Translate this page into:
Traumatic dystrophic calcinosis cutis in a child successfully treated with sodium metabisulfite ointment
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Bhoi AK, Khandpur S. Traumatic dystrophic calcinosis cutis in a child successfully treated with sodium metabisulfite ointment. Indian J Dermatol Venereol Leprol. 2024;90:656-8. doi: 10.25259/IJDVL_139_2023
Dear Editor,
A 13-year-old girl presented with multiple erythematous papules and nodules with ulceration and crusting, on her right knee for the past 1.5 years. There was a history of recurrent discharge of chalky white material from the lesions. The lesions did not limit any movement in the patient. There was no fever, muscle weakness, photosensitivity or any other systemic complaints. The patient had sustained trauma on the right knee due to a fall from a bicycle five years ago. Considering a diagnosis of an infective aetiology including scrofuloderma and atypical mycobacterial infection, she had received multiple courses of oral antibiotics and intralesional steroids before presenting to us with minimal improvement. Dermatological examination revealed multiple erythematous and yellow, discrete and coalescent, papules and nodules of size 0.5–1 cm on the right knee. Some lesions were arranged in a linear pattern. The papules were centrally ulcerated with whitish chalky deposits, along with variable white scaling and crusting. There were interspersed, small atrophic round scars [Figure 1]. The lesions were firm-to-hard on palpation. There was mild tenderness with no restriction of movement at the knee joint.
Dermatoscopy of the ulcerated erythematous papules showed scaling and crusting, central yellowish-to-white globules, with a surrounding rim of erythema and telangiectasias [Figure 2a]. A plain radiograph of the right knee joint revealed multiple well-defined periarticular opacities suggesting calcification [Figure 2b]. Serum calcium, phosphorus, vitamin D and parathyroid hormone levels were within normal limits. Histopathology on haematoxylin and eosin showed amorphous purple–blue dermal deposits suggestive of calcinosis cutis [Figure 2c]. A diagnosis of dystrophic calcinosis cutis probably secondary to preceding trauma was considered, and the patient was started on topical 25% sodium metabisulfite ointment applied twice daily. For this preparation, 25 g of sodium metabisulfite powder was mixed with 75 g of commercial petroleum jelly by rapidly stirring it using a small spoon for a few minutes in a plastic container until a homogenous mixture without visible powdery residue was obtained. After regular application of the prepared ointment for 3 months there was complete resolution of ulceration and discharge. The size of the lesions also decreased significantly, and many lesions resolved with scarring [Figure 3].

- Multiple erythematous and yellow, discrete and coalescent, papules and nodules with central ulceration, white scaling and crusting on the right knee in a 13-year-old girl. Some papules are linearly arranged.
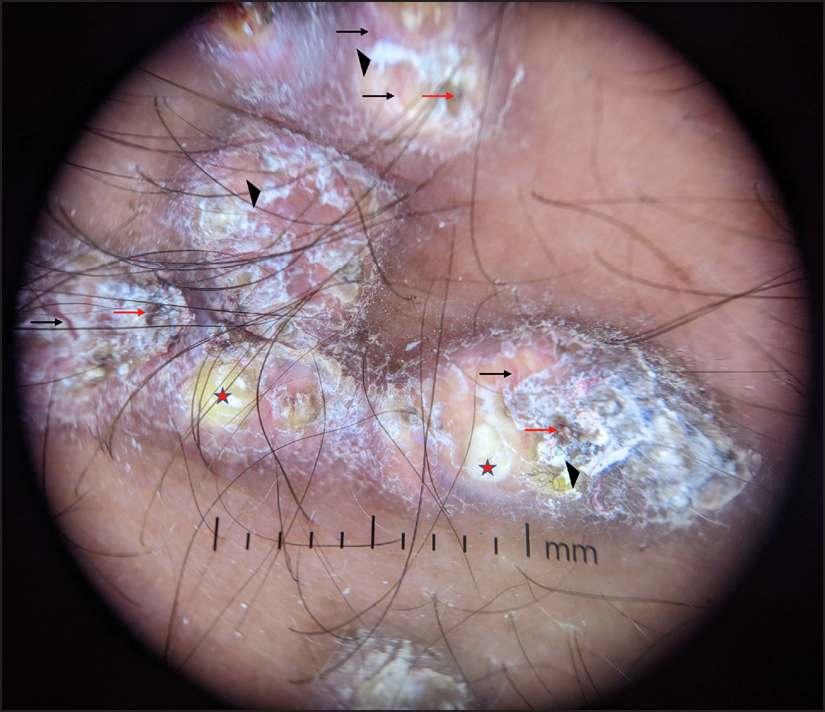
- Dermatoscopy of erythematous ulcerated papules showing scaling (black triangles), crusting (red arrows), central yellow globules (red stars) surrounded by areas of erythema and peripheral telangiectasias (black arrows) (Heine delta 20T, x10, polarised mode).
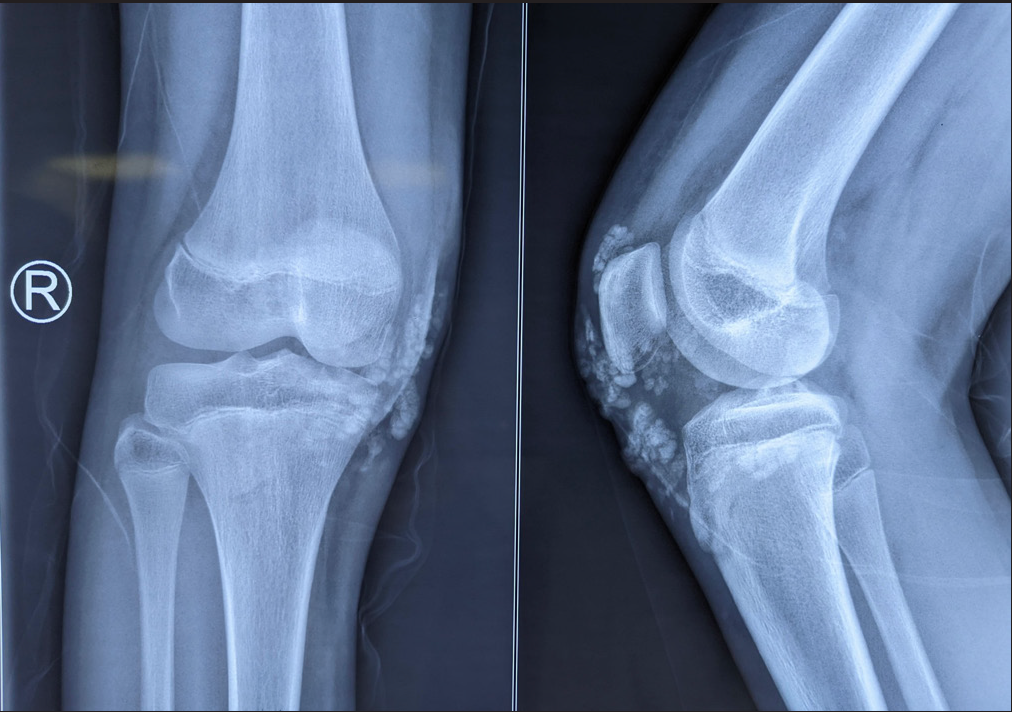
- X-ray of right knee, antero-posterior and lateral view, showing amorphous opacities in the skin and subcutaneous plane suggestive of calcinosis cutis.
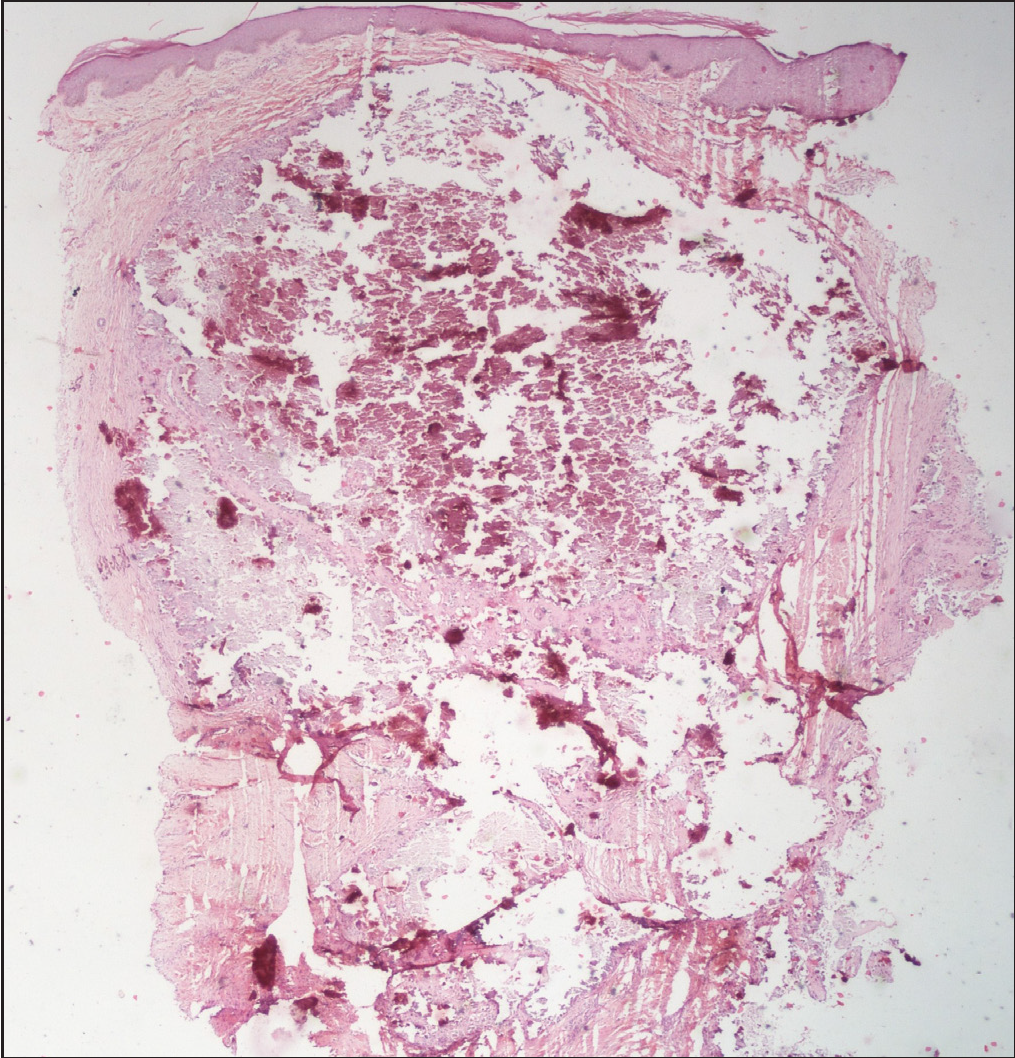
- Biopsy from an erythematous papule showing a large central collection of amorphous purple deposits with a fragmented appearance, suggestive of calcium (Haematoxylin and eosin, 20x).

- Response with sodium metabisulfite ointment in traumatic calcinosis cutis. Significant decrease in discharge, crusting and size of the papules. Complete resolution of a few papules with atrophic scars
Calcinosis cutis is characterised by abnormal deposition of calcium salts in the skin. It is classified into three types based on pathology—dystrophic, metastatic and idiopathic. Dystrophic cutaneous calcification occurs due to the precipitation of calcium at sites of tissue damage, without any increase in the serum calcium levels. It is the most common type of calcinosis cutis reported in the paediatric population. It can be seen in various conditions such as pilomatrixoma, cysts, subcutaneous fat necrosis of the newborn, trauma and autoimmune and inherited disorders of connective tissue. Traumatic dystrophic calcification without any primary skin condition is very rare with limited reports in the literature. Larralde et al. described calcinosis cutis in a child which developed 10 days after sustaining multiple abrasions in the inguinal folds which resolved quickly with spontaneous transepidermal elimination of calcium. 1 However, frequently, traumatic calcinosis cutis lesions do not self-resolve. In a study of 30 cases of paediatric calcinosis cutis from a single centre, 13 of the 30 cases were of dystrophic calcinosis cutis, out of which three had a preceding trauma. 2
Calcinosis cutis is a difficult-to-treat condition. Intralesional and topical steroids, calcium channel blockers, bisphosphonates, surgical excision etc have been used with an inconsistent and unsatisfactory response. Extracorporeal shock-wave lithotripsy (ESWL), and various lasers such as CO2, Er:YAG and diode lasers are minimally invasive options for calcinosis cutis. 3 Sodium metabisulfite and sodium thiosulfate are organic compounds that chelate and increase the solubility of calcium in the blood by converting less soluble calcium salts to more soluble calcium salts, and by inhibiting the agglomeration of calcium oxalate salts. Sodium thiosulfate was first used intravenously in patients with calciphylaxis with a fairly good response. It has also been used intravenously for calcinosis cutis, but more commonly the topical and intralesional forms have been tried in calcinosis cutis secondary to various aetiologies to prevent side effects associated with intravenous injections. Concentrations ranging from 10–25% have been used, compounded with petrolatum or cream base. 4 Metabisulfite salt has been preferred by some researchers as it is cheaper and easily available. The response is varied, with a retrospective study of connective tissue disease patients with calcinosis cutis showing a response in 19 out of 28 (68%) cases. 4
Sodium thiosulfate, but not metabisulfite, in solution form as intralesional therapy has been used in 0.1–250 mg/dL concentration, usually in 0.1 mL/cm 2 dosage to the base of the lesions as weekly-to-monthly injections for 3–6 months, with good response in calcinosis cutis nodules. The best response was seen in a prospective case series of six patients who received weekly injections for 4 weeks and were then followed up for a total of 12 weeks. There was a 67% reduction in the size of lesions at the end of 4 weeks and 90% at the end of 12 weeks. Complete remission was seen in three out of the six patients. 5
In a systemic review, clinical improvement was seen in 39 (81%) out of 48 cases treated with topical sodium thiosulphate, and complete response was seen in 9 (19%) of these 48 cases. The median treatment duration was 3.9 months. 3 Clinical improvement was seen in 39 (74%) out of 53 cases treated with intralesional sodium thiosulphate, and complete response was seen in 19 (36%) of these 53 cases. 3 The median treatment duration was 1 month. The effect size of responses has not been properly quantified and correlated with the type of lesions and the extent of the disease in various reports. The response with topical therapies is expected to be poor in deep subcutaneous non-ulcerated lesions and in extensive disease. A combination of various modalities for an appropriate amount of time should be tried in such cases, along with attempts to discover newer therapies for this disabling condition.
Our case highlights the utility of topical sodium metabisulfite in a distressing condition such as calcinosis cutis in a case that showed no spontaneous reduction or resolution of lesions despite the absence of repetitive trauma. In resistant and extensive cases, topical sodium metabisulfite can be combined with other modalities to maximize the benefit to the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Calcinosis cutis following trauma. Pediatr Dermatol. 2005;22:227-9.
- [CrossRef] [PubMed] [Google Scholar]
- Characterizing calcinosis cutis in a pediatric population. Pediatr Dermatol. 2020;37:317-9.
- [CrossRef] [PubMed] [Google Scholar]
- Local, non-systemic, and minimally invasive therapies for calcinosis cutis: A systematic review. Arch Dermatol Res. 2022;314:515-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Topical sodium thiosulfate for calcinosis cutis associated with autoimmune connective tissue diseases: The Mayo Clinic experience, 2012–2017. Clin Exp Dermatol. 2019;44:e189-92.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of skin calcifications with intra-lesional injection of sodium thiosulphate: A case series. Acta Derm Venereol. 2016;96:257-8.
- [CrossRef] [PubMed] [Google Scholar]





