Translate this page into:
Cutaneous granulocytic sarcoma arising on a surgical scar
Corresponding author: Dr. Mouna Korbi, Department of Dermatology, University of Monastir, Fattouma Bourguiba University Hospital, Monastir, Tunisia. korbimouna68@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Korbi M, Rouatbi J, Belloumi D, Hermassi A, Sriha B, Sahraoui G, et al. Cutaneous granulocytic sarcoma arising on a surgical scar. J Dermatol Venereol Leprol 2023;89:735-37
Dear Editor,
Granulocytic sarcoma, also known as myeloid sarcoma, involves the localization of myeloblasts or immature myeloid cells to an extramedullary site. 1 Although cutaneous granulocytic sarcoma is rare, it occurs most commonly in association with acute myeloid leukaemia, affecting 2.5–9.1% of patients. 1 Herein, we report a case of cutaneous granulocytic sarcoma as the presenting sign of acute myeloid leukaemia relapse without signs of systemic involvement, which demonstrated a predilection for an old surgical scar.
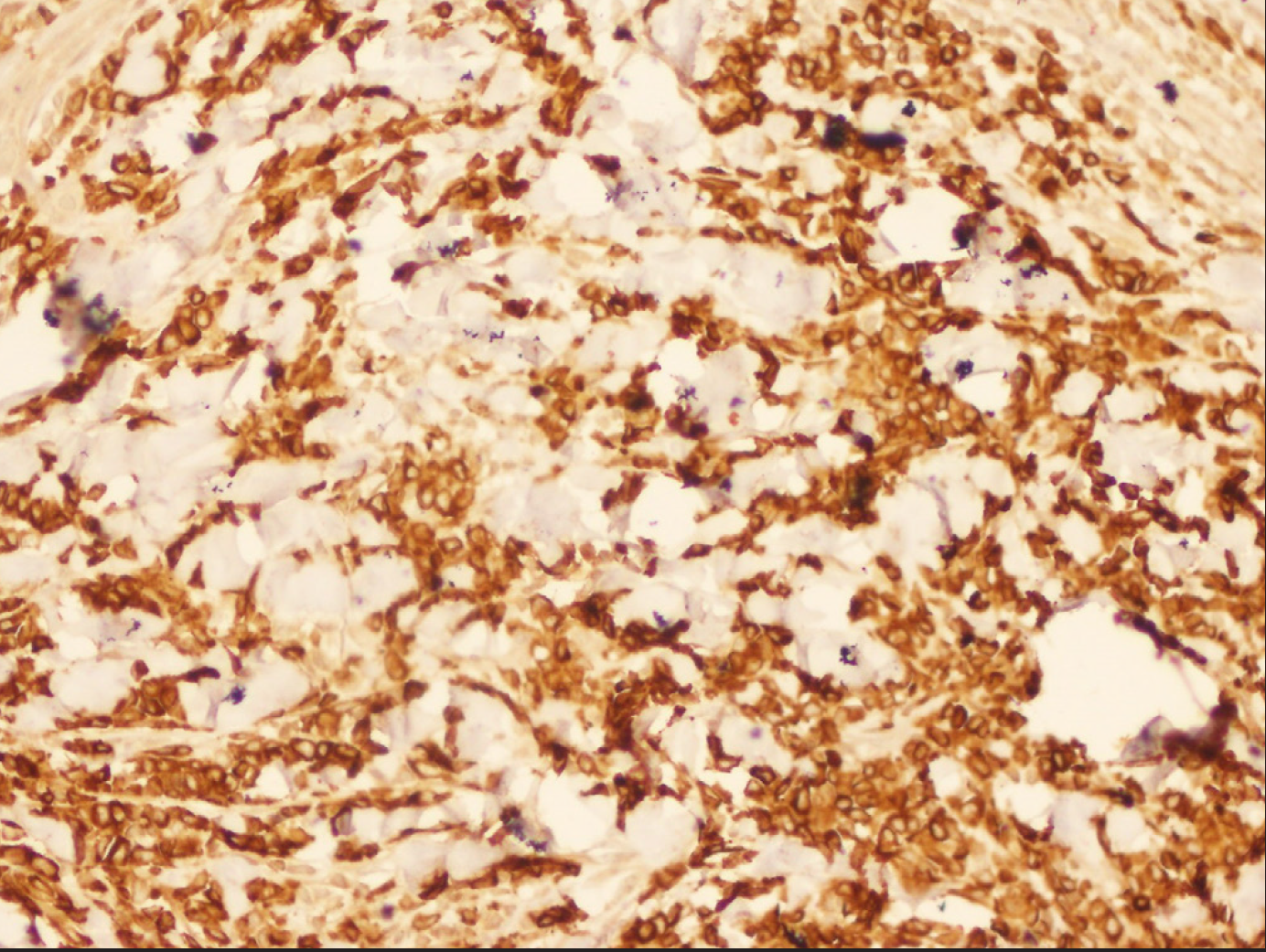
A 33-year-old woman was referred to the Dermatology departmetn of the University Hospital of Monastir, Tunisia, in May 2021, for a one week history of a painful plaque wich was spontaneous in onset. She had a history of appendicectomy in 2006. She was diagnosed with acute myeloid leukaemia in April 2019. Cytogenetic studies and screening for gene rearrangements, did not show genetic mutations. According to the revised World Health Organization classification of tumours of haematopoietic and lymphoid tissues, 2 a diagnosis of acute myelomonocytic leukaemia was made based on the morphology and immunophenotype. She received four courses of chemotherapy, followed by haematopoietic stem cell transplantation and was in remission 20 months prior to current consultation. On physical examination, the patient was in good condition. There was no lymphadenopathy. Cutaneous examination revealed an indurated purple plaque infiltrating around the appendicectomy surgical wound, with a bullous evolution in the centre [Figure 1a]. She had no other surgical or previous traumatic scar sites elsewhere on her body. A skin biopsy was taken with a differential diagnosis of malignancy-associated Sweet syndrome, subcutaneous panniculitis-like T-cell lymphoma or leukaemia cutis. Histological examination showed massive infiltration of blast cells with round nuclei and scant cytoplasm [Figures 1b and 1c]. Immunohistochemically, myeloblasts were found to be positive for myeloperoxidase, CD117 and CD34 [Figures 2a, 2b and 2c]. Based on the clinical presentation and the histopathological findings, the patient was diagnosed with cutaneous granulocytic sarcoma. Total WBC count was within normal levels, but with circulating blast cells. In bone marrow analysis, myeloblasts represented 24% of the nucleated cells. After salvage chemotherapy course, complete remission was achieved in bone marrow smears with regression of the skin lesion.

- Infiltrated purple plaque around the appendicectomy surgical incision wound
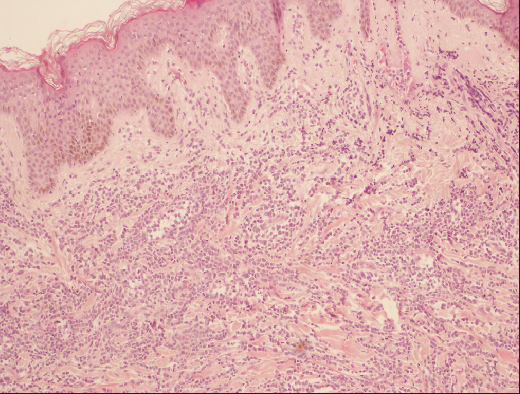
- Massive infiltration of haematopoietic cells within the granulocytic sarcoma (H&E, 100x)
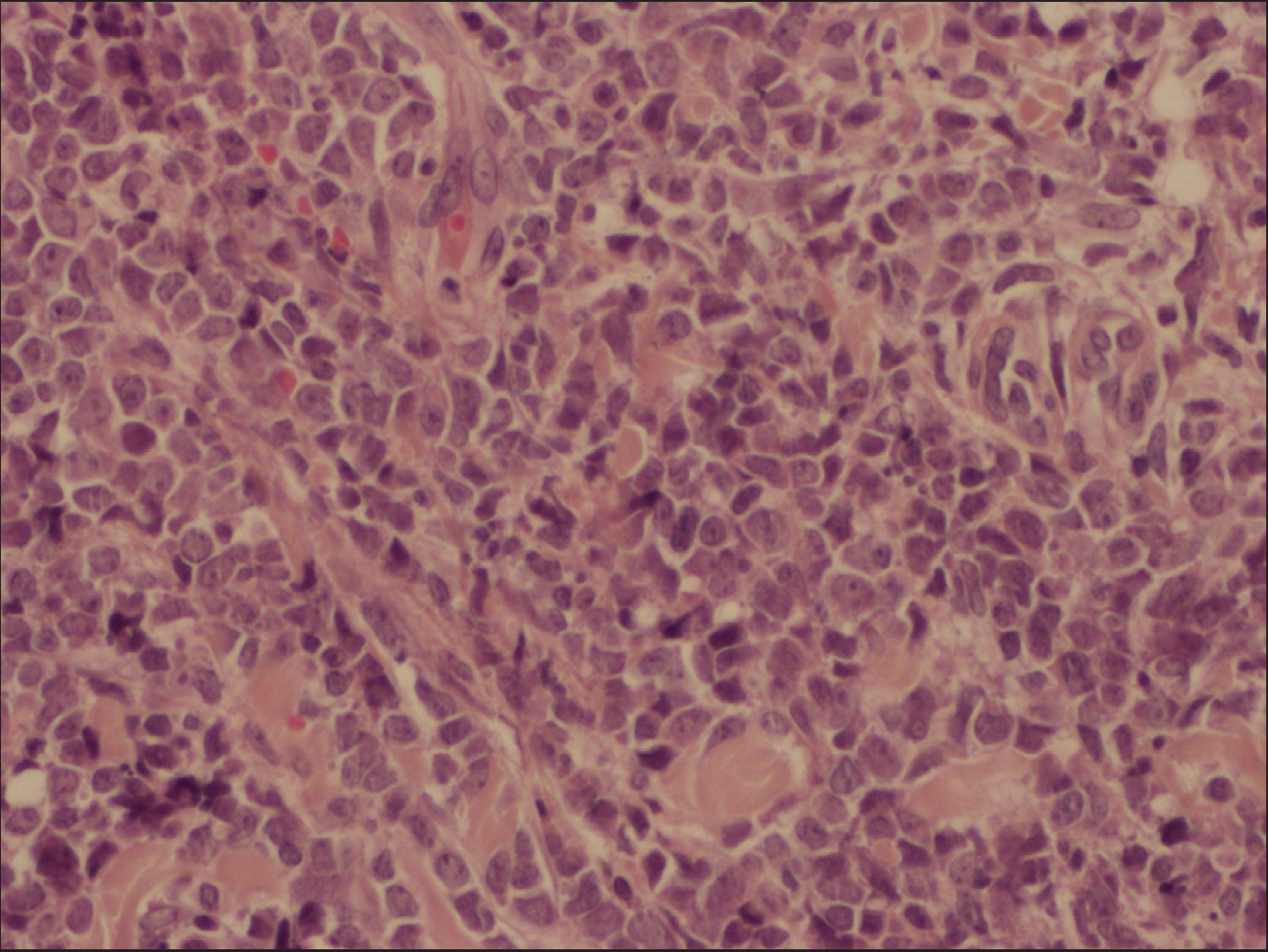
- Tumour cells have a high nucleocytoplasmic ratio, with large irregular nuclei, often nucleolated (H&E, 400x)
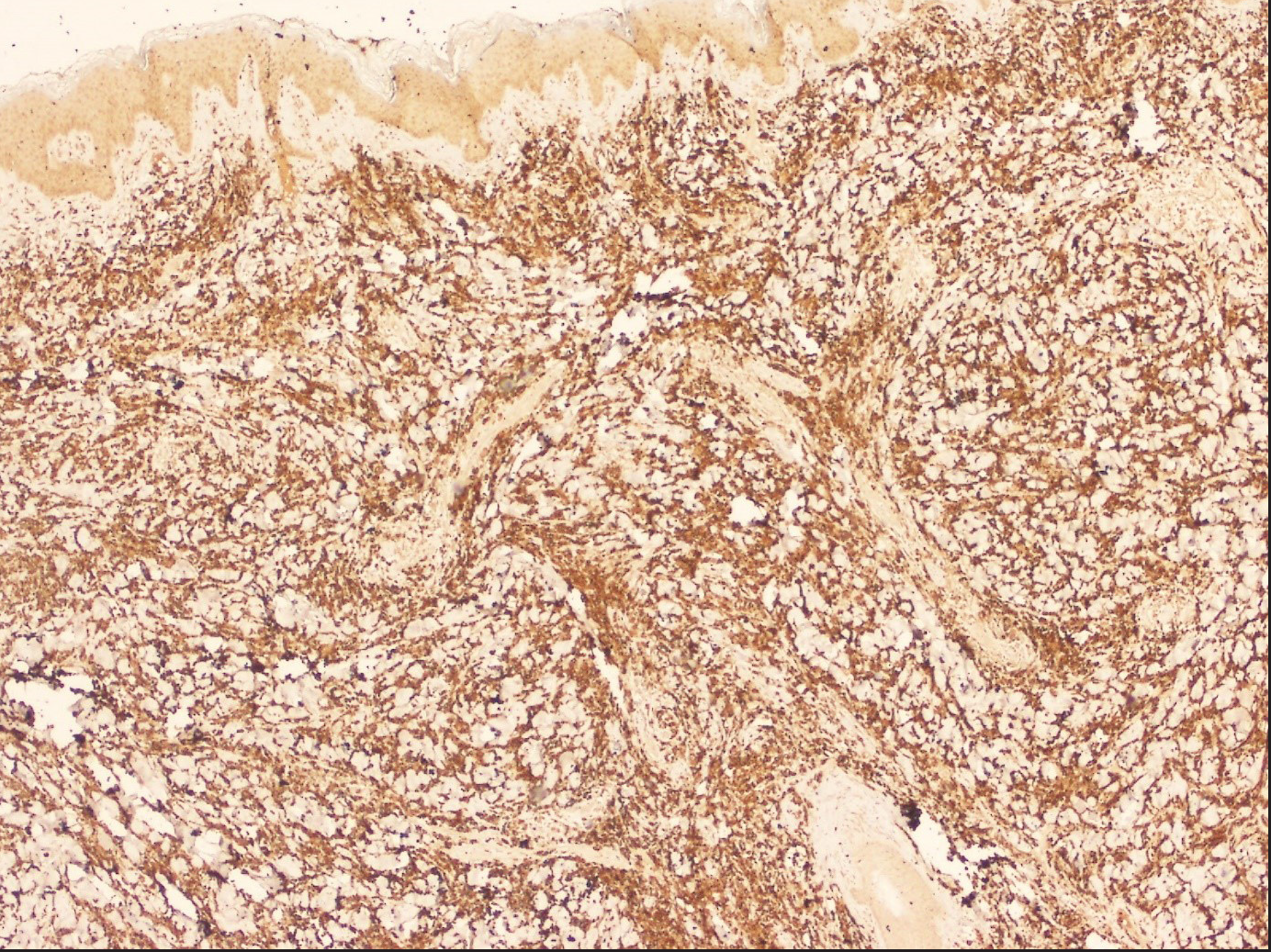
- Immunohistochemical analysis shows positivity of blast cells to myeloperoxidase (original magnification, 100x)
- Immunohistochemical analysis shows positivity of blast cells to CD117
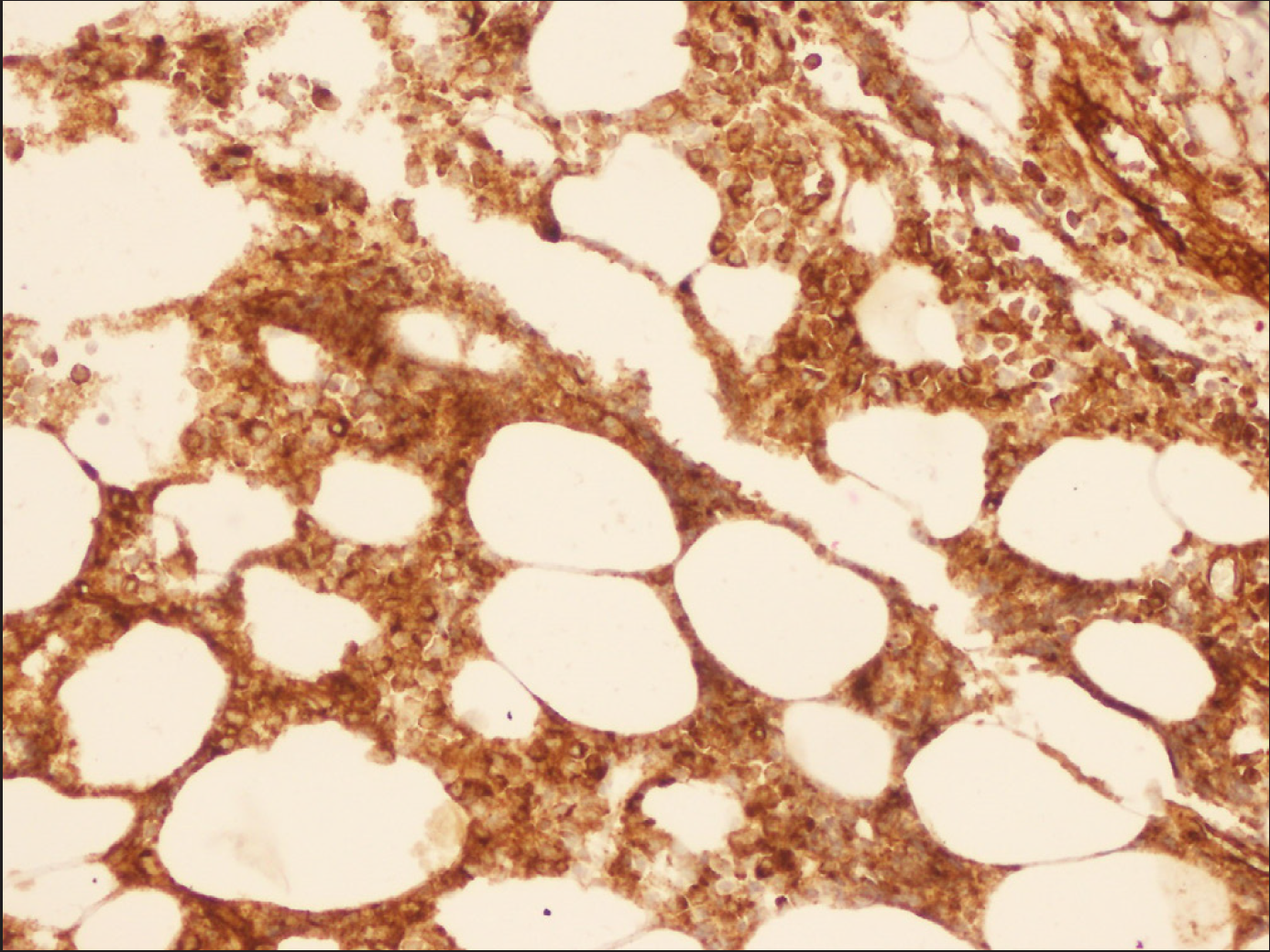
- Immunohistochemical analysis shows positivity of blast cells to CD34 (original magnification, 400x)
We present an unusual case of cutaneous granulocytic sarcoma arising on surgical scar as a sole sign of relapsed acute myeloid leukaemia. Indeed, cutaneous manifestations in leukaemia can be diverse and present as specific and non-specific signs. Non-specific manifestations do not show leukemic infiltration of skin and are mediated by various factors related to cytokines, hormones, or autoimmunity. Specific signs present as cutaneous granulocytic sarcoma also called leukaemia cutis, which is a generic term to describe specific cutaneous involvement. This condition can occur with concurrent active acute myeloid leukaemia or in the setting of its extramedullary relapse, including in the post bone marrow transplant setting, 1 as well in cases such as that of our patient. Interestingly, in our case, the cutaneous leukemic infiltrates were limited to the site of an old surgical scar with no signs of diffuse cutaneous involvement.
Cutaneous infiltration of blast cells in traumatic scars in patients with acute myeloid leukaemia can be attributed to chemical mediators such as interleukin-1 for chemotaxis of monocytes, which might be released from not only new wounds but also old scars. 3 A similar explanation was provided previously, as a local tumour growth-promoting factor, possibly a product of dead or dying normal cells, may be involved in the ability of leukemic monocytes and myelomonocytes to proliferate in surgical scars. 4 Moreover, two case reports of cutaneous granulocytic sarcoma that occurred after trauma (haematoma and cutaneous surgery) in the context of myelodysplastic syndrome were described as a result of Koebner phenomenon or isomorphic response. 5 In our case, cutaneous granulocytic sarcoma occurring on the surgical scar seems to be not suggestive of the Koebner phenomenon, as it developed in a pre-existing surgical scar that evolved 15 years ago. A more broadly applied term, locus minoris resistentiae (refers to a body region of lessened resistance that is more vulnerable than others 6 ) may be more appropriate to describe the phenomenon observed in our case, in which cutaneous granulocytic sarcoma was not preceded by an inflammatory process, did not occur in a patient with a known dermatosis, and manifested over 10 years after initial skin trauma. So, the wound site merely served as a determinant of its localization.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Myeloid sarcoma: Presentation, diagnosis, and treatment. Clin Lymphoma Myeloma Leuk. 2017;17:263-7.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of acute myeloid leukemia. Blood Res. 2020;55:S1-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leukemia cutis in acute myelomonocytic leukemia: Infiltration to minor traumas and scars. J Dermatol. 1991;18:281-5.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma and the localization of tumor cells. Cancer. 1967;20:23-30.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous granulocytic sarcoma and Koebner phenomenon in a context of myelodysplastic syndrome. JAAD Case Rep. 2015;1:207-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Locus minoris resistentiae: An old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-6.
- [CrossRef] [PubMed] [Google Scholar]





