Translate this page into:
Implementation of National Leprosy Eradication Programme during COVID-19 era: A qualitative research
Corresponding author: Dr. Nilay Kanti Das, Department of Dermatology, Bankura Sammilani Medical College, Bankura, West Bengal, India. drdasnilay@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhattacharya T, Das S, Sarkar AP, Patra AC, Sarkar D, Das NK. Implementation of National Leprosy Eradication Programme during COVID-19 era: A qualitative research. Indian J Dermatol Venereol Leprol 2023;89:393-402.
Abstract
Introduction
The COVID-19 pandemic imposed new challenge to the implementation of the National Leprosy Eradication Programme. According to national data, after lockdown due to COVID-19, there was a 29% reduction in total leprosy cases reported in the first quarter (April-June) of 2020 in comparison to 2019.
Objectives
To explore the difficulties faced by different stakeholders of the National Leprosy Eradication Programme like policy makers, doctors, grass root level health workers as well as leprosy patients during COVID-19 pandemic with respect to programme implementation and access to leprosy care.
Materials and Methods
Qualitative research was undertaken including two focus-group-discussions held among six leprosy patients diagnosed after lockdown and nine ASHA workers as well as six in-depth interviews of doctors, leprologists, and programme managers. Ethics committee approval was sought and informed consent was obtained from all participants. All focus-group-discussions were electronically recorded and the in-depth interviews telephonically recorded, transcribed and translated from Bengali-to-English. Transcripts were separately coded by researchers and thematically analysed with the help of Visual-Anthropac software version 1.0.
Results
Solitary focus on COVID-19 control, capacity building and information, education and communication, leprosy case search & surveillance, co-infection among health workers, transportation issues were the themes explored from focus-group-discussions of health workers and ASHA workers. Similarly, the present study identified six themes from in-depth interviews of programme manager, leprologists, programme manager as diagnostic difficulty, operational issues, rehabilitation issues, capacity building & information education and communication activities and way forward.
Limitations
The research reveals the perceptions of rural population of Eastern India with high leprosy prevalence, which might not be applicable for urban areas or low prevalent districts
Conclusion
The solitary focus of the administration towards COVID and shifting the infrastructure and human resource only towards the management of COVID can lead to resurgence of the leprosy. Having an organised framework of operations, catering to the need of the front-line workers in rendering services, utilizing the digital platform and social media, and focusing on rehabilitation would be needed to overcome the crisis.
Keywords
National leprosy eradication programme
COVID-19
leprosy
focus group discussion
in-depth interview
qualitative research
Plain Language Summary
COVID-19 pandemic imposed new challenges to the implementation of the National Leprosy Eradication Programme. This study explored the difficulties faced by different stakeholders of National Leprosy Eradication Programme including policy makers, doctors, grass root level health workers as well as leprosy patients during the COVID-19 pandemic, with respect to programme implementation as well as accessing leprosy care. A qualitative research comprising of focus-group-discussions and in-depth interviews among doctors, leprologists and programme manager was conducted after obtaining ethics-committee permission and consent from participants. Solitary focus on COVID-19 control, capacity building and information education and communication, leprosy case search and surveillance, co-infection among health workers and transportation issues were the six themes explored from focus-group-discussions of health workers and ASHA workers. Similarly, five themes were identified from in-depth interviews of programme managers and leprologists, namely, diagnostic difficulty, operational issues, rehabilitation issues, capacity building & information education and communication activities and way forward. Solitary focus of the administration on COVID-19 and shifting of infrastructure and human resource only towards the management of COVID-19 can lead to the resurgence of leprosy. Having an organised framework of operations, catering to the needs of front-line workers in rendering services, utilising digital platforms and social media and focussing on rehabilitation would be needed to overcome this crisis.
Introduction
Leprosy, the chronic infectious disease caused by Mycobacterium Leprae, if left untreated has the potential to cause progressive physical, psychological and social disabilities.1 The National Leprosy Control Programme, which was launched in India in 1955, aimed at controlling leprosy using survey, education and dapsone monotherapy. The programme was renamed as National Leprosy Eradication programme in 1983 with the introduction of multi-drug treatment. The goal was to eliminate of leprosy as a public health problem (less than 1 case per 10,000 population) by the year 2000 AD. The programme successfully reduced the national prevalence of leprosy from 57.6/10,000 in March 1981 to 2.44 per 10,000 in March 2004.2 With continued and sustained effort, India successfully achieved the goal of elimination of leprosy in December, 2005, when the prevalence rate in the country was recorded as 0.95/10,000 population. Even after these efforts, India continued to record the highest number of new leprosy cases globally followed by Brazil and Indonesia. In 2008, 2.5 lakh new cases of leprosy were recorded globally and India accounted for 1.37 lakh, of those cases 35% were women.3 In West Bengal, on 1 April, 2008, the prevalence rate was recorded to be 0.74/10,000, which rose to 0.99 in 1st April 2009.4 A performance assessment report in March 2010 revealed that out of 19 districts, in West Bengal, 10 districts had attained elimination status, whereas the remaining nine still had a prevalence rate more than 1 per 10,000 population, including Bankura and Purulia with a prevalence of more than 2 per 10,000.4 A total of 127,334 new cases were detected in India during the year 2015-16, which implied an annual new case detection rate of 9.71 per 100,000 population, as against 125,785 cases in 2014-15. A total of 86,028 leprosy cases were on record as on 1st April 2016, giving a Prevalence Rate of 0.66 per 10,000 population, as against 88,833 cases in 1st April 2015.5 The case load and prevalence rate further declined to 80,000 and 0.57/10,000 population on 1st April 2020.6 Detailed information on 57,672 new leprosy cases detected during 2020-21 indicated that the proportions of multibacillary leprosy cases (58.10%), females (39.05%), children (5.76%) patients with grade II deformity (2.41%), scheduled tribe cases (20.13%) and scheduled caste cases (17.74%) remained burning issues.5 As per recent reports, some persistent hotspots in two states (Odisha and Chattisgarh) and one union territory (Dadra and Nagar Haveli) are yet to achieve elimination.6 In a report from the department of health and family welfare, West Bengal, the number of new cases in 2008-09 from Bankura, Birbhum and Purulia was 3203 which represented 26.9% of 11,891 cases from the whole of West Bengal; notably 65 among them presented with grade 2 deformity.7
Understandably, the hotspot of leprosy in West Bengal (which includes the district of Bankura) needs special attention to eliminate the leprosy burden. The focus is on early diagnosis and treatment of leprosy, thereby reducing the chance of developing deformities, psychological stress or any type of reactions.
Amidst this situation COVID-19 brought a new challenge to the implementation of the programme. WHO declared it a pandemic on 11th March 20208 and in an effort to contain the spread of this disease, ‘lockdowns’ were implemented in different parts of the world. In India, the government enforced a total lockdown on 24th March 2020 for 21 days. It was later extended up to 31s May 2020, taking the total number of days under lockdown to beyond 50 days.9 All the non-emergency out-patient departments in India were to be shut; and only emergency healthcare services were allowed to function. Leprosy being a non-emergency disease was likely to be affected by this lockdown. In addition to the lockdown, social distancing norms were also being enforced which had the potential to interfere with the clinical examination and reconstructive surgeries. Under these circumstances this study was undertaken to understand the impact of COVID-19 on the implementation of the National Leprosy Eradication Programme. Various stakeholders including policy-makers, doctors, other healthcare staff and leprosy patients were interviewed to explore the threat to the leprosy programme imposed by COVID-19.
The findings of our study can assist policy-makers in modifying the leprosy programme accordingly and so as to deliver the best outcome to patients.
Materials and Methods
This study was conducted between December, 2020-February, 2021. The study population included newly diagnosed leprosy patients attending the dermatology outpatient department of Bankura Sammilani Medical College situated in a high prevalence district of eastern India, who were diagnosed after 25th March 2020, i.e., after announcement of lockdown as well as various healthcare workers like accredited social health activists (ASHA), health assistants, district level programme manager, non-governmental organization (NGO) consultant, doctors, leprologists and reconstructive surgery clinic in-charge. Participants who were unwilling and unable to speak Bengali were excluded from the study. Thus, six newly diagnosed leprosy patients in the reference period and nine ASHA workers were recruited for focus-group-discussions. Additionally, six in-depth interviews of leprologists, doctors, district level programme managers and an NGO consultant were carried out.
Background characteristics of leprosy patients were collected using a semi-structured schedule. A separate guide was prepared for conducting focus-group-discussions and in-depth interviews with a few overlapping questions keeping in mind the respondents, eg., questions on administrative and logistical issues were posed to the programme managers, while questions on difficulties faced in accessing healthcare were addressed to the leprosy patients.
Two focus group discussions involving 15 study subjects who fulfilled the eligibility criteria were conducted to explore their views towards the implementation of the National Leprosy Eradication Programme. One focus-group-discussion session was conducted among six leprosy patients in the outpatient department of Bankura Sammilani Medical College and another focus-group-discussion was held with nine ASHA workers at the community health centre of Chatna block of Bankura District, West Bengal. Focus-group-discussions were carried out with the help of a predetermined focus-group-discussion guide composed of some guiding questions. There was a moderator for conducting the discussion and a recorder to note down the proceedings. Participants were asked to sit in semi-circular manner so that each one of them was within view of the others. A predetermined logical sequence of open-ended questioning was done to stimulate discussion among the participants to understand their perceptions, treatment seeking behaviour and whether they faced any difficulties. Participants were asked questions in a neutral manner, their responses were heard attentively and if necessary, follow-up questions were asked. There were no leading questions and participants were not shown approval or disapproval related to what they said. The complete proceedings of the focus-group-discussion including level of participation and sociogram were noted, and it revealed equal levels of participation among the respondents. These sessions were electronically recorded, and each lasted for not more than 30 minutes.
Besides the focus-group-discussions, a total of six in-depth telephonic interviews were undertaken to elicit challenges faced by leprologists as well as leprosy programme managers. Each interview involved one interviewer and one participant and lasted for not more than 20 minutes. After formal introduction of the interviewer, participants were asked questions in a neutral manner, their responses were heard attentively and if necessary follow-up questions were asked. All interviews were electronically recorded.
Data collection and analysis were done simultaneously. After each focus-group-discussion and in-depth interview, data including all field notes and recorded audio were transcribed at first and then translated from Bengali into English; close to verbatim, on the day of data collection itself. All researchers then coded interview transcripts separately and any discrepancies in the coding were sorted out following exhaustive discussion. These coded notes were thematically analysed and emerging themes were identified with illustrative quotations. Statements in italics indicate direct quotations from the participants.
Finally, free listing using Smith’s Salience score and a pile sorting exercise was conducted.9 Smith’s S (Smith’s saliency score) refers to the importance, representativeness or prominence of items to individuals or to the group, and is measured in three ways: word frequency across lists, word rank within lists and a combination of these two.10 Smith saliency index suggests a weighted mean that takes into account the number of items on a participant’s list, placement of the item on the participant’s list, and the frequency with which an item was mentioned.11 In the pile sorting exercise, the individual participants were asked to group those difficulties which they felt went together.12 It means items under same pile were related and similar according to the participants. The data were analysed by Visual Anthropac version 1.0 software.13 To get the collective picture, two-dimensional scaling and hierarchical cluster analysis of pile sort data were undertaken.12 Multi-dimensional scaling is a tool for quantitative analysis indexing similarity in judgments. Multi-dimensional scaling produces a two-dimensional map of the data reflecting how they were sorted by the respondents. The spatial distance model of multi-dimensional scaling, maps objects as points, in a multidimensional space such that the objects are perceived similar, the nearer they are positioned in the spatial map. Thus, items that are closest together on a multi-dimensional scaling map are items considered similar by the respondents, while dissimilar items are placed farther apart.14 Using both multi-dimensional scaling and hierarchical cluster analysis to interpret data is a common practice among researchers in a variety of situations.15 The cluster analysis results can indicate the actual connections between items near each other on a multi-dimensional scaling map. The participants of focus-group-discussions (FGDs) were debriefed regarding the findings of the free list, pile sorting exercise and focus-group-discussions to increase the credibility of the results. The debriefing was done to leprosy patients in their subsequent clinic visit and for debriefing the ASHA workers a second visit was made to the block. In the debriefing meeting apart from explaining the results of the study and its implications, the queries of the participants regarding leprosy and its treatment were also answered.
The study received ethical clearance from the institutional ethics committee and informed consent was obtained from each respondent. They were assured regarding anonymity and confidentiality of their responses.
Result
Background characteristics
Totally fifteen study subjects (12 females and 3 males) participated in the two focus-group-discussions. The mean age of participants was 41 ± 10.1 years; median was 45 years and the inter-quartile range was 38-47 years. The majority of study subjects were from rural areas (n = 12, 80%) and were below the poverty line (n = 9, 60%). The leprosy patients who participated in the focus-group-discussion were all of the multi-bacillary spectrum and were economically below poverty line. The male:female ratio was 1:1 and mean age was 34.83 ± 13.47 years (median 34.5, inter-quartile range 22-47 years). The patients were under treatment for a mean duration of 6 ± 1.89 months (median: six months, range: 3-9 months)
Two focus-group-discussions among leprosy patients and ASHA workers and six in-depth interviews among doctors and programme managers identified several difficulties and challenges in the National Leprosy Eradication Programme implementation. Major themes that emerged during focus-group-discussions and in-depth interview were summarized separately (though there was an overlap of response and some were common themes) as follows:
A] Themes explored from focus-group-discussion
Solitary focus on COVID-19
It emerged from the focus-group-discussion of ASHA worker (as well as in-depth interviews of several programme managers) that during the initial phase of the pandemic, the prime focus was on control of COVID-19 and all other National programmes came to a pause. ASHA workers who are social mobilisers and play a profound role in case detection were compelled only to do COVID-19 related work. One ASHA worker told that “We couldn’t give time to leprosy programme as we were compelled to get involved in COVID-19 related work.”
Capacity building & information education and communication
Capacity building activities suffered a great blow as overall training of medical officers, public health nurses, other health care staff and grass root level workers were hampered due to pandemic since March 2020. One of the ASHA workers shared, “Every year two or three training programmes for us had been organised but no such training programmes were organised till now, this year.”
Similarly, information education and communication activities had come to a halt up to September 2020 since the starting of lockdown. According to one ASHA worker: “Government is not making adequate announcements or campaigning using loudspeakers/leaflets etc regarding leprosy and all announcements are related to COVID.”
Leprosy case search & surveillance
Active search for leprosy cases also got hampered as people were sceptical about visit by health workers to their house during pandemic. In some areas ASHA workers were debarred from doing home visits. One ASHA worker stated that “In the initial days we were not allowed to enter households by some families.” Another one recounted, “I was permitted to enter some households but not allowed to weigh their babies.” The ASHA workers used to make phone-calls to the household to ensure the well-being of residents during those periods.
Co-infection among Health workers
Several Healthcare workers contracted COVID-19 infection and were quarantined which impacted the National Leprosy Eradication Programme by leading to greater burden on the existing staff. One ASHA worker told that “One ASHA worker and one auxiliary nurse midwife were found to be suffering from COVID-19 and their work at that time was done by another ASHA worker.”
Transportation issues
To tackle the COVID pandemic lockdowns were implemented nationwide, crippling the transport system. For health workers residing far away from their place of work, the commute was immensely challenging. One such health worker stated that “I had to use private transport to do village home visits as no buses, auto-rickshaw were available.”
Suggestion
The ‘SPARSH’ programme envisioned the elimination of stigma attached to the disease but eventually COVID-19 imposed physical distancing thus one of our study participants came up with the idea of revamping ‘SPARSH’ programme into ‘NAMASHKARAM PROGRAMME’ when she said, “Instead of touching the patient we can do ‘Namashkaram’ to express our feeling that we respect them and do not consider them socially isolated.”
As COVID-19 greatly impacted information education and communication activities associated with National Leprosy Eradication Programme we must come up with newer, feasible ways for information education and communication promotion. COVID-19 taught us that social media platforms can be greatly helpful in these times of crisis for information education and communication promotional activities. One ASHA worker told us that “caller tune of mobile network operators can do information education and communication announcements just like they were doing for COVID-19.” We should come up with newer interesting ways like the above mentioned one for information education and communication activities.
B] Themes that emerged from in-depth interviews
Diagnostic difficulties
Existing manpower was deputed for COVID-19 related jobs in the initial days leading to problem for case detection. One of the leprologists remarked, “Investigations like Slit skin smear for AFB and skin biopsy for diagnosis of doubtful case were hampered since the beginning of pandemic.”
Operational issues
The active search for leprosy cases also got hampered as people were sceptical about visits by health workers to their house during the pandemic. According to one programme manager “NLEP had suffered a lot like any other national programme since March, 2020 due to solitary focus on control of COVID-19 infection.” Several health workers also got infected by COVID-19 which impacted the National Leprosy Eradication Programme by increasing the burden on existing staff.
Due to the lockdown many patients who required frequent follow-up visits (especially with type 2 Lepra reaction) couldn’t come to hospitals for treatment. Doctors also had difficulties admitting such patients due to the unorganised framework as well as communication gaps since March. Regarding multi drug treatment and microcellular rubber chappals, one of the programme managers said that “as leprosy cases were detected less, hence MDT, microcellular rubber chappals and splint requirements were reduced. Also, the procurement was done just at the beginning of the month of March 2000, thus the lockdown did not affect it.” However, the respondent stated that delivery of microcellular rubber chappals got delayed especially up to September 2020. Another programme officer reported that “Reconstructive surgery camp could not be conducted during lockdown period.” Migration of people during the pandemic also posed challenges for drug distribution to patients. Many patients couldn’t receive medicine due to migration leading to increase in defaulter cases.
Rehabilitation issues
The employment and livelihood of leprosy patients suffered a lot due to lockdown. According to one respondent, “Education of leprosy affected children came to a standstill as they don`t have smartphones.”
One of the programme managers remarked that “After school learning centre for leprosy affected children as well as Skill centre for leprosy patients in the leprosy colony were closed down during lockdown leading to challenges of rehabilitation”
However, district authorities had provided economic support to leprosy patients in some of the leprosy colonies. Some economic and social help was also rendered at personal level by the health workers to those who stay in the leprosy colony.
Capacity building and information education and communication
Overall training of medical officers, public health nurses, other health care staff and grass root level workers was hampered due to the pandemic since March 2020. Similarly, information education and communication activities had come to a halt up to September 2020 since the starting of lockdown.
Way forward
Clinical examination of the patients also got affected as several health workers were apprehensive of coming close to patients. “Detailed examination of suspect cases including nerve palpation was difficult due to fear of contracting COVID-19 among health workers, hence if proper PPE is provided in future then it will help to remove fear” remarked one respondent. One of the programme managers suggested that “Tracking of defaulters should be carried out if such a pandemic occurs in future.”
Finally, whole free listed items (with Smith’s S score) of challenges/issues elicited are presented in Table 1 (for focus-group-discussions of frontline workers and patients) and Table 2 (for in-depth interview of programme managers and doctors). Items with higher Smith’s Salience score were more frequently reported by the respondents. Thus “solitary focus on COVID-19 control” was the most important issue raised by both the frontline workers/leprosy patients (Smith’s S score 0.856) and the key respondents (Smith’s S score 0.692). Subsequently, six themes from focus-group-discussion and five themes from in-depth interview emerged after pile sorting including solitary focus on COVID-19 control, capacity building and information education and communication, leprosy case search & surveillance, co-infection among health workers, transportation issues, suggestion (from focus-group-discussion) [Table 3] and diagnostic difficulties, operational issues, rehabilitation issues, capacity building and way forward (from in-depth interview) [Table 4]. Thematic analysis of difficulties and challenges in implementation of the National Leprosy Eradication Programme are presented separately for focus-group-discussion [Figure 1] and in-depth interview [Figure 2].
| Items | Smith’s salience score |
|---|---|
| Solitary focus on COVID-19 control | 0.856 |
| ASHAs debarred from home visits | 0.587 |
| Active case surveillance has been reduced | 0.485 |
| ASHAs were compelled to get involved in COVID-19 related work | 0.475 |
| No capacity building activities in the initial days though virtual training has been started since November 2021 | 0.381 |
| Information Education and Communication activities came to a halt | 0.370 |
| Several health workers got COVID-19 infection overburdening others | 0.339 |
| Caller tune of mobile phones can use Information Education and Communication message regarding leprosy just like COVID-19 | 0.160 |
| Some health workers had to use own vehicle to attend job since public transport was not plying | 0.146 |
| ’Namashkaram’ can be used in place of touch to maintain social distancing | 0.133 |
| Reaction patients could not come to hospital due to lockdown | 0.125 |
| ASHAs made phone calls to household to enquire about well being | 0.067 |
| Items | Smith’s salience score |
|---|---|
| Solitary focus on COVID-19 control | 0.692 |
| New case detection delayed as other than fever/emergency nobody turned up | 0.644 |
| Lepra reaction and relapse case diagnosis hampered | 0.500 |
| Patients needing admissions were denied due to un-organized framework in initial days | 0.475 |
| Histopathology and slit skin smear could not be done | 0.466 |
| Nerve palpation not done due to fear of coming close to patients | 0.423 |
| Reconstructive surgery camp could not be undertaken | 0.421 |
| Microcellular rubber chappal procurement faced no issues but delivery got delayed in some areas | 0.416 |
| Increased defaulter cases as patients migrated from place of taking MDT | 0.404 |
| Release from treatment was delayed | 0.364 |
| Lepra reaction/ENL patients could not attend OPD | 0.327 |
| Government also urged that only emergency cases should attend hospitals during initial months of lockdown | 0.296 |
| Examination of patients should be carried out with proper PPE in future so that diagnosis does not get hampered | 0.271 |
| Tracking of defaulters should be carried out | 0.257 |
| Lepra reaction cases were managed with steroids in spite of COVID-19 | 0.250 |
| MDT procurement did not face any challenges | 0.231 |
| No capacity building activities till November | 0.223 |
| Microcellular rubber chappals procurement faced no issues but delivery got delayed in some areas | 0.173 |
| Employment and livelihood of leprosy patients suffered due to lockdown | 0.136 |
| Defaulter tracking is more difficult in urban areas | 0.112 |
| After school learning centre for leprosy affected children closed down | 0.068 |
| Education of leprosy affected children came to a standstill as they didn’t have smartphones | 0.063 |
| Patients in leprosy colony were given economic support by District initiatives | 0.058 |
| Skill centre for leprosy patients in leprosy colony were closed | 0.053 |
| Pile number | Theme | Difficulties faced by respondents in NLEP implementation |
|---|---|---|
| 1. | Solitary focus on COVID-19 control | 1. Solitary focus on COVID-19 control 2. ASHAs were compelled to involved in COVID-19 related work |
| 2. | Capacity building and Information Education and Communication | 1. No capacity building activities in initial days though virtual training has started since November 2020 2. Information Education and Communication activities came to a halt |
| 3. | Leprosy case search & surveillance | 1. Active case surveillance has been reduced 2. ASHAs debarred from home visits 3. ASHAs made phone calls to households to enquire about well being |
| 4. | Co-infection among Health workers | 1. Several health workers got COVID-19 infection overburdening others |
| 5. | Transportation issues | 1. Patients in Lepra reaction needing immediate medical care could not come to hospital due to lockdown 2. Some health workers had to use own vehicle to attend their jobs since public transport was not plying |
| 6. | Suggestion | 1. Caller tunes of mobile phones can use Information Education and Communication message regarding leprosy just like COVID-19 2. ‘Namashkaram’ can be used in place of ‘Sparsh’ (touch) to remove stigma while maintaining social distancing |
| Pile number | Theme | Difficulties faced by respondents in NLEP implementation | Reasons for grouping |
|---|---|---|---|
| 1 | Diagnostic difficulty | 1. Histopathology and slit skin smear could not be done 2. Lepra reaction and relapse case diagnosis hampered 3. Nerve palpation not done due to fear of coming close to patients 4. New case detection delayed as other than fever/emergency nobody turned up |
Directly related to diagnosis of cases |
| 2 | Operational issues | 1. Lepra reaction cases were managed with steroids in spite of COVID-19 2. MDT procurement didn`t face any challenge 3. Lepra reaction/ENL patients could not attend OPD 4. Patients needing admissions were denied due to unorganized framework in the initial days 5. Release from treatment was delayed 6. Increased defaulter cases as patients migrated from the place of taking MDT 7. Government also urged that only emergency cases should attend hospitals during initial months of lockdown 8. Microcellular rubber chappal procurement faced no issues but delivery got delayed in some areas 9. Reconstructive surgery camp could not be undertaken 10. Defaulter tracking is more difficult in urban areas |
Directly related to operational issues of NLEP |
| 3 | Rehabilitation issues | 1. Patients in leprosy colony were given economic support by District initiatives 2. Employment and livelihood of leprosy patients suffered due to lockdown 3. Education of leprosy affected children came to a standstill as they didn’t have smartphones 4. ‘After school learning centre’ for leprosy affected children closed down 5. Skill centres for leprosy patients in leprosy colony were closed |
Directly related to rehabilitation |
| 4 | Capacity building | 1. No capacity building activities till November, 2020 | Directly related to training |
| 5 | Way forward | 1. Examination of patients should be carried out with proper PPE in future so that diagnosis does not get hampered 2. Tracking of defaulters should be carried out |
Directly related to issues for future |
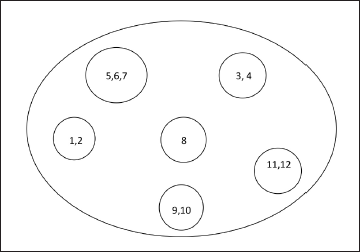
- Cognitive map with two-dimensional scaling and hierarchical cluster analysis of issues faced by health workers and leprosy patients regarding National Leprosy Eradication Programme implementation. Abbreviations: 1. Solitary focus on COVID-19 control 2. ASHA were compelled to be involved in COVID-19 related work 3. No capacity building activities in the initial days though virtual training have been started since November 2020 4. Information Education and Communication activities came to halt 5. Active case surveillance has been reduced 6. ASHA debarred from home visits 7. ASHA made phone calls to households to enquire about wellbeing 8. Several health workers got COVID-19 infection overburdening others 9. Patients in Lepra reaction needing immediate medical care could not come to hospital due to lockdown 10. Some health workers had to use own vehicles to attend to their jobs since public transport was not plying 11. Caller tunes of mobile phones can use Information Education and Communication messages regarding leprosy just like COVID-19 12. ’Namashkaram’ can be used in place of ‘Sparsh’ (touch) to remove stigma while maintaining social distancing
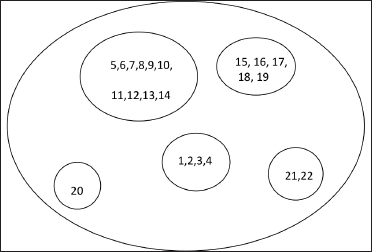
- Cognitive map with two-dimensional scaling and hierarchical cluster analysis of difficulties in National Leprosy Eradication Programme implementation reported by key respondents (programme managers and doctors). Abbreviations: 1. Histopathology and slit skin smear could not be done 2. Lepra reaction and relapse case diagnosis hampered 3. Nerve palpation not done due to fear of coming close to patients 4. New case detection delayed as other than fever/emergency nobody turned up 5. Lepra reaction cases were managed with steroids in spite of COVID-19 6. Multi drug treatment procurement didn`t face any challenge 7. Lepra reaction/ENL patients could not attend OPD 8. Patients needing admissions were denied due to unorganized framework in initial days 9. Release from treatment was delayed 10. Increased defaulter cases as patients migrated from the place of taking multi drug treatment 11. Government also urged that only emergency cases should attend hospitals during the initial months of lockdown 12. Microcellular rubber chappal procurement faced no issues but delivery got delayed in some areas 13. Reconstructive surgery camps could not be undertaken 14. Defaulter tracking is more difficult in urban areas 15. Patients in leprosy colonies were given economic support by District initiatives 16. Employment and livelihood of leprosy patients suffered due to lockdown 17. Education of leprosy affected children came to a standstill as they didn’t have smartphones 18. ‘After school learning centre’ for leprosy affected children closed down 19. Skill centres for leprosy patients in leprosy colonies were closed 20. No capacity building activities till November, 2020 21. Examination of patient should be carried out with proper PPE in future so that diagnosis does not get hampered 22. Tracking of defaulters should be carried out
Discussion
COVID-19 came as a blow to all spheres of life and the National Leprosy Eradication Programme was no exception. The National Leprosy Eradication Programme has rolled out several measures in the recent past to ensure early diagnosis, disability management and stigma alleviation; which includes “Leprosy case detection campaign (2016)”16 “Sparsh Leprosy Awareness Campaign (2018)”17 and “Active Case Detection and Regular Surveillance for Leprosy (2020).”18 National Health Mission in its directives, urged the essential health care services (Reproductive and Child health, Immunization, Tuberculosis, Leprosy, Vector borne diseases, Cancer and Dialysis) to remain uninterrupted.19 Amidst all these measures and endeavours the pandemic of COVID-19 brought everything to a standstill with the lockdown which started from 24 March, 20208 and leprosy took a back-seat considering it was a non-emergency (though essential) health-care service. The leprosy experts and the programme manager shared their experiences that during the phase of lockdown only patients with fever attended the out-patient department thus eventually the diagnosis of new cases and relapsed cases of leprosy was bound to get affected. There was scarcity of PPE kits during the initial days which led to deferring nerve palpation as well as delaying slit skin smear and histopathology in suspect cases, which further contributed to reducing case detection
The ground reality remains that in the state of West Bengal, the leprosy indicators fell sharply in the 1 two quarters (April-September 2020) compared to the previous year (2019). New leprosy case detection fell from 3433 to 1480, prevalence rate dropped from 0.64 to 0.41, and Grade I and II deformities dropped from 192 to 73 and 37 to 11 respectively.20 This sharp dip in reporting was a direct jolt to the goals and objectives of the existing programme. The ASHA and health care workers revealed that people were apprehensive about allowing household visits and thus active-surveillance as envisaged previously was difficult at grass-root level. The stigma attached to COVID-19 was a problem compounding the centuries-old stigma attached to leprosy.21 Though the ‘Sparsh Leprosy Elimination Campaign’ which aims at reducing stigma in leprosy does not actually mention that the leprosy patient needs to be touched physically, still the front-line workers felt that the word Sparsh (Hindi meaning of Sparsh being ‘Touch’) could give a wrong signal in the pandemic times with emphasis on safe distancing. They have proposed the term ‘Namashkaram’ could replace ‘Sparsh’ as the key word for the programme, the policy-makers can consider this in future. The participants in this research highlighted that during this phase of the COVID-19 pandemic the information education and communication activities regarding leprosy had come to a halt. Hence it was essential that the ‘Sapna mascot’ of National Leprosy Eradication Programme be refurbished in tune with the ongoing situation, conveying that leprosy cannot be ignored even during COVID-19 times.22 Since organising camps or raising public awareness by public announcement system/wall writing might be difficult in this period, the participants suggested utilising online-platforms, social media, television and radio to spread the message. Learning from the information education and communication for COVID-19, they suggested that caller-tunes of mobile phones can be utilised for spreading leprosy awareness. The utilisation of digital platforms also helped in revamping the capacity building activities after November 2020 and this is the way training programmes are to be managed since COVID-19 has the potential to return with more vigour with more mutant strains.
The respondents expressed their concern regarding COVID-19 becoming the sole focus of the health administration. There was manpower shortage to carry out activities related to National Leprosy Eradication Programme and this was further escalated when co-workers were affected with COVID-19. The health workers and patients alike expressed their apprehension regarding future lockdowns in the upcoming waves of COVID pandemic which might again interfere with transportation and resultant difficulties in commuting to work and even to avail healthcare services, especially during episodes of Lepra reaction. The patients shared that the ASHA workers used to call them during such periods and helped arrange medication delivery during such periods. Similar recommendations to contact the patients over phone were emphasised by leprologists from the Union territories of Dadra and Nagar Haveli.23 Healthcare workers shared their experiences regarding inability to admit patients with Lepra reactions due to the unorganised framework in the initial days. They supported the present recommendations regarding telemedicine by the government of India, and this is what lies ahead in the management of emergent serious events when physical consultation is not possible.24 The healthcare workers also instructed that they had to manage severe lepra reactions with steroids in the initial days of the epidemic despite the attendant risk of immune-suppression since they had to salvage the limb. Nowadays with more reports coming in, it has become evident that the use of steroids and/or methotrexate is not associated with untoward outcomes even in leprosy patients co-infected with COVID-19.25 The initial fear regarding immune-suppressive agents in COVID-19 was proven wrong and the guideline states that they may be used to prevent disease flares which can result in poor quality of life and sequelae, thereby increasing the need for healthcare usage26,27
Another profound problem which arose during the period of lockdown was mass migration which led to treatment interruptions since patients were not able to get the medicines in their new place of residence in the absence of referral cards. Things happened in such quick succession that National Leprosy Eradication Programme could not track the defaulters and it was expressed that tracking the defaulter was a major problem in urban areas. Thus, it becomes evident that National Leprosy Eradication Programme has to focus on these aspects so that a similar situation is not repeated. The authors would advocate providing multidrug treatment (MDT) blister pack for two-three more months instead of one month in the phase of such crisis to tide over the problem of interrupted treatment and can be a solution to tackle defaulter. This will be in tune with accompanied multi drug treatment (A-MDT). In spite of all these problems, the good thing was that the procurement of multi drug treatment as well as microcellular rubber chappals was not affected since that was done in the initial half of March 2020 before the lockdown was announced.
The management of disability was hit very badly in-spite of having optimum stocks of microcellular rubber chappals, since its delivery to the needy was impeded. More importantly, no reconstructive surgery camp could be organised since the time lockdown was imposed. Thus, it is of paramount importance that the National Leprosy Eradication Programme focuses on disability management in this difficult time, else the decades-long efforts of the ‘enhanced global strategy for further reducing the disease burden’28 and reducing disability rates will fall flat.
The socio-economic problems of persons living in leprosy colonies were immense; these impoverished individuals lost their livelihood due to lack of markets where they could sell the items prepared them and even the ‘skills centres’ were closed down. The NGOs involved in social rehabilitation expressed their concerns about the unfortunate state-of-affairs that children of leprosy families faced since they had no smartphones to attend online classes and ‘after-school learning centres’ were also closed. The humane face of the health-care service provider was highlighted by the some respondents and there were instances when economic support was rendered to patients by personal endeavour at district level. During the festive season of ‘Durga Puja’ (Local Festival), new clothes were distributed to the people in the leprosy colony which reassures us that the virus would never win over humanity.
Limitation: The research was conducted in the rural population of eastern India which has high leprosy prevalence; however, the findings might not completely reflect the problems and perceptions of healthcare workers in the low prevalence, urban regions of the country.
Conclusion
The COVID-19 pandemic has shown that the virus can mutate and stay for long, thus creating mayhem, affecting lives and livelihoods globally. Managing the pandemic is the priority but at the same time the nearly won battle against leprosy cannot be ignored. The solitary focus of the administration on COVID-19 and shifting of infrastructure and human resources towards the management of COVID-19 can lead to resurgence of leprosy. The diagnostic difficulties and management complications can be addressed by having an organised framework of operations in the healthcare setting. The front-line workers need support from the programme to provide them with transportation and protective equipment, so that they may render their services with full efficiency in. Utilising online platforms, digital and social media needs to be maximised to help in capacity building of the staff as well as for information education and communication. Rehabilitation of patients of leprosy needs to be given a serious thought by the programme. Apart from giving economic support, it will be more sustainable if they can be provided with job opportunities in small-scale industries. They could also be a source of valuable human resources for industries linked to COVID-19 management (e.g., manufacture of Personal protective equipment, etc). It needs to be emphasised that National Leprosy Eradication Programme needs to ramify itself and work out ways to address the various issues faced by patients, doctors, front-line workers, programme managers during the difficult times of the COVID-19 pandemic.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial source and support
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Impact of leprosy on the quality of life. Bull World Health Organ. 1999;77:354-6.
- [PubMed] [PubMed Central] [Google Scholar]
- Integration of leprosy elimination into primary health care in Orissa, India. PLoS One. 2009;4:e8351.
- [CrossRef] [PubMed] [Google Scholar]
- India has highest number of new leprosy patients TNN. 2010. Available at: http://timesofindia.indiatimes.com/india/India-has-highest-numberof-new-leprosy-patients/articleshow/5546725.cms Last accessed 11th May 2021
- [Google Scholar]
- National Leprosy Eradication Programme. Available at: http://nlep.nic.in/index.html accessed on 8th Decemeber, 2020. Last accessed 11th May 2021
- [Google Scholar]
- Central Leprosy Division. Directorate General of Health Services. Ministry of Health & Family Welfare. Government of India
- [Google Scholar]
- Central Leprosy Division. Directorate General of Health Services. Ministry of Health & Family Welfare. Government of India
- [Google Scholar]
- Department of Health and Family Welfare, Government of West Bengal. Available at: https://www.wbhealth.gov.in/other_files/2008/9_33.html issued on 31.03.2009 Last accessed 11th May 2021
- [Google Scholar]
- 11 March 2020. World Health Organization (WHO) (Press release). Archived from the original on March 2020
- Ministry of Home Affairs Order no 40-3/2020-D dated 24.03.2020. Available online https://www.mohfw.gov.in/pdf/Annexure_MHA.pdf Last accessed 11th May 2021
- The focus group manual: Methods for social research in disease. Boston: International Nutrition Foundation for Developing Countries (INFDC); 1993.
- [Google Scholar]
- The preponderance of negative emotion words in the emotion lexicon: A cross-generational and cross-linguistic study. J Multiling Multicult Dev. 2004;25:266-84.
- [CrossRef] [Google Scholar]
- Farmers’ suicides in the Vidarbha region of Maharashtra India: A qualitative exploration of their causes. J Inj Violence Res. 2012;4:2-6.
- [CrossRef] [PubMed] [Google Scholar]
- Salience counts - and so does accuracy: Correcting and updating a measure for free-list-item salience. J Linguist Anthr. 1997;7:208-9.
- [CrossRef] [Google Scholar]
- (2003) Version 1.0: Analytic Technologies
- A qualitative study of perceptions about voluntary blood donation among the supportive service employees of a multispecialty rural tertiary care hospital. National Journal of Community Medicine. 2012;3:310-5.
- [Google Scholar]
- A review of multidimensional scaling (MDS) and its utility in various psychological domains. Tutorials in Quantitative Methods for Psychology. 2009;5:1-10.
- [CrossRef] [Google Scholar]
- Leprosy case detection campaign (LCDC) for active surveillance. Trop Doct. 2018;48:72-73.
- [CrossRef] [PubMed] [Google Scholar]
- National Leprosy Eradication programme. Central leprosy division. Directorate general of heath services. Ministry of health and famiy welfare. Governement of India. Available from: https://jknhm.com/pdf/gui7-15.pdf Last accessed 11th May 2021
- [Google Scholar]
- National Leprosy Eradication programme. Central leprosy division. Directorate general of heath services. Ministry of health and famiy welfare. Governement of India. Available from: https://alertindia.org/wp-content/uploads/2020/10/2020-Operational-Guidelines-for-ACD-and-RS-NLEP-.pdf Last accessed 11th May 2021
- [Google Scholar]
- National health Mission. Ministry of Health and Family Welfare. Government of India. Available at: https://nhm.gov.in/index1.php?lang=1&level=1&sublinkid=1339&lid=720 Last accessed 11th May 2021
- [Google Scholar]
- WB MPR for the month of September 2019. NLEP wing. Swastha Bhavan. Government of West Bengal
- Government of India initiative against leprosy-We should be aware. J Family Med Prim Care. 2019;8:3072-73.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 and leprosy-hurdles and possible solutions. Asian Pac J Trop Med. 2020;13:472-3.
- [CrossRef] [Google Scholar]
- Appendix 5 of the Indian Medical Council (Professional Conduct, Etiquette and Ethics Regulation. 2002. 25 March 2020. Available at https://www.mohfw.gov.in/pdf/Telemedicine.pdf Last accessed 11th May 2021
- [Google Scholar]
- Severe type 2 leprosy reaction with COVID-19 with a favourable outcome despite continued use of corticosteroids and methotrexate and a hypothesis on the possible immunological consequences. Int J Infect Dis. 2021;103:549-51.
- [CrossRef] [PubMed] [Google Scholar]
- Use of immunosuppressants/ immunomodulators in autoimmune/inflammatory dermatologic diseases during COVID-19 pandemic-general recommendation based on available evidence. Indian Dermatol Online J. 2020;11:526-33.
- [CrossRef] [PubMed] [Google Scholar]
- 2009. World Health Organization. Available at http://apps.who.int/iris/bitstream/handle/10665/205003/B4322.pdf;jsessionid=8CC82C5F63A33D68EDCD1570FE362F31?sequence=1 Last accessed 11th May 2021






