Translate this page into:
Lepromatous leprosy with central serous chorioretinopathy
Corresponding author: Dr. Rohit Singla, Department of Dermatology, Venereology and Leprosy, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India. drrohitsingla25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Goel S, Gogia K, Singla R, Gupta S, Patel K, Verma S. Lepromatous leprosy with central serous chorioretinopathy. Indian J Dermatol Venereol Leprol 2022;88:807-11.
Sir,
Leprosy is being detected in more than 200,000 new cases annually.1 Ocular involvement in leprosy is estimated at 70–75% worldwide.2About 10–50% suffers from severe ocular symptoms and blindness occurs in approximately 5% of cases.2 Erythema nodosum leprosum, also called as type 2 reaction, is a severe multisystem immune-mediated complication in patients with borderline and lepromatous leprosy. The ocular derangements in erythema nodosum leprosum include lagophthalmos, keratitis, episcleritis, scleritis and iridocyclitis.3,4 Central serous chorioretinopathy is a rare complication seen in leprosy that is characterised by a serous detachment of the neurosensory retina at the macula.5,6 Erythema nodosum leprosum is treated mainly with corticosteroids. Steroids are often required for extended period and central serous chorioretinopathy worsens with systemic steroids. Hence it should be managed cautiously with regular follow-up. We herein report a case of rare association of central serous chorioretinopathy in a patient of lepromatous leprosy with erythema nodosum leprosum.
A 37-year-old man presented with epistaxis and slipping of footwear for four months. He gave a history of numbness and tingling sensation on bilateral lower and upper extremities. This was insidious in onset and gradually progressive. On examination, the patient had numerous shiny erythematous macules which were symmetrically distributed on both thighs and sensations on the lesions were intact [Figure 1a]. Posterior auricular nerve was thickened bilaterally [Figure 1b]. Sensation to hot and cold was lost on bilateral upper and lower extremities. The patient refused biopsy, however, slit skin smear showed bacterial index of +4. The patient was diagnosed as a case of Hansen disease (lepromatous leprosy) and was started on multibacillary multidrug therapy. He came for follow-up and gave a history of low-grade fever with joint pain every two to three days for the past one month which resolved on taking medications. The patient also complained of multiple painful reddish nodules on face and extremities which were transient, episodic and appeared with onset of fever. On examination, multiple erythematous tender nodules measuring 2–3 cm in diameter were noted on face and bilateral ears. Bilateral posterior auricular nerves and common popliteal nerves were tender. His blood counts and liver function tests were normal. He was diagnosed with erythema nodosum leprosum. The ENLIST erythema nodosum leprosum severity score was 9 in our case.

- Shiny erythematous macules on right thigh

- Thickened posterior auricular nerve
The patient also complained of blurring of vision associated with redness in both the eyes for past 20 days for which he was referred to ophthalmology department. He also complained of watering and photophobia. There was no history of any discharge, trauma, diabetes, hypertension or steroid intake in any form. Best-corrected visual acuity was 6/60 in the right eye and 6/36 in the left eye. On examination, there was madarosis in both eyes and lagophthalmos in the left eye [Figure 2a]. Superficial punctate keratitis, plasmoid aqueous with 4+ cells in anterior chamber with posterior synechiae and pigments on anterior lens capsule were noted in the right eye whereas the left eye had superficial punctate keratitis with 2+ cells and flare in the anterior chamber [Figures 2b and 2c]. Dilated fundus examination showed subretinal fluid at macula in both eyes [Figures 3a and 3b]. The right eye fundus view was hazy due to presence of posterior synechiae. Fundus fluorescein angiography was done. The right eye showed hyperfluorescence nasal to fovea [Figure 3c]. The left eye showed ink blot leak superior to fovea [Figure 3d]. A diagnosis of bilateral anterior uveitis and central serous chorioretinopathy was made. The patient was advised to use topical steroids in a tapering dose, cycloplegics along with lubricants and continued multibacillary multidrug therapy. As central serous chorioretinopathy worsens with oral steroids, the patient was started on oral methotrexate weekly and the dose of clofazimine was increased to 300 mg/day along with ibuprofen for the treatment of erythema nodosum leprosum. On follow-up after three weeks, anterior chamber reaction had resolved and fundus view showed improvement. Fundus of the right eye showed shallow subretinal fluid with retinal pigment epithelial detachment and fibrin nasal to fovea and the left eye fundus showed decrease in subretinal fluid [Figures 4a and 4b] that was confirmed on spectral domain optical coherence tomography (SDOCT) [Figures 4c and 4d]. The patient was advised to stop topical steroids and cycloplegics and is under regular follow-up.

- Madarosis in both eyes and lagophthalmos in the left eye
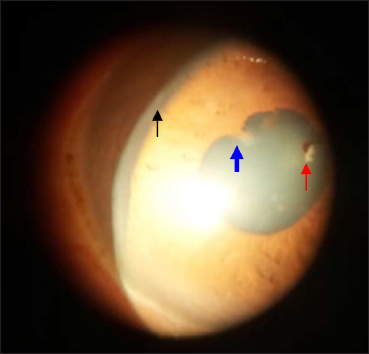
- Right eye showing superficial punctate keratitis (black arrow), posterior synechiae (blue arrow) and pigments on anterior lens capsule (red arrow)
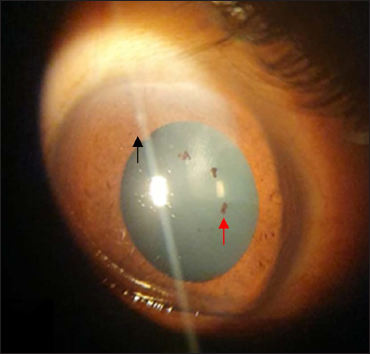
- Left eye showing superficial punctate keratitis (black arrow) and pigments on anterior lens capsule (red arrow)
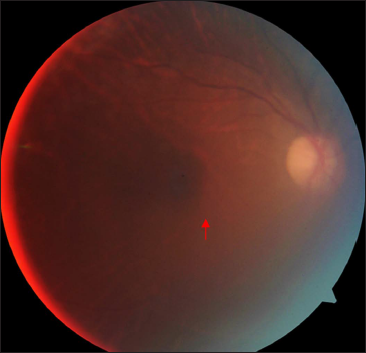
- Colour fundus photograph of the right eye showing shallow subretinal fluid at macula (red arrow). Fundus view is hazy due to presence of posterior synechiae
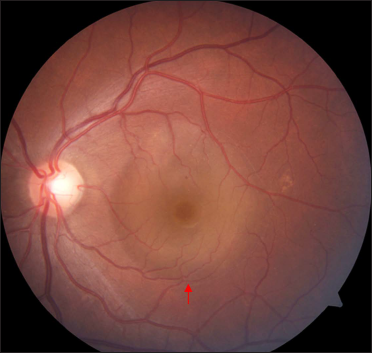
- Colour fundus photograph of the left eye showing subretinal fluid at macula (red arrow)
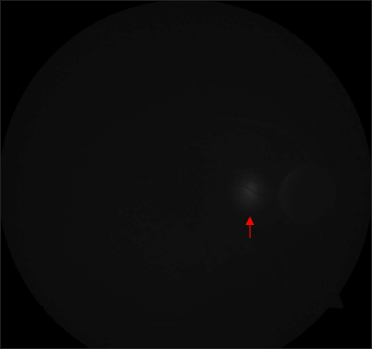
- Fundus fluorescein angiography of the right eye showing hyperfluorescence nasal to fovea (red arrow)
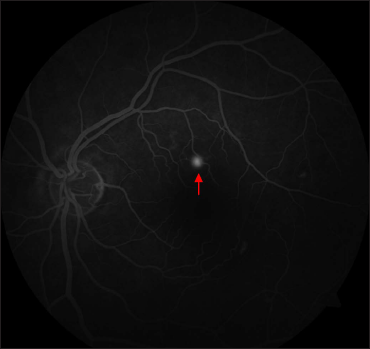
- Fundus fluorescein angiography of the left eye showing ink blot leak superior to fovea (red arrow)
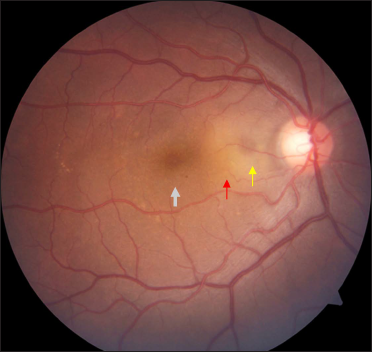
- Fundus of the right eye showing shallow subretinal fluid (white arrow) with fibrin (red arrow) and pigment epithelial detachment (yellow arrow) nasal to fovea on follow-up
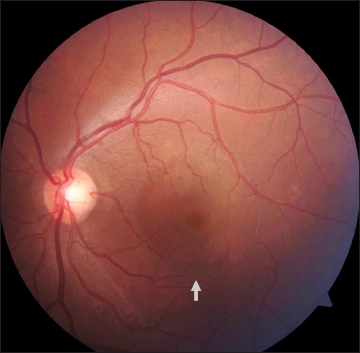
- Fundus of the left eye showing decrease in subretinal fluid at macula (white arrow) on follow-up
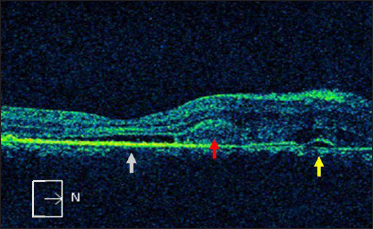
- Spectral domain optical coherence tomography of the right eye in the corresponding area showing shallow subretinal fluid (white arrow) with fibrin (red arrow) and pigment epithelial detachment (yellow arrow) nasal to fovea
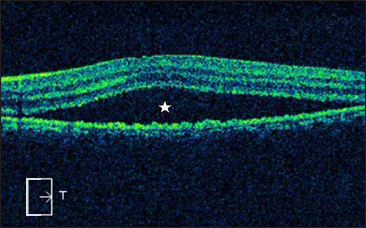
- Spectral domain optical coherence tomography of the left eye in the corresponding area showing subretinal fluid at macula (star)
Ocular involvement in Hansen disease can be due to direct infiltration by the mycobacteria or due to the immune damage caused by reactionary episodes in leprosy. Paralysis of the seventh nerve gives rise to the weakness of the orbicularis muscle with ectropion and lagophthalmos. Paralytic ectropion and lagophthalmos subsequently give rise to exposure keratitis, corneal ulceration and scarring. Cornea may show superficial punctate opacities and interstitial keratitis particularly in the upper and outer quadrant. In some cases, minute nodules or ‘pearls’ will be seen on the surface of the iris.7 It is extremely rare to see posterior segment involvement in leprosy. A rare association of retinochoroiditis and central serous chorioretinopathy is reported in literature.5,7,8
Central serous chorioretinopathy is an idiopathic disorder characterised by a localised serous detachment of the neurosensory retina at the macula. The patient commonly presents with central scotoma, metamorphopsia associated with a modest reduction in the visual acuity. This condition is associated with psychological factors. Risk factors include males with type A personality, emotional stress, steroid intake and Cushing syndrome. Rarely, it can be associated with leprosy.5,8 Elevated levels of circulating tumour necrosis factor (TNF)-α as well as expression of interleukin (IL)-6 and interferon (IFN)-γ in the serum and cutaneous lesions of patients with erythema nodosum leprosum are reported.9 IL-6 is a multifunctional cytokine that is essential for the regulation of immune processes. It increases vascular permeability and angiogenesis by inducing the expression of vascular endothelial growth factor (VEGF). Increased concentration of pro-inflammatory cytokines, such as IL-6, IL-8, monocyte chemoattractant protein (MCP)-1 and interferon gamma inducible protein (IP)-10, is found in central serous chorioretinopathy patients.10 Central serous chorioretinopathy can occur due to increased VEGF that enhances choroidal vascular hyperpermeability.8,10 This causes increase in choroidal hydrostatic pressure that overcomes the retinal pigment epithelium barrier function, causing accumulation of subretinal fluid and retinal pigment epithelial detachment.
Acute central serous chorioretinopathy is usually a self-resolving condition. Most cases heal spontaneously in four–eight weeks with recovery of visual acuity in six months. Persistence of symptoms with presence of subretinal fluid beyond three–four months warrants treatment. Various treatment modalities such as focal laser photocoagulation, micropulse diode laser photocoagulation, transpupillary thermotherapy, photodynamic therapy with verteporfin and multiple anti-corticosteroids agents have been proposed for the treatment of central serous chorioretinopathy. Focal laser and photodynamic therapy are the preferred modalities and have been found to be effective in this condition. As glucocorticoids are implicated in the development of central serous chorioretinopathy, glucocorticoid inhibition with rifampicin has been suggested as a potential treatment modality. Rifampicin is known to induce cytochrome P450 3A4 that increases the metabolism of endogenous steroids with an improvement in clinical features of central serous chorioretinopathy with resolution of subretinal fluid. As the drug is hepatotoxic, liver function tests should be done at baseline and repeated every month till cessation of the drug. These patients require regular observation with regulating the exacerbating factors such as stress and systemic steroid use. Therefore, to avoid systemic steroids for the management of erythema nodosum leprosum, alternative therapies such as immunosuppressants (methotrexate, azathioprine, cyclosporine and mycophenolate mofetil), antimalarial drug (chloroquine) and clofazimine in higher dose can be given to such patients. Thalidomide is another effective treatment of erythema nodosum leprosum; however, its use is limited due to the risk of teratogenicity and neurotoxicity.
This case letter highlights the association between central serous chorioretinopathy and leprosy that is rarely reported in literature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global leprosy update, 2018: Moving towards a leprosy free world. Wkly Epidemiol Rec. 2019;94:389-412.
- [Google Scholar]
- Evaluation of ocular involvement in patients with Hansen’s disease. PLoS Negl Trop Dis. 2020;14:e0008585.
- [CrossRef] [PubMed] [Google Scholar]
- Clinico-pathological features of erythema nodosum leprosum: A case-control study at ALERT hospital, Ethiopia. PLoS Negl Trop Dis. 2017;11:e0006011.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular manifestations of Hansen’s disease. Doc Ophthalmol. 1994;87:211-21.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic central serous chorioretinopathy. Indian J Ophthalmol. 1998;46:131-7.
- [PubMed] [Google Scholar]
- Central serous chorioretinopathy in Hansen’s disease–an entity unknown. Acta Sci Ophthalmol. 2019;2:7-8.
- [Google Scholar]
- Differential expression of IFN-γ, IL-10, TLR1, and TLR2 and their potential effects on downgrading leprosy reaction and erythema nodosum leprosum. J Immunol Res. 2019;2019:3405103.
- [CrossRef] [PubMed] [Google Scholar]
- Association of upregulated angiogenic cytokines with choroidal abnormalities in chronic central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2018;59:5924-31.
- [CrossRef] [PubMed] [Google Scholar]





