Translate this page into:
Bilateral verruciform lesions: A new CHILD syndrome presentation
Corresponding author: Dr. Yiqun Jiang, 12 Jiangwangmiao Street, Nanjing 210042, Jiangsu Province, China. yiqunjiang@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Zeng R, Yang X, Lin L, Jiang Y. Bilateral verruciform lesions: A new CHILD syndrome presentation. Indian J Dermatol Venereol Leprol 2023;89:497-8.
Dear Editor,
CHILD syndrome (congenital hemidyplasia with ichthyosiform nevus and limb defects syndrome) is a rare X-linked dominant disorder which is lethal in hemizygous males. Unilateral congenital hemidysplasia with ichthyosiform erythroderma and ipsilateral limb defects characterize this condition. A large proportion of patients with this condition have unilateral ichthyosiform erythroderma lesions, with a few having verrucous xanthoma-like symptoms. A rare case of CHILD syndrome with bilateral verruciform lesions is described.
A 30-year-old Chinese woman presented with keratotic papules on her left and right extremities which had been present since birth. Following a Blaschko linear distribution, the skin lesions had steadily increased with age. Lesions appeared on the left jaw as well. In addition, the left leg and spine of the patient were shorter than the right. There were no signs of cognitive impairment in the patient. There were no other serious diseases in the past. Ten years ago, patient had a bacterial infection of the skin lesions over the left ankle joint which was treated surgically leaving behind scars. There was nothing significant in the family history.
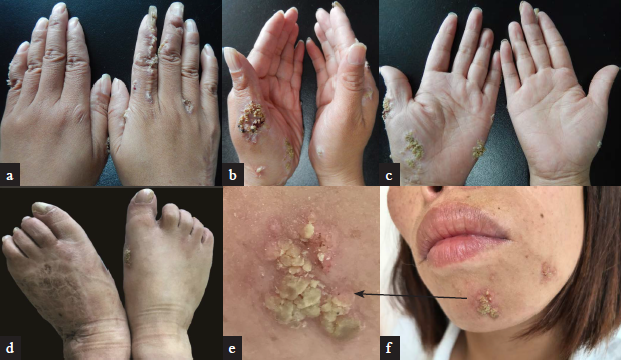
The patient was 130 cm tall and weighed 36 kg. Her left lower limb was shorter than her right one. Dermatological examination revealed verruciform lesions over the left mandible and bilaterally over hands and feet [Figure 1]. Hyperkeratosis and parakeratosis in the epidermis, as well as dense histiocytic infiltrates and foamy cells in the dermis were found on histopathological examination [Figure 2]. The routineblood and urine tests revealed nothing unusual. X-ray examination of spine showed scoliosis to the left [Figure 3]. The left tibia was shorter and thinner than the right, and fifth toe on the left foot was missing (white arrow).
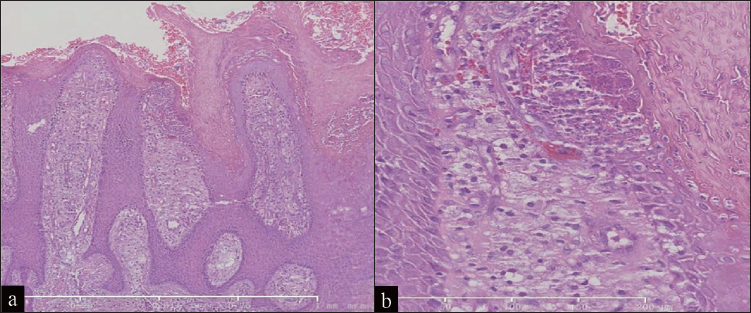
- Histopathological examination revealed epidermis hyperkeratosis and parakeratosis, as well as dense histiocytic infiltrates and foamy cells in the dermis (a, haematoxylin and eosin,×25; b, haeamtoxylin and eosin,×200)
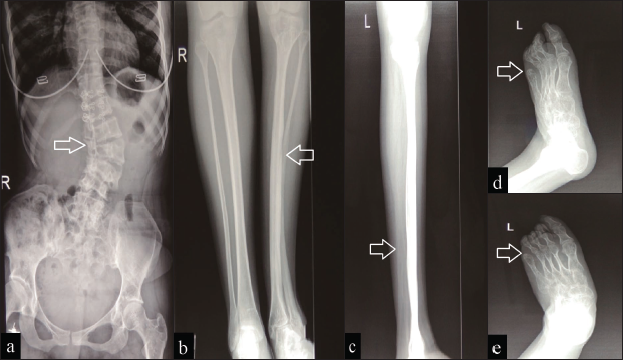
- An X-ray examination revealed that the spine was twisted to the left. The left tibia was shorter and thinner than the right tibia, and the fifth toe was missing
Genetic sequencing revealed c.766C>T nonsense mutations in the nicotinamide adenine dinucleotide phosphate-dependent steroid dehydrogenase-like genes. This was linked to the dependent steroid dehydrogenase-like gene’s p.R256X amino acids, which hindered protein activity. Gene sequencing of the enhancer-binding proteins produced negative results. The patient was diagnosed with CHILD syndrome based on her clinical symptoms and gene alterations.
Happle and colleagues initially characterized the CHILD syndrome in 1980.1 The right side of the body is usually affected by CHILD syndrome lesions. On the right side of the body, almost two-thirds of patients have a clear midline delineation. Right-sided lesions affect about a third of the patients.2 There have only been two occurrences of bilateral involvement documented.3,4 More than 60 patients with CHILD syndrome have been previously reported, but only 12 of them had verruciform lesions. The remaining patients had ichthyosiform erythroderma. Our patient did not have erythematous lesion. To the best of our knowledge, our patient might be the first case of CHILD syndrome to develop bilateral verrucous lesions.
The clinical history, histopathology and congenital history can help distinguish CHILD syndrome from other similar conditions. A histopathological examination should be used to differentiate the verruciform lesions of CHILD syndrome from other linear keratinized diseases, such as inflammatory linear verrucous epidermal nevus. CHILD syndrome has histopathological findings that are similar to xanthomatous diseases. Hence it should be distinguished from conditions like Simple verrucous xanthoma, clinically. Furthermore, some congenital skin diseases with bone dysplasia have clinical manifestations similar to CHILD syndrome.Hence, histopathological examination and genetic screening should be performed to rule out conditions like X-linked dominant chondrodysplasia punctata type 2, which is an X-linked dominant disorder caused by mutations in the gene encoding enhancer-binding proteins.5
There is currently no specific treatment for CHILD syndrome. Verruciform lesions are treated in the same way as that of ichthyosis, with topical application of keratolytics, lubricants, and corticosteroids. These methods only provide temporary relief from dermatologic symptoms, have limited therapeutic efficacy and are often poorly tolerated by patients. Based on the abnormal lipid metabolism in the pathogenesis, there are a few reports of successful treatment of skin lesions of CHILD syndrome with simvastatin ointment. However, the efficacy and safety of these drugs are yet to be confirmed in larger clinical trials. It has been found that verruciform lesions in CHILD syndrome have a favorable prognosis. Malignant tumors were not found in any of the 12 previously reported cases.
The phenotype and genotype of this disease were not found to be correlated in the literature. Our patient’s dependent steroid dehydrogenase-like gene had a c.766C > T (p.R256X) mutation in exon8. Only one of the previously discovered mutation sites agreed with our findings, but this patient had ichthyosiform erythroderma lesions on the left side.6 This Hence it is assumed that a link between the site of gene mutation and phenotype is unlikely.
While genetic testing accurately diagnosed the disease, clinical manifestations vary greatly, making it difficult to choose which gene to screen. Our case serves as a reminder to clinicians to test for the dependent steroid dehydrogenase-like gene in patients who have congenital bilateral verruciform lesions.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The CHILD syndrome. Congenital hemidysplasia with ichthyosiform erythroderma and limb defects. Eur J Pediatr. 1980;134:27-33.
- [CrossRef] [PubMed] [Google Scholar]
- CHILD syndrome: Case report of a Chinese patient and literature review of the NAD[P]H steroid dehydrogenase-like protein gene mutation. Pediatr Dermatol. 2015;32:e277-82.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital hemidysplasia with ichthyosiform naevus and limb defects (CHILD) syndrome without hemidysplasia. Br J Dermatol. 2015;173:304-7.
- [CrossRef] [PubMed] [Google Scholar]
- A novel missense mutation of NSDHL in an unusual case of CHILD syndrome showing bilateral, almost symmetric involvement. J Am Acad Dermatol. 2002;46:594-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mutations in the gene encoding 3 beta-hydroxysteroid-delta 8, delta 7-isomerase cause X-linked dominant Conradi-Hünermann syndrome. Nat Genet. 1999;22:291-4.
- [CrossRef] [PubMed] [Google Scholar]
- Left-sided CHILD syndrome caused by a nonsense mutation in exon 7 of the NSDHL gene. Eur J Dermatol. 2010;20:634-5.
- [CrossRef] [PubMed] [Google Scholar]