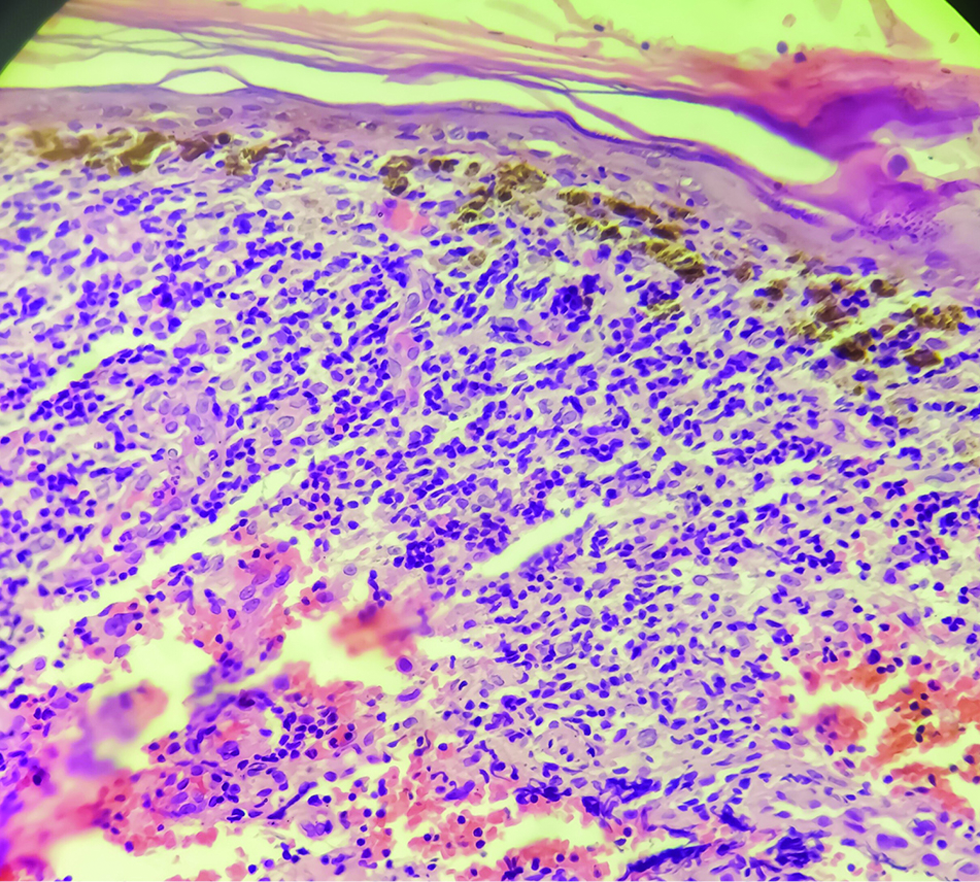
- Histopathology image showing atrophic epidermis, basal cell damage with pigment incontinence. Dense lymphohistiocytic infiltrate in the upper and mid dermis (H&E × 200)
Based on the review of literature, all our cases fit the classical description of lichenoid pseudovesicular papular eruption on the nose. All of them were treated with topical tacrolimus 0.1% ointment at night and hydroxychloroquine 400 mg twice a day in two cases along with strict photoprotection. Two cases had mild response in two months and one case was lost to follow-up.
Singh et al., in a study of 11 patients, described a new entity, lichenoid pseudovesicular papular eruption on the nose, ruling out the common differentials of facial papules like rosacea, granulosis rubra nasi, sarcoidosis, lupus miliaris disseminatus faciei, Jessner lymphocytic infiltrate etc. In addition, lesions were present on the forehead in few of the patients. These papules histopathologically showed a dense lichenoid infiltrate at the dermoepidermal junction.1 LIPEN has primarily been described as a histopathological diagnosis but the dermatoscopic features have not been evaluated yet.
Dermatoscopy showed multiple structureless red clods clustered together with scattered white dots at the periphery in all four of our cases. The colour of the clods was not uniformly red but varied from red to yellowish-orange between patients even at different places in the same patient. The structureless red clods can be correlated with focally dense lymphohistiocytic infiltrate in the dermis. White dots may correspond to eccrine openings.2 The dermatoscopic features of common differentials of lichenoid pseudovesicular papular eruption on the nose has been tabulated in Table 2.3-7 The yellow-orange structureless areas seen in granulomatous differential were absent in LIPEN. Also, the pink-red round to oval structureless areas seen in granulosis rubra nasi were more well-defined than those seen in LIPEN. Follicular plugging is seen only in lupus miliaris disseminatus faciei among all differentials. Histopathology remains the mainstay for diagnosis along with classical clinical features. The difference in dermatoscopic features among close clinical differentials is subtle and looking at those features in a larger cohort could help us to define the findings in a better way.
| S. No. | Differential diagnosis | Classical findings | Our cases (LIPEN) |
|---|---|---|---|
| 1 | Granulomatous rosacea3 | Focal structureless orange areas or clods with linear and branching vessels | Structureless red clustered clods are ill-defined. Linear vessels: occasional, not a consistent finding. No branching vessel. |
| 2 | Sarcoidosis4 | Yellow-orange globule structures with overlying linear, branching and arborising vessels. A scar-like white areas | No yellow-orange globules. No arborising vessels. Fewer amorphous white areas. |
| 3 | Granulosis rubra nasi5 | Discrete round to oval red to pink structureless areas or clods with scattered brown dots | Less well-defined red clods. No brown dots. White dots are present at the periphery of the red clods. Focal brown dots and network. |
| 4 | Acne agminata3 | Focal structureless orange areas, follicular openings with white/yellow keratotic plugs | No follicular opening with plug. |
| 5 | Pseudolymphoma6 | White reticular lines around red globules, linear vessels without branches, perifollicular white colour | Paler and broader areas around orange-red clods. A vascular pattern was not seen. |
| 6 | Nodular amyloidosis7 | Central orange-yellowish homogeneous area with elongated and serpentine telangiectasias | Smaller and multiple clods rather than a large single one. |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of Interest
There are no conflicts of interest.
References
- Lichenoid pseudovesicular papular eruption on nose: A papular facial dermatosis probably related to actinic lichen nitidus or micropapular polymorphous light eruption. Indian J Dermatol Venereol Leprol. 2019;85:597-604.
- [CrossRef] [PubMed] [Google Scholar]
- Pinpoint white dots in the scalp: Dermoscopic and histopathologic correlation. J Am Acad Dermatol. 2010;63:721-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of granulomatous disorders. Dermatol Clin. 2018;36:369-75.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of sarcoidosis: A useful clue to diagnosis. Indian Dermatol Online J. 2018;9:80-1.
- [CrossRef] [PubMed] [Google Scholar]
- Granulosis rubra nasi seen through the dermatoscope. JAAD Case Rep. 2020;6:234-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is dermoscopy useful for the diagnosis of pseudolymphomas? Dermatology. 2021;237:213-16.
- [CrossRef] [PubMed] [Google Scholar]
- A unique dermoscopy pattern of primary cutaneous nodular amyloidosis mimicking a granulomatous disease. J Am Acad Dermatol. 2016;74:e9-e10.
- [CrossRef] [PubMed] [Google Scholar]





