Translate this page into:
Intravascular pattern of cutaneous spread in a case of relapsed nasal natural killer/T-cell lymphoma
Corresponding author: Dr. Xiao Mei Zhu, Department of Dermatology, Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology, 1095 Jiefang AVE, Wuhan, Hubei, China. zhuxiaomei@tjh.tjmu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Zou P, Du YX, Cao YC, Zhu XM. Intravascular pattern of cutaneous spread in a case of relapsed nasal natural killer/T-cell lymphoma. Indian J Dermatol Venereol Leprol. 2024;90:220–2. doi: 10.25259/IJDVL_940_2022
Dear Editor,
Extranodal natural killer/T-cell lymphoma, nasal type, is an uncommon non-Hodgkin lymphoma. It mainly occurs in the nose and the paranasal area and also the skin. The skin involvement is mostly seen as erythematous nodules and ulcerated lesions. The pathology shows characteristic angiotropism or angiocentric pattern of growth. We report a case of nasal extranodal natural killer/T-cell lymphoma with an intravascular pattern in a 59-year-old woman.
A 59-year-old woman noticed erythema and nodules on her lower limbs and trunk for two months. Five years back, she had been diagnosed with stage I extranodal natural killer/T-cell lymphoma, nasal type and underwent surgical resection and post-operative radiotherapy with a complete ongoing response. No other medical or family history was recorded. She was found to have fever during physical examination. Skin examination revealed erythema, subcutaneous nodules and telangiectases on the limbs and trunk. Patchy dark erythema, ecchymoses and ulcers were seen on both calves [Figure 1].
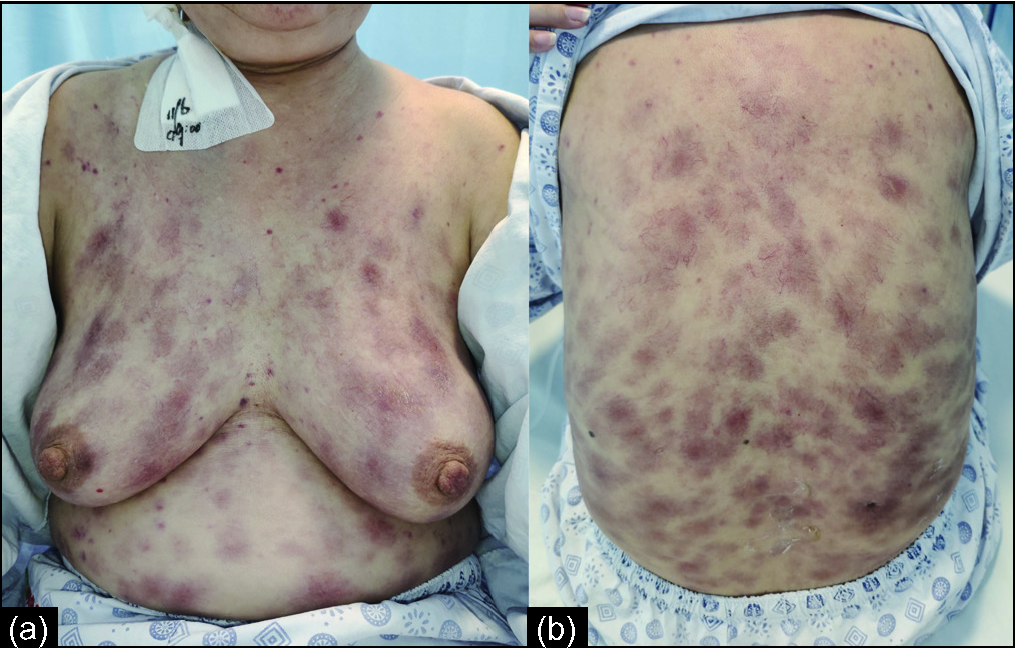
- Diffuse telangiectasia, erythema, and subcutaneous nodules on the trunk

- Dark red erythema, ulceration and erosion on the lower limbs
Laboratory tests showed mild anaemia (haemoglobin level of 73 g/L), thrombocytopenia (platelet count of 40 × 109/L), normal blood cell count, hypertriglyceridemia (300 mg/dL), hypofibrinogenemia (1.31 g/L), elevated ferritin (43921 ug/L) and soluble interleukin-2 receptor (3260 U/mL). Plasma Epstein-Barr virus nucleic acid level was 2.08 × 107 copies/mL and EBV-DNA level was 1.90 × 107 copies/mL. We did a skin biopsy from the lesion on the right lateral aspect of the back of the trunk. Histopathology showed many distended vessels filled with fibrin and medium-sized lymphoid cells with irregular nuclei in the dermis [Figure 2]. Bone marrow biopsy revealed myelodysplastic features without any atypical lymphoid infiltrate. Immunocytochemical analysis showed that the lymphocytes were positive for CD2, CD3, CD7, CD56, GrB and TIA-1. CD4, CD5, CD8 and CD20 were negative. The proliferation index of Ki67 was approximately 90%. CD31 and CD34 verified that all the tumour cells were restricted within the vessels [Figure 3]. Immunohistochemical analysis showed very similar results to the biopsy of nasal tissue five years ago, while the Ki67 was approximately 70%. PET-CT identified increased uptake in the soft tissue of the nose and the skin on the right lateral aspect of the back of the trunk. Based on the above findings, a diagnosis of cutaneous intravascular invasion by nasal extranodal natural killer/T-cell lymphoma was established. Secondary haemophagocytic lymphohistiocytosis accelerated the progression of her disease. She passed away soon after being diagnosed.
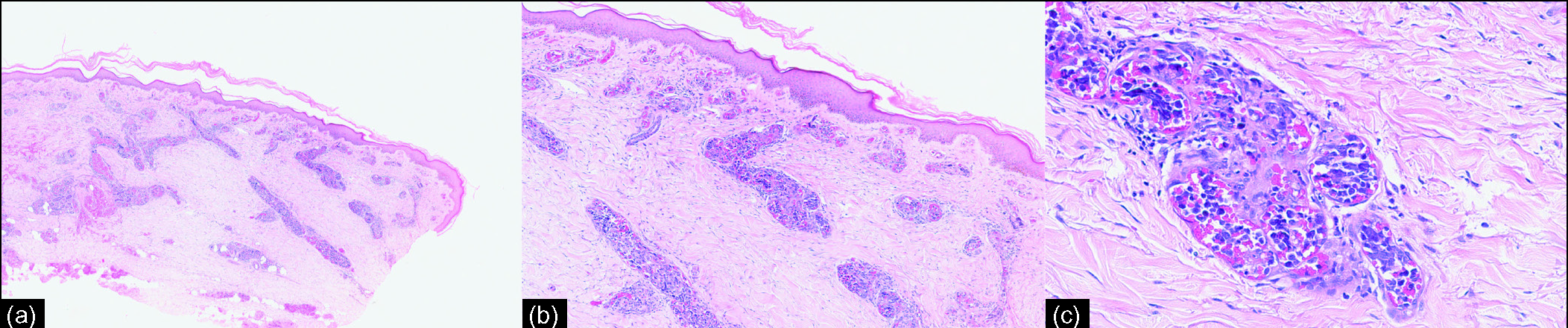
- Distended vessels filled with medium-sized lymphoid cells with irregular nuclei and fibrin in the dermis. (Haematoxylin-eosin stain; a: ×40; b: ×100; c: ×400)
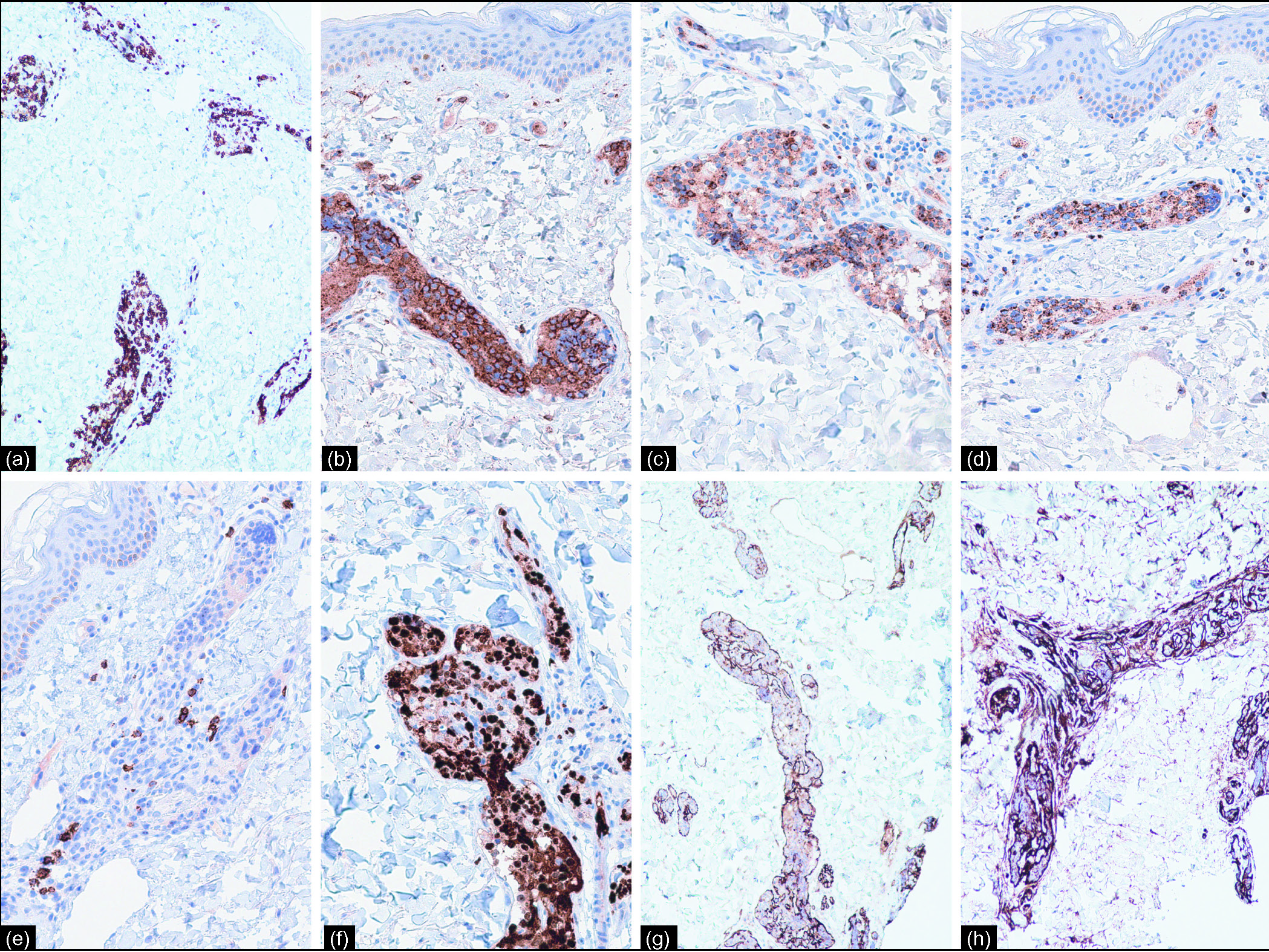
- The intravascular lymphoma cells were CD3+ (a), CD56+ (b), GrB+ (c), TIA-1+(d), CD20- (e), Ki-67 (approximately 90%) (f) and the intravascular localization of the lymphoma cells are highlighted by CD31 (g) and CD34 (h)
Intravascular lymphoma, a rare type of non-Hodgkin lymphoma, is most commonly reported in large B-cell lymphomas. Nevertheless, a few were found to be of T-cell lineage. It is characterised by lymphoma being strictly restricted within the vessels. We reported the intravascular localisation of lymphoma cells in the skin biopsy of a patient with a history of nasal extranodal natural killer/T-cell lymphoma. We, therefore, need to distinguish it from intravascular lymphoma. Considering that intravascular natural killer/T-cell lymphoma has not been considered as a specific entity lymphoma by World Health Organization, and it might be a related disease of extranodal natural killer/T-cell lymphoma,1 we mainly differentiate cutaneous extranodal natural killer/T-cell lymphoma from intravascular large B-cell lymphoma.
Clinically, unlike extranodal natural killer/T-cell lymphoma, the most commonly affected organs in intravascular large B-cell lymphoma are the skin and central nervous system, while other sites, including the heart, spleen, lung and liver, can also be affected. However, the manifestations when the skin are involved are very similar, such as ill-defined violaceous plaques on the trunk and extremities, scaling plaques, ulcerated nodules, telangiectasia, painful indurated erythematous eruptions and red–blue nodules. Pathologically, tumour cells of extranodal natural killer/T-cell lymphoma are mainly characterised by angiocentric and angiodestructive growth patterns rather than intravascular invasion. Furthermore, the cytotoxic markers, TIA-1 and GrB, can help us differentiate extranodal natural killer/T-cell lymphoma from intravascular large B-cell lymphoma because the cytotoxic phenotype of the latter is non-activated. Besides, almost all intravascular large B-cell lymphoma display constant CD20 expression. Nevertheless, several cases of intravascular patterns of extranodal natural killer/T-cell lymphoma have been reported in recent years. Kusari et al.2 reported a case with angiotropism and genuine intravascular involvement in the biopsy. Obara et al.3 described this disease, presenting intravascular positioning of tumour cells when they took skin biopsies from both plaque and normal skin. Battesti et al.4 and Yu et al.5 reported two patients with a history of it whose skin biopsy showed intravascular lymphoma cell infiltration. These reports broke the absolute angiocentric and angiodestructive growth patterns of extranodal natural killer/T-cell lymphoma. The cause of intravascular localisation is not known, perhaps it is similar to intravascular large B-cell lymphoma where the molecular expression promote cell migration and attachment to the endothelium, but lack the markers that promote extravasation.6
According to the patient’s clinical manifestations, we also must distinguish it from vasculitis and erythema nodosum. Our patient’s biopsy did not show the characteristics of vasculitis, such as inflammatory cell infiltration, fibrinoid degeneration and granuloma formation, or the characteristics of erythema nodosum, such as panniculitis.
For localised extranodal natural killer/T-cell lymphoma, radiotherapy combined with chemotherapy is the standard treatment. For disseminated disease, systemic chemotherapy remains the primary treatment. Common chemotherapy regimens include DeVIC (dexamethasone, etoposide, ifosfamide, carboplatin) and SMILE (dexamethasone, methotrexate, ifosfamide, E. coli L-asparaginase, etoposide). The most common neoplastic trigger for haemophagocytic lymphohistiocytosis is the T- and natural killer cell lymphoma. The primary therapy of it is most frequently high-dose corticosteroids combined with etoposide.7
In conclusion, we report a patient with nasal extranodal natural killer/T-cell lymphoma with cutaneous intravascular recurrence. The lack of active follow-up after the patient’s lesions had been resected five years back may be one of the reasons for the delay in diagnosis and starting treatment. The overall survival rate of patients with cutaneous extranodal natural killer/T-cell lymphoma is low. There is still a lack of sufficient understanding of these diseases, their pathogenesis, effective treatment options and prognostic factors. Early diagnosis by histopathological examination may be crucial for the patient’s medical prognosis and early treatment.
Declaration of patient consent
Patient’s consent not required as her identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- New concepts in EBV-associated B, T, and NK cell lymphoproliferative disorders. Virchows Arch. 2023;482:227-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Widespread erythematous plaques with prominent telangiectases. JAMA Dermatol. 2021;157:1376-7.
- [CrossRef] [PubMed] [Google Scholar]
- Case of extranodal natural killer/T-cell lymphoma, nasal type, presenting with intravascular localization of tumor cells in skin biopsies from both plaque and normal-appearing skin: a case report and literature review. Am J Dermatopathol. 2020;42:196-203.
- [CrossRef] [PubMed] [Google Scholar]
- Intravascular relapse of an extra-nodal NK/T-cell lymphoma, nasal-type, presenting as diffuse and eruptive telangiectasia. Eur J Cancer. 2021;156 Suppl 1:S63-s4.
- [CrossRef] [PubMed] [Google Scholar]
- Intravascular large NK/T-cell lymphoma: a variant of extranodal NK/T-cell lymphoma, nasal type? Eur J Dermatol. 2019;29:440-2.
- [CrossRef] [PubMed] [Google Scholar]
- Intravascular large B-cell lymphoma: A chameleon with multiple faces and many masks. Blood. 2018;132:1561-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hemophagocytic lymphohistiocytosis. Annu Rev Pathol. 2018;13:27-49.
- [CrossRef] [PubMed] [Google Scholar]





