Translate this page into:
Comparative efficacy and safety of six photoelectric therapies for the atrophic acne scars: A network meta-analysis
Corresponding author: Fengchuan Zhang, Department of Dermatology, Dongfang Hospital of Beijing University of Chinese Medicine, Beijing, China. fengchuanzhang@163.com
-
Received: ,
Accepted: ,
How to cite this article: Wang Y, Sun Z, Cai L, Zhang F. Comparative efficacy and safety of six photoelectric therapies for the atrophic acne scars: A network meta-analysis. Indian J Dermatol Venereol Leprol 2023;89:353-62.
Abstract
Objectives
This network meta-analysis assessed the relative efficacy and safety of six common photoelectric therapies including 1064-nm neodymium-doped yttrium aluminum garnet (Nd: YAG), fractional carbon dioxide laser(FSCO2), fractional micro-plasma radiofrequency(Plasma), micro-needling fractional radiofrequency (MRF), 1550nm or 1540nm erbium-glass non-ablative fractional laser (NAFL) fractional erbium-doped yttrium aluminum garnet (Er: YAG).
Methods
A comprehensive search to identify relevant studies was conducted using four electronic databases. Outcome measures were extracted based on subjective and objective indexes, including the dermatologists’ evaluation(DE), the patients’ overall satisfaction(PS), VAS score, and Postinflammatory hyperpigmentation (PIH).
Results
Eleven published clinical research studies, involving 405 patients were included in this study. Ranking of DE from large to small is as follows: Nd: YAG, FSCO2, Er: YAG, Plasma, NAFL, MRF. In terms of PS, the rand from high to low can be described as follows: Er: YAG, Nd: YAG, FSCO2, Plasma, NAFL, MRF. In connection with the sequencing of adverse events, pain severity from slight to severe as follows: Er:YAG, Nd:YAG, FSCO2, NAFL, MRF, Plasma. The probability of having PIH are presented in order from lowest to highest as follows: MRF, Plasma, Nd: YAG, NAFL, Er: YAG, FSCO2.
Conclusion
FSCO2 remains the mainstream of potentially curative treatment, then again Nd: YAG and Er: YAG require greater efforts to prove their superior effectiveness. NAFL might be appropriate for mild and moderate improvement with its strengths of good tolerance while Plasma fits into patients with higher pain thresholds but an expectation of higher results. MRF has not given expression on absolute predominance for the present.
Registration
PROSPERO CRD42021242160
(available from https://www.crd.york.ac.uk/prospero).
Keywords
Meta-analysis
acne scar
laser
radiofrequency
randomised controlled trial
Plain Language Summary
Acne vulgaris is the most common dermatological disorder worldwide. Acne scars cause anxiety and embarrassment to the patients, all of which affect the quality of life. The investigators of this article are from China. This network meta-analysis assessed the relative efficacy and safety of six common photoelectric therapies including 1064-nm neodymium-doped yttrium aluminum garnet (Nd: YAG), fractional carbon dioxide laser(FSCO2), fractional micro-plasma radiofrequency(Plasma), micro-needling fractional radiofrequency (MRF), and 1550nm or 1540nm erbium-glass non-ablative fractional laser (NAFL) fractional erbium-doped yttrium aluminum garnet (Er: YAG). Eleven published clinical research studies, involving 405 patients from Asia and Africa were included in this study.We conclude that fractional carbon dioxide laser remains the major potentially curative treatment, followed by Nd: YAG and Er: YAG. Erbium-glass non-ablative fractional laser might be appropriate for mild and moderate improvement with good tolerance while fractional micro-plasma radiofrequency fits patients with higher pain thresholds but having an expectation of higher results. Microneedling fractional radiofrequency has not given expression on absolute predominance in the present study.
Introduction
Acne vulgaris is a common chronic inflammatory disease of the skin. Even after definitive treatment, there is a high probability of occurrence of acne scars. Among them, atrophic acne scars are more common than keloids and hypertrophic scars.1 Acne scars not only decrease facial attractiveness but also cause anxiety and embarrassment to the patients, all of which affect the quality of life.2 Therefore, atrophic acne scars must be treated at an early stage with an effective treatment. Currently used treatment methods such as dermabrasion, chemical peeling, hypodermic injection, dermal filler, dermal grafting and trephination have limited efficacy with adverse effects. The recent decades have seen a growing trend toward use of photoelectric therapies such as lasers and radiofrequency. Furthermore, advances in technology and technique have allowed photoelectric therapies to be applied to an ever-increasing number of acne scars.3 Lasers appear to function mainly through selective photothermal action and radiofrequency use of electromagnetic waves to generate electricity, which can all result in collagen contracture and new collagen formation.4,5 Among them, lasers can be divided into fractional ablative lasers and non-ablative lasers, the former effect seems stronger than the latter but the latter has shorter downtime and fewer side effects.6 Radiofrequency appears to achieve good results but it may cause significant pain and discomfort.7 So far, there has been little discussion about the comparative efficacy and safety of different photoelectric therapies. There is a paucity of empirical research because few head-to-head comparison studies are available and traditional pairwise meta-analysis cannot integrate all of the evidence from several comparators. Hence, this research project has been aimed to assess the relative efficacy and safety of six common photoelectric therapies including 1064-nm neodymium-doped yttrium aluminium garnet, fractional carbon dioxide laser, fractional micro-plasma radiofrequency (plasma), micro-needling fractional radiofrequency, 1550 nm or 1540 nm erbium-glass non-ablative fractional laser and fractional erbium-doped yttrium aluminium garnet using a network meta-analysis design.
In this study, we tabulate previously published data, using subjective rating procedures including the dermatologists’ evaluation of the treatment efficacy greater than 50% improvement, the patients’ overall satisfaction in the improvement of atrophic acne scars greater than or equal to “moderately satisfied” and VAS score (a 10-point visual analog scale, 0 = no pain and 10 = worst pain ever). Post-inflammatory hyperpigmentation was selected as the objective measurement for the evaluation of postoperative complications.
Methods
We performed a network meta-analysis following an a priori established study protocol (available on request). The study protocol is registered with PROSPERO (Registration No CRD42021242160).
Inclusion criteria
Types of patients: (1) presence of atrophic acne scars on the face, (2) willingness to follow up and comply with the study protocol. The exclusion criteria were as follows: (1) having active acne under treatment, (2) pregnancy, (3) mental illness, (4) active dermatitis or bacterial infection on the face and (5) having received any other treatments for acne scars for six months before the first treatment.
Types of interventions and control: (1) 1064-nm neodymium-doped yttrium aluminium garnet, (2) fractional carbon dioxide laser, (3) fractional micro-plasma radiofrequency (plasma), (4) micro-needling fractional radiofrequency, (5) non-ablative fractional laser, (6) fractional erbium-doped yttrium aluminium garnet and (7) blank control or placebo.
Types of outcome measures: (1) The number of patients with a clinical improvement greater than 50% in skin texture and atrophy evaluated by dermatologists. (2) The number of patients with an overall satisfaction greater than or equal to “moderately satisfied.” (3) VAS score (a 10-point visual analogue scale, 0 = no pain and 10 = worst pain ever). (4) The number of patients with post-inflammatory hyperpigmentation.
Types of studies: All reports included in this study were clinical randomised controlled trials.
Literature search
The studies selected in this network meta-analysis were obtained from the PubMed, Web of Science, EMBASE and Cochrane Library databases (up to May 31, 2021). The search strategy was as follows: [acne scar] or [acne scarring] or [atrophic scarring], [laser] or [lasers] or [radiofrequency], and [RCT] or [randomised controlled trial]. The reference lists of included manuscripts were reviewed in search of sources that may have been missed.
Data extraction
Two researchers independently screened titles and abstracts and selected references. The information and data extraction which included first author, year of publication, the country in which the trial was conducted, patient sample size, study design, mean age of patients, type of laser or radiofrequency, therapy mode of laser or radiofrequency, the time interval between treatment, number of sessions, follow-up time, adverse reactions and complications. Efficacy assessment outcomes included dermatologists’ evaluation and patients’ overall satisfaction. Safety outcomes included VAS score and post-inflammatory hyperpigmentation.
Assessment of risk of bias
Two authors independently grade the quality of each original study using the Cochrane Collaboration tool, which is widely used in quality assessment. The quality of the literature was assessed independently by two authors and discrepancies were reviewed by a third author.
Statistical analysis
All statistical analyses were performed using STATA software (Version 15.1; STATA. Corp, College Station, Tex). For confidence intervals (e.g., number of patients with clinical improvement, overall satisfaction and post-inflammatory hyperpigmentation), calculated the relative risk (RR) with 95% confidence intervals (95% confidence interval). The P-value for the overall effect was judged using the Z test, with a significance set of P < 0.05.8 Heterogeneity was tested using the I2 test, with I2>50% suggesting the existence of heterogeneity. A fixed-effects model was used when I2<50%, otherwise, a random-effects model was used.9,10 Statistically significant was determined as a P-value < 0.05. The inconsistency model was mainly used to examine the degree of inconsistency between direct comparison evidence and indirect comparison evidence.11 At the same time, a network relationship diagram and predictive interval plot of various interventions were drawn. The former can effectively demonstrate the interdependencies among criterias, indirect comparison relationship and the latter can illustrate the summary effect size of the comparative effectiveness among interventions.12 Additionally, funnel plots were used to assess bias, which would be visually examined for asymmetry.13 In this study, to rank the intervention effects, the cumulative ranking probability curve (surface under the cumulative ranking area) of each treatment scheme would be estimated. Greater surface under the cumulative ranking area values were probability indicative of better intervention.14
Results
Literature search
A total of 878 articles were identified through database searching, from which 514 were screened after excluding duplicates. 162 studies were evaluated by browsing the full-text, 11 of these met the inclusion criteria in this network meta-analysis. Most of the included studies were from Asia so most patients approximately had the same Fitzpatrick skin type (III or Iv). Furthermore, the severity of acne scars was mostly from mild to severe and the type of scars was mostly a combination of two or three types. Moreover, the frequency of treatment was predominantly 3-4 sessions at 3-4 weeks intervals and the duration of follow-up varied between three to six months. The flow chart of literature screening and review is outlined in Figure 1.

- Flowchart of literature screening
Study characteristics and risk of bias
405 patients were included in 11 studies included in this meta-analysis and were of approximately equal representation of sex (184 males and 189 females). All of them came from an Asian background, such as China, Korea, Thailand, etc. All studies were published between 2010 and 2020. Four of 11 randomised controlled trials separated patients into two groups of equal numbers, others were split-face studies. Six types of photoelectric therapies, including neodymium-doped yttrium aluminium garnet, fractional carbon dioxide laser, plasma, micro-needling fractional radiofrequency, non-ablative fractional laser and erbium-doped yttrium aluminium garnet were included in 11 studies. The clinical and demographic characteristics and the treatment options of participants are displayed in Table 1. Details of the risk of bias summary and risk of bias graph are shown in Figure 2.
| Study | Country | Design | Age (year) | Male | Female | Total | Fitzpatrick skin type | Follow-up time (month) | Intervention group | Control group | Number of applications | Intervals (week) | Primary outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sirithanabadeekul, 202015 | Thailand | RCT (split-face) |
28.9 ± 4.8 | 13 | 12 | 25 | IIΙ28%, IV68%, V4% | 1, 3 | Nd:YAG | FSCO2 | NR | NR | DE, PS, VAS, PIH |
| Lan, 202016 | China | RCT (split-face) |
22.87 ± 2.51 | 39 | 21 | 60 | III41.67%, IV58.33% | 1, 3, 6 | Plasma | MRF | 3 | 8 | DE, PS, VAS, PIH |
| Kwon, 202017 | Korea | RCT (split-face) |
NR | 11 | 14 | 25 | NR | 2 | Nd:YAG | NAFL | 4 | 3 | DE, PS, VAS, PIH |
| Chayavichitsilp, 202018 | Thailand | RCT (split-face) |
30.4 ± 6.8 | 16 | 14 | 30 | III90%, IV10% | 4, 8 | Nd:YAG | NAFL | 4 | 4 | VAS, PIH |
| Al-Sultany, 202019 | Iraq | RCT (random groups) |
36(20-48) | 12 | 30 | 42 | II23.8%, III35.7%,IV30.95%, V9.55% | 2 | FSCO2 | MRF | 4 | 4 | DE |
| Elsaie, 201820 | Egypt | RCT (random groups) |
NR | 19 | 39 | 58 | NR | 3 | FSCO2 | NAFL | 4 | 3 | DE, PS, VAS, PIH |
| Chae, 201521 | Korea | RCT (random groups) |
26.9 | 29 | 11 | 40 | III17.5%, IV70%, V12.5% | NR | NAFL | MRF | 3 | 4 | DE, PS, VAS, PIH |
| Zhang, 201322 | China | RCT (split-face) |
26.4 ± 3.7 | 19 | 14 | 33 | III and IV | 6 | FSCO2 | MRF | 3 | 8 | PS, VAS, PIH |
| Manuskiatti, 201323 | Thailand | RCT (split-face) |
29.5 | 8 | 12 | 20 | NR | 1, 3, 6 | Er:YAG | FSCO2 | NR | NR | DE, PS, VAS, PIH |
| Asilian, 201124 | Iran | RCT (random groups) |
26.6 | 10 | 22 | 64 | NR | 3, 6 | Nd:YAG | FSCO2 | 4 | 4 | DE, PS, PIH |
| Cho, 201025 | Korea | RCT (split-face) |
NR | 8 | 0 | 8 | NR | 3 | NAFL | FSCO2 | NR | NR | DE, PS, VAS, PIH |
NR: not reported, Values are expressed as mean ± standard deviation or median (interquartile range)
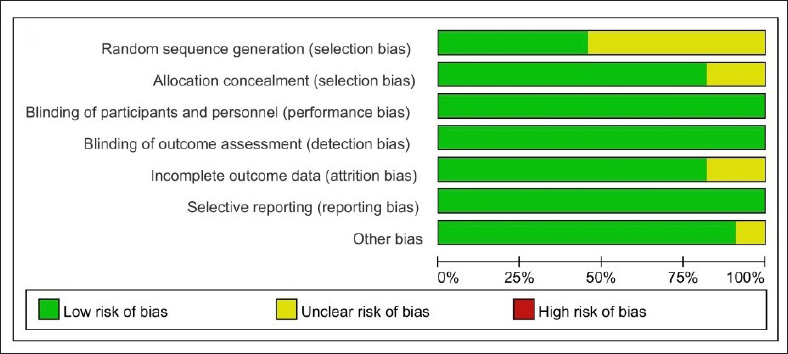
- Risk of bias graph
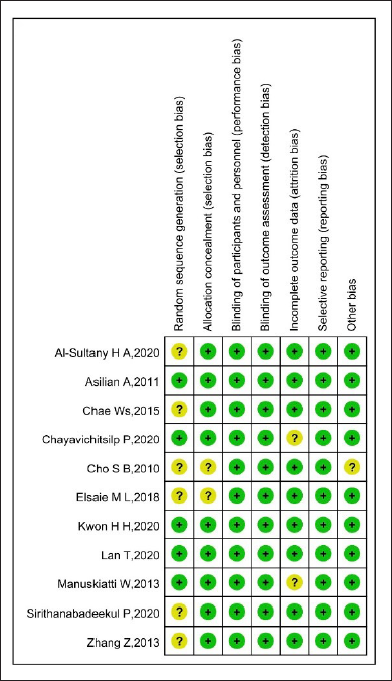
- Risk of bias summary. Green colour: Low risk of bias; red colour: High risk of bias; yellow colour: Unclear risk of bias
Evidence network
The set of direct comparison evidence between treatments (network geometry) is illustrated by the network evidence graph (Figure 3). The directly compared interventions are linked with a line, the thickness of which is proportional to the number of studies assessing the comparisons. Each round dot represents one intervention. The larger the area of a dot, the greater the overall sample size of each intervention. In this context, fractional carbon dioxide laser has the greatest number of studies, sample size, and direct comparison, conversely, plasma harbours the least number of them.
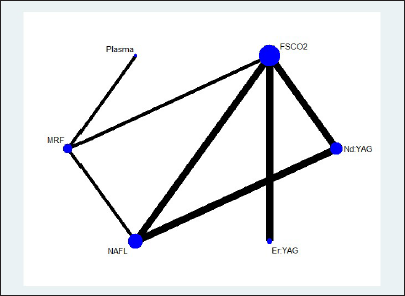
- Schematic of the network of evidence used in network meta-analysis
Consistency test
Logistic regression analysis was used to assess total concordance. Post-inflammatory hyperpigmentation, dermatologists’ evaluation and patients’ overall satisfaction did not show inconsistency (Prob of post-inflammatory hyperpigmentation = 0.6402>0.05, Prob of dermatologists’ evaluation = 0.8967>0.05, Prob of patients’ overall satisfaction = 0.7444>0.05), while VAS score shows a certain inconsistency (Prob> chi2 = 0.0000<0.05). Subsequently, we applied local consistency between direct and indirect evidence by a loop-specific approach. Likewise, post-inflammatory hyperpigmentation (fractional carbon dioxide laser-plasma-micro-needling fractional radiofrequency-non-ablative fractional laser ROR = 7.805, 95% confidence interval 1.00,2381.91; Nd:YAG-fractional carbon dioxide laser-non-ablative fractional laser ROR = 2.498, 95% confidence interval 1.00, 72.02), dermatologists’ evaluation (fractional carbon dioxide laser-micro-needling fractional radiofrequency-non-ablative fractional laser ROR = 1.557, 95% confidence interval 1.00,12.52; Nd:YAG-fractional carbon dioxide laser-non-ablative fractional laser ROR = 1.158, 95% confidence interval 1.00, 6.44) and patients’ overall satisfaction (fractional carbon dioxide laser-plasma-micro-needling fractional radiofrequency-non-ablative fractional laser ROR = 3.434, 95% confidence interval 1.00, 28.02; Nd:YAG-fractional carbon dioxide laser-non-ablative fractional laser ROR = 1.056, 95% confidence interval 1.00, 24.43) exhibits local consistency whereas VAS score shows a certain local inconsistency (fractional carbon dioxide laser-plasma- micro-needling fractional radiofrequency -non-ablative fractional laser 95% confidence interval 1.29,3.35; Nd:YAG-fractional carbon dioxide laser-non-ablative fractional laser 95% confidence interval 0.34, 2.07). The inconsistency analysis showed that the P-value only between fractional carbon dioxide laser and non-ablative fractional laser is 0.000 <0.05, while other P values of pairwise comparisons are all greater than 0.05 [Table 2]. This inconsistency is discussed in more detail later. In like manner, funnel plots for the dermatologists’ evaluation, patients’ overall satisfaction and post-inflammatory hyperpigmentation status were roughly symmetrical, nevertheless, fractional carbon dioxide laser vs non-ablative fractional laser in VAS indicates the presence of publication bias (Figure 4).
| Side | Direct | Indirect | Difference | ||||
|---|---|---|---|---|---|---|---|
| Coef. | Std. err. | Coef. | Std. err. | Coef. | Std. err. | P > z | |
| A B | −0.4051 | 0.94163 | 1.79443 | 1.14719 | −2.1996 | 1.48416 | 0.138 |
| A E | 0.91129 | 0.94556 | −1.2883 | 1.14397 | 2.19957 | 1.48417 | 0.138 |
| B C | 0.9863 | 1.16771 | −0.8775 | 1.82285 | 1.86376 | 2.16479 | 0.389 |
| B E | −1.1818 | 0.25483 | 1.23783 | 0.30751 | −2.4196 | 0.39938 | 0 |
| B F | . | . | . | . | . | . | . |
| C D | −0.6096 | 1.15329 | −2.4734 | 1.83203 | 1.86378 | 2.16481 | 0.389 |
| D E | 0.76385 | 1.18465 | −1.0999 | 1.8119 | 1.86379 | 2.1648 | 0.389 |
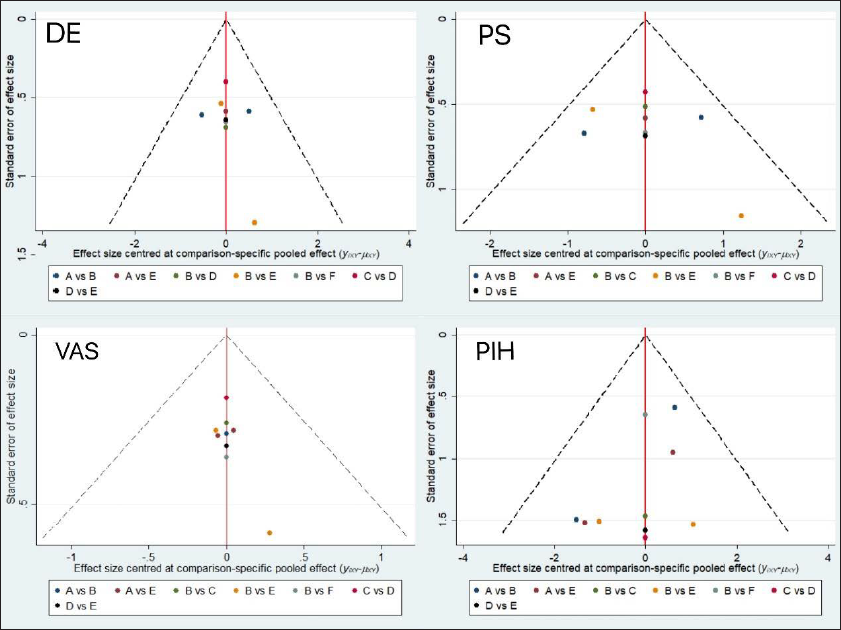
- Funnel plot for the meta-analysis
Meta-Analysis
1. Pairwise comparisons
The limits of the 95% credible interval and prediction interval have been drawn, respectively in red and blue. The short black horizontal or rhombus intersected with the midcourt line, which means no significant difference. As can be seen from Figure 5, from the dermatologists’ evaluation perspective, micro-needling fractional radiofrequency has a less pronounced effect than neodymium-doped yttrium aluminium garnet, fractional carbon dioxide laser, and plasma. Non-ablative fractional laser has a less pronounced effect than neodymium-doped yttrium aluminium garnet and fractional carbon dioxide laser. From a patients’ overall satisfaction perspective, there is no significant difference among different treatment options. Concerning VAS, fractional carbon dioxide laser and non-ablative fractional laser have greater pain intensity than neodymium-doped yttrium aluminium garnet. Plasma and micro-needling fractional radiofrequency have greater pain intensity than erbium-doped yttrium aluminium garnet. With regard to post-inflammatory hyperpigmentation, the chances with plasma or micro-needling fractional radiofrequency is less than fractional carbon dioxide laser.
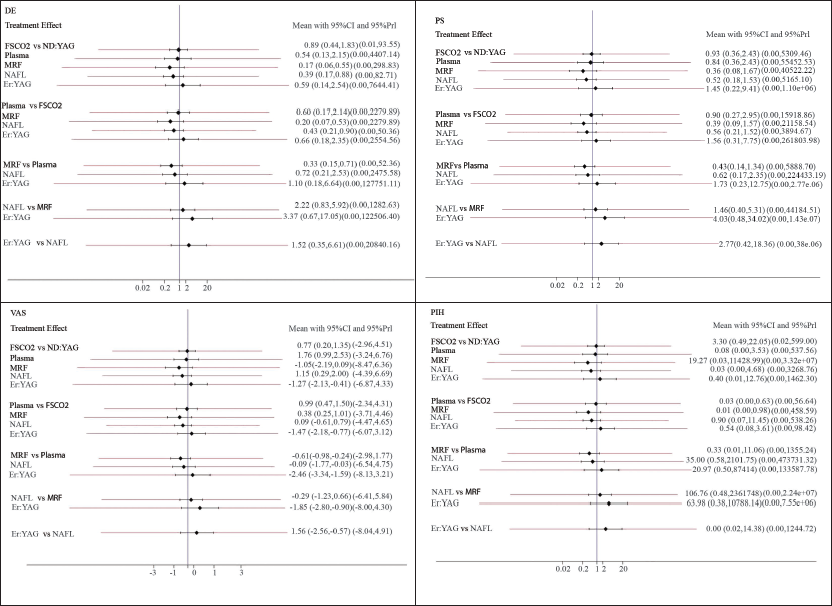
- Statistically significant pairwise comparisons
2. Comprehensive comparisons
As can be seen in Figure 6, cumulative probability plots of four individual indicators are presented. The surface under the cumulative ranking area probabilities of dermatologists’ evaluation from large to small are as follows: neodymium-doped yttrium aluminium garnet (83.6%), fractional carbon dioxide laser (78.0%), erbium-doped yttrium aluminium garnet (53.6%), plasma (51.4%), non-ablative fractional laser (30.9), micro-needling fractional radiofrequency (2.5%). In terms of patients’ overall satisfaction, the rand from high to low can be described as follows: erbium-doped yttrium aluminium garnet (76.4%), neodymium-doped yttrium aluminium garnet (65.5%), fractional carbon dioxide laser (61.9%), plasma (57.0%), non-ablative fractional laser (25.5%) and micro-needling fractional radiofrequency (12.7%). With regards to adverse events, pain severity from slight to severe was as follows: erbium-doped yttrium aluminium garnet (98.4%), neodymium-doped yttrium aluminium garnet (81.5%), fractional carbon dioxide laser (48.2%), non-ablative fractional laser (44.6%), micro-needling fractional radiofrequency (27.0%), plasma (0.3%). The probability of having post-inflammatory hyperpigmentation is presented in order from lowest to highest as follows: micro-needling fractional radiofrequency (87.3%), plasma (83.0%), neodymium-doped yttrium aluminium garnet (54.4%), non-ablative fractional laser (32.8%), erbium-doped yttrium aluminium garnet (32.6%), fractional carbon dioxide laser (9.9%).
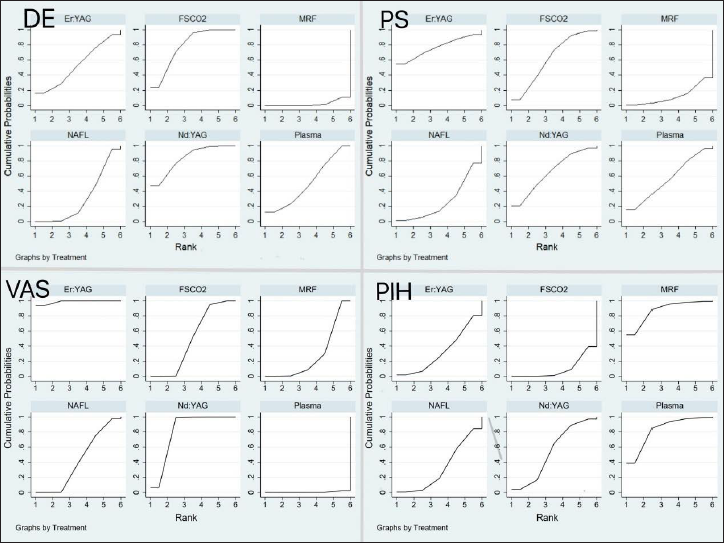
- Cumulative probability plots
Discussion
Most of the previous review articles on acne scars were on non-laser-based approaches such as chemical reconstruction etc. or comparison with two laser modalities.6,15 Because of the lack of uniformity in the data, it was not possible to perform meta-analyses or network meta-analyses. Based upon our clinical experience and reading of the literature, 6 commonly used photoelectric therapeutics in clinical settings were included in this study. To our knowledge, this study is the first report about the comparative efficacy and safety of these several photoelectric approaches. They can be further subdivided into fractional ablative laser (fractional carbon dioxide laser, erbium-doped yttrium aluminium garnet), non-ablative laser (neodymium-doped yttrium aluminium garnet, non-ablative fractional laser), and radiofrequency (plasma, micro-needling fractional radiofrequency). In the first place, fractional ablative laser and non-ablative laser can both induce normal skin tissue surrounding acne scars to initiate the wound repair response, and the collagen tissue in the dermis will constrict immediately, playing a pivotal role in skin remodelling.16 In practice, however, they have different therapeutic rationales and side effects. The fractional ablative laser is dehydrates the skin, producing limited thermally damaged zones.17 There were postoperative oblong scab skin formations to regenerate the damaged skin.18 Moreover, a desirable characteristic of the non-ablative laser is the energy concentration in the deep dermis without damaging the epidermis, which does not form crusts, and with no downtime.19 The microplasma radiofrequency can excite the nitrogen between the probe and the skin into the microplasma state, and then establish multiple controllable micropillars with thermal penetration on the skin tissue. Next, the surrounding water molecules can have high-speed rotating friction, thus promoting skin surface reconstruction and collagen recovery.20 Finally, microneedle radiofrequency is a new type of phased radiofrequency with the principle of simulating lattice mode models, which can generate thermal energy released by microneedle, thereby heating the dermis and stimulating the neogenesis of collagen without affecting the epidermis.21
All the studies had low risk in performance, detection, and reporting bias, while half of them had unclear risk of selection bias because their reports did not mention specific procedures of random sequence generation. A few of them did not mention allocation concealment either. We need to highlight that it is hard to implement blinding for treating physicians because of the human manipulation of photoelectric instruments. However, we think this situation has no direct effect on the outcome data. In addition, the lost follow-up rates of the two studies were 10% (NO.4) and 20% (NO.9). Although these authors have reported that most of the lost follow-up participants have scheduling conflicts, we judge them as unclear risk of bias with no provision of proper substitution proposal and no definite impact on outcome data.
Concerning the number of studies and the sample size included in our research, fractional carbon dioxide laser and non-ablative fractional laser have the largest proportion, followed by neodymium-doped yttrium aluminium garnet and erbium-doped yttrium aluminium garnet, while two radiofrequency therapies rank last. A novel principle of “fractional photothermolysis” was proposed early in 2004, which allowed fractional lasers such as fractional carbon dioxide laser and non-ablative fractional laser to be widely used for many years.22 In more recent years, a newer technology of radiofrequency has been found but have not been used in the majority of medical institutions, so there are not many studies on radiofrequency.23
According to our result on the consistency test and publication bias, the VAS score seems to lack consistency, which is specifically manifested by fractional carbon dioxide laser vs non-ablative fractional laser. We searched the source of heterogeneity. We found two studies (NO1 and NO11) with potential source of heterogeneity because of their excessive gap between VAS scores of fractional carbon dioxide laser. Sirithanabadeekul et al. referred to the very conservative treatment setting for the fractional CO2 laser they used, which had a fixed pulse duration and a depth of penetration of about 350-400 μm. However, other studies applying fractional carbon dioxide laser used Deep FX which had a penetration of about 1000 μm or even deeper depth, and thus patients in this study would naturally have less pain. Cho et al. mentioned that their comparison was not conclusive due to the small study sample (only 8 patients) and only male patients.
Based upon the primary outcome measure of efficacy, results obtained from surface under the cumulative ranking area rankings and pairwise comparison of dermatologists’ evaluation were all consistent. Nevertheless, there is no significant difference in the pairwise comparison of patients’ overall satisfaction among all treatments. We conclude that the possible reasons for this situation could be that half of the studies were split-face designs which may produce similar feelings between two sides of the face. Frequently, several sessions of treatment are required for acne scars,24 which makes patients not sensitive enough to identify subtle variations in the improvement with regards to strength and appearance of scars. Even then, we can still obtain similar results from surface under the cumulative ranking area rankings between dermatologists’ evaluation and PE. Micro-needling fractional radiofrequency and non-ablative fractional laser show poor therapeutic efficacy while fractional carbon dioxide laser, neodymium-doped yttrium aluminium garnet, and erbium-doped yttrium aluminium garnet have a good curative effect. Among them, doctors’ judgment is significantly more skewed to neodymium-doped yttrium aluminium garnet and fractional carbon dioxide laser while patients’ more skewed to erbium-doped yttrium aluminium garnet. These results reflect those of Nirmal et al. (2013)25 who also found that patients’ satisfaction of improvement of erbium-doped yttrium aluminium garnet was higher when compared to physicians’ observations. About adverse effects, the results show consistency between surface under the cumulative ranking area rankings and pairwise comparison both in VAS and post-inflammatory hyperpigmentation. Plasma and micro-needling fractional radiofrequency show maximal pain but comparatively lower complication rates while neodymium-doped yttrium aluminium garnet and erbium-doped yttrium aluminium garnet reflect mild pain but a higher rate of post-inflammatory hyperpigmentation. These results also corroborate the findings of previous work by Xie et al.26 The low post-inflammatory hyperpigmentation rate of radiofrequency therapies can be interpreted by the characteristics of high temperature and high energy, which will not vaporize the tissue and retain minimally invasive epidermis or part of the dermis as a biological dressing. As for neodymium-doped yttrium aluminium garnet and erbium-doped yttrium aluminium garnet, their absorbing main chromophores laser energy are not melanin but the sebaceous glands, water, and adjacent dermal tissues, which probably relate to their higher post-inflammatory hyperpigmentation.27 Even though, they still have indelible advantages in good tolerance, short downtime, and superior results.28,29
Taking this one step further, we may confirm our comprehensive ranking of both efficacy and safety of six photoelectric therapies. Fractional carbon dioxide laser can be more widely used in clinical treatment for acne scars in the future because of its exceptional efficacy as Peprahk et al. mentioned.30 Neodymium-doped yttrium aluminium garnet and erbium-doped yttrium aluminium garnet has been proposed as quite good efficacy and a higher level of tolerance which need to be further confirmed by more randomised controlled trials. Although non-ablative fractional laser has a lesser effect, it can be used as a conservative laser option for mild acne scars because of its low rate of post-inflammatory hyperpigmentation. This coincides with the report by Chan et al. (2010),30 who certified the safety of non-ablative fractional laser and indicated that its clinical efficacy could be maintained by increasing the total number of treatment sessions. Finally, plasma can be used for patients who require faster and better efficacy as well as have high pain tolerance. Micro-needling fractional radiofrequency only has the advantage of low post-inflammatory hyperpigmentation but is not frequently recommended.
Our network meta-analysis does present some notable limitations. Apart from the absence of direct comparison and relatively small sample size, the lack of objective and quantitative evidence such as histopathological results and severity score, ECCA (Echelle d'Evaluation Clinique des Cicatrices d'Acné) grading scale scores or Goodman & Baron score) still make our study not fully objective. We believe that an increasing number of clinical trials will be conducted with the development of cosmetic dermatology.
Conclusion
This study set out to assess the efficacy and safety of 6 photoelectric therapies for atrophic acne scars. Fractional carbon dioxide laser remains the most popular potentially curative treatment. Neodymium-doped yttrium aluminium garnet and erbium-doped yttrium aluminium garnet require greater efforts to prove their superior effectiveness. Non-ablative fractional laser might be appropriate for mild and moderate cases because of good tolerance while plasma seems to be the choice for patients with higher pain thresholds. Further investigations with multicentre randomised controlled trial data of acne scars are needed.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
This work was supported by financial grants from the National Natural Science Foundation of China (No. 30873268).
Conflict of interest
There are no conflicts of interest.
References
- New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60:S1-50.
- [CrossRef] [PubMed] [Google Scholar]
- Management of acne scarring, part II: A comparative review of non-laser-based, minimally invasive approaches. Am J Clin Dermatol. 2012;13:331-40.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions for acne scars. Cochrane Database Syst Rev. 2016;4:CD011946.
- [CrossRef] [PubMed] [Google Scholar]
- Radiofrequency ablation in dense ventricular scar-Longer continuous lesions may be beneficial. J Cardiovasc Electrophysiol. 2020;31:1891.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy, safety, and guidelines of application of the fractional ablative laser erbium YAG 2940 nm and non-ablative laser erbium glass in rejuvenation, skin spots, and acne in different skin phototypes: A systematic review. Lasers Med Sci. 2020;35:1877-88.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of atrophic acne scarring with fractional micro-plasma radio-frequency in Chinese patients: A prospective study. Lasers Surg Med. 2018;50:844-850.
- [CrossRef] [PubMed] [Google Scholar]
- A method of moments estimator for random effect multivariate meta-analysis. Biometrics. 2012;68:1278-84.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676-80.
- [CrossRef] [PubMed] [Google Scholar]
- Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28:123-37.
- [CrossRef] [PubMed] [Google Scholar]
- Graphical tools for network meta-analysis in STATA. PLoS One. ;8:e76654.
- [CrossRef] [PubMed] [Google Scholar]
- Automated methods to test connectedness and quantify indirectness of evidence in network meta-analysis. Res Synth Methods. 2019;10:113-124.
- [CrossRef] [PubMed] [Google Scholar]
- Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-34.
- [CrossRef] [PubMed] [Google Scholar]
- Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J Clin Epidemiol. 2011;64:163-71.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical reconstruction of skin scars (CROSS) method for atrophic scars: A comprehensive review. J Cosmet Dermatol. 2021;20:18-27.
- [CrossRef] [PubMed] [Google Scholar]
- Principles and development of collagen-mediated tissue fusion induced by laser irradiation. Sci Rep. 2019;9:9383.
- [CrossRef] [PubMed] [Google Scholar]
- Histologic comparison of microscopic treatment zones induced by fractional lasers and radiofrequency. J Cosmet Laser Ther. 2014;16:317-23.
- [CrossRef] [PubMed] [Google Scholar]
- Dermal Remodeling of Burn Scar by Fractional CO2 Laser. Aesthetic Plast Surg. 2016;40:761-8.
- [CrossRef] [PubMed] [Google Scholar]
- Non-ablative fractional laser provides long-term improvement of mature burn scars-a randomized controlled trial with histological assessment. Lasers Surg Med. 2015;47:141-7.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo histological evaluation of fractional ablative microplasma radio frequency technology using a roller tip: An animal study. Lasers Med Sci. 2015;30:2287-94.
- [CrossRef] [PubMed] [Google Scholar]
- Microneedle radiofrequency. Facial Plast Surg Clin North Am. 2020;28:9-15.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-38.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional radiofrequency treatment in acne scars: Systematic review of current evidence. J Cosmet Laser Ther. 2016;18:442-447.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser for the treatment of facial atrophic acne scars: Prospective clinical trial with short and long-term evaluation. Lasers Med Sci. 2017;32:2047-2054.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of Erbium-doped Yttrium Aluminium Garnet fractional resurfacing laser for treatment of facial acne scars. Indian J Dermatol Venereol Leprol. 2013;79:193-8.
- [CrossRef] [PubMed] [Google Scholar]
- [Laser and related photoelectric therapies for scar worth expecting] Zhonghua Shao Shang Za Zhi. 2018;34:598-602.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of pulse energy variations on the dimensions of microscopic thermal treatment zones in nonablative fractional resurfacing. Lasers Surg Med. 2007;39:145-55.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of atrophic facial scars of acne vulgaris by Q-Switched Nd:YAG (Neodymium: Yttrium-Aluminum-Garnet) laser 1064 nm wavelength. J Cosmet Laser Ther. 2012;14:224-33.
- [CrossRef] [PubMed] [Google Scholar]
- Histological validity and clinical evidence for use of fractional lasers for acne scars. J Cutan Aesthet Surg. 2012;5:75-90.
- [CrossRef] [PubMed] [Google Scholar]
- Fractionated CO2 Laser for Scar Improvement: A Review of Clinical Effectiveness and Cost-Effectiveness [Internet] Canadian Agency for Drugs and Technologies in Health Copyright © 2019 Canadian Agency for Drugs and Technologies in Health., Ottawa (ON), 2019
- [PubMed] [Google Scholar]






