Translate this page into:
Cervicofacial actinomycosis with an atypical presentation
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, AIIMS, Sijua, Patrapada, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash S, Behera B, Sethy M, Garg S, Mishra J, Sarkar N. Cervicofacial actinomycosis with an atypical presentation. Indian J Dermatol Venereol Leprol. 2024;90:217–9. doi: 10.25259/IJDVL_1024_2022
Dear Editor,
Cervicofacial actinomycosis, also called lumpy jaw, is a chronic, suppurative and granulomatous bacterial infection caused mostly by Actinomyces species and rarely by Propionicusbacterium species.1 It classically presents as an indurated and suppurative nodule which subsequently results in draining sinuses and tissue fibrosis.1 Herein, we present an atypical morphological presentation of cervicofacial actinomycosis, resembling a ‘bunch of grapes’.
A 45-year-old man presented with multiple, painless red elevated lesions on his face since 6 months. There was no history of granular discharge, any congenital anomaly, dental pain, dental procedure or trauma prior to the appearance of lesions. Personal and family history was unremarkable. Cutaneous examination showed multiple erythematous to pinkish-grey nodules on an indurated base, resembling a “bunch of grapes” on the left side of the face around nose. It was associated with swelling of the nose, upper lip and left mandible [Figure 1]. There was no regional lymphadenopathy. General examination and other systemic examinations were unremarkable. On dermoscopy (Dermlite DL4, polarised, 10× magnification), yellow homogenous areas, arborizing vessels and shiny white structures were visible [Figure 2]. Haematological parameters were within normal limits and radiological investigations failed to show any bony abnormality. We considered cervicofacial actinomycosis, and botryomycosis as differentials. Histopathology revealed granules with radiating slender filaments [Figure 3a] and the Grocott Methenamine silver stain showed filamentous bacteria [Figure 3b]. Cultures for bacteria, Mycobacteria, fungus and Actinomyces did grow any organism. A diagnosis of actinomycosis was made, and the patient was treated with oral amoxicillin with clavulanic acid 625 mg thrice daily and oral doxycycline 100 mg twice daily. The lesions resolved completely after 5-months [Figure 4].

- Multiple, erythematous to pinkish-grey nodules on an indurated base giving an appearance like a “bunch of grapes” on the left side of the face around the nose
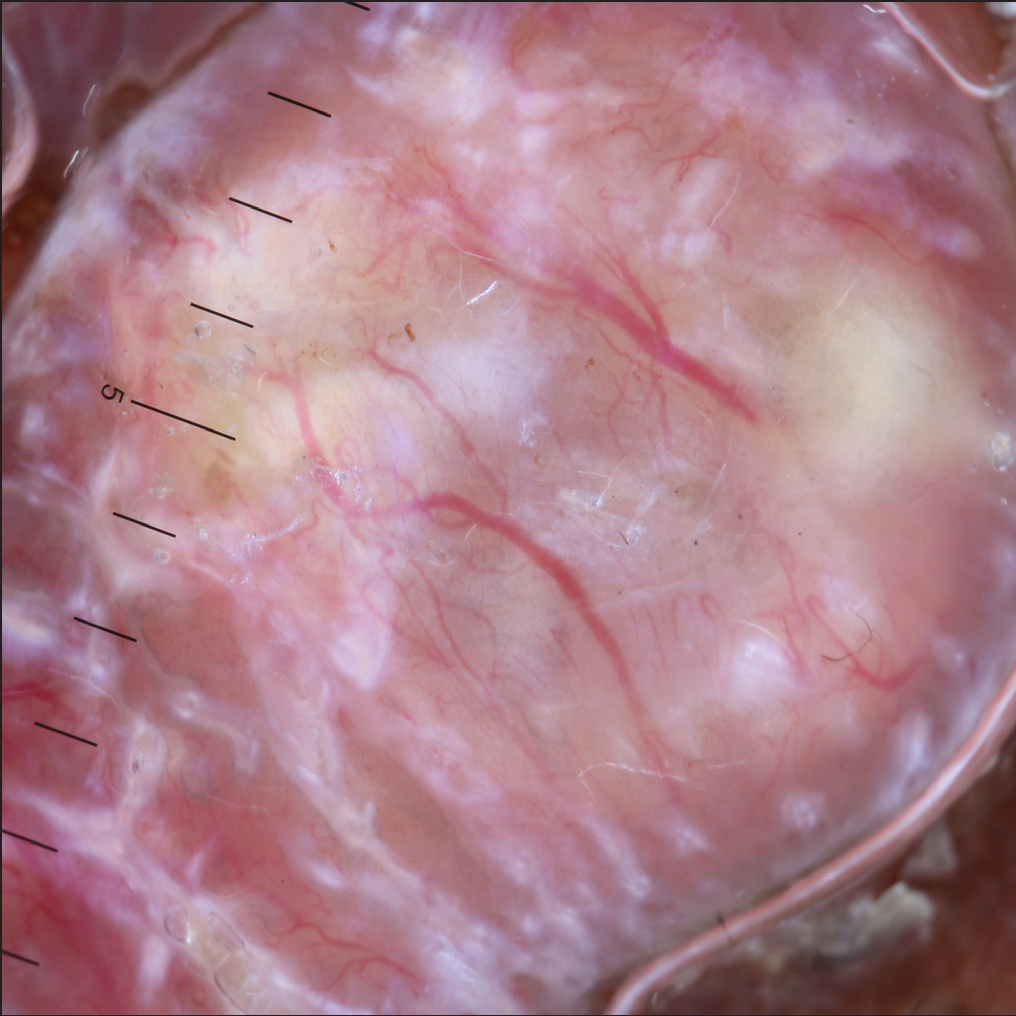
- Dermoscopy (DermLite DL4, ×10) shows yellow homogeneous areas, arborizing vessels and shiny white structures
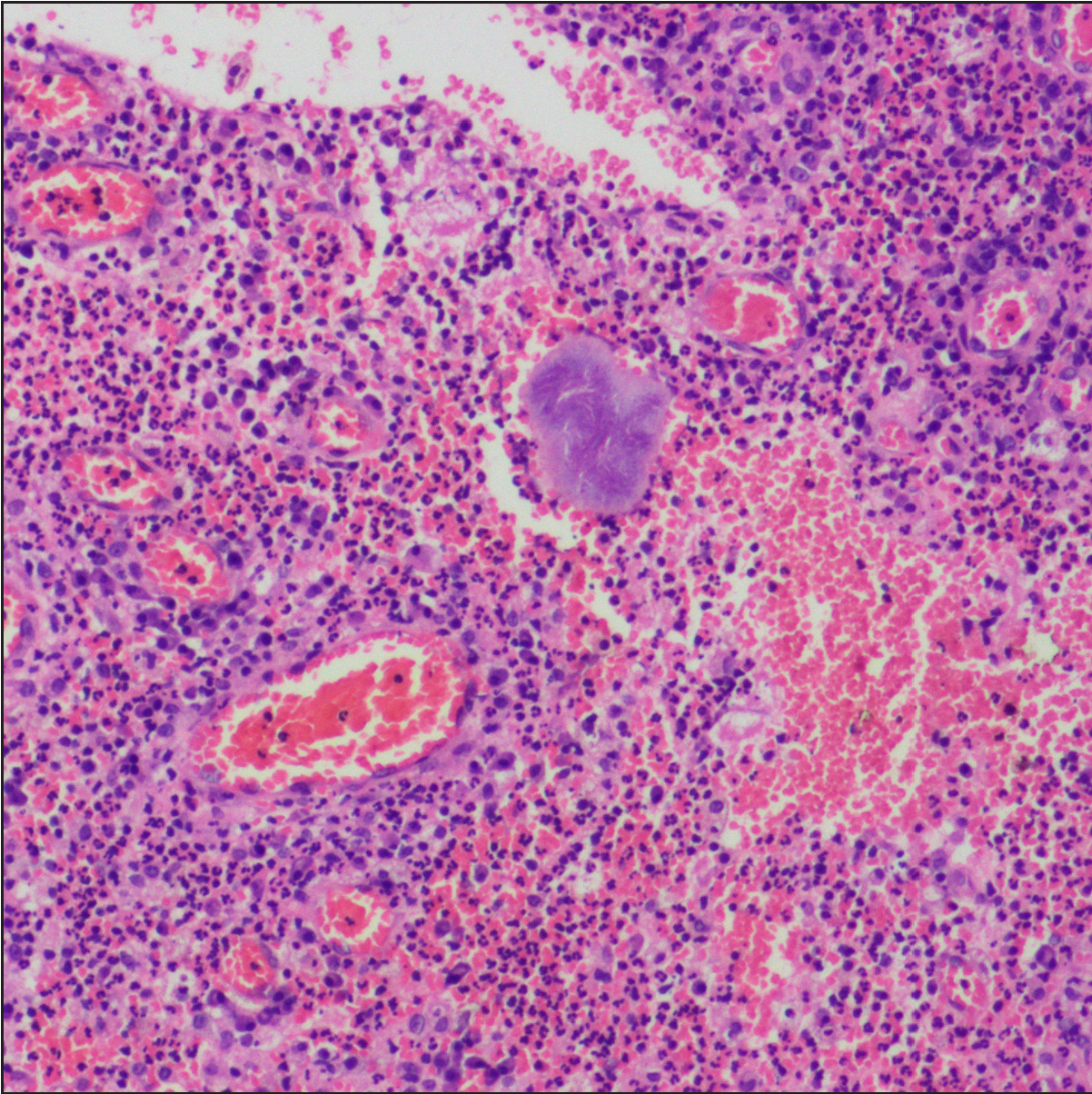
- Histopathology shows a granule with slender filaments radiating from the granule (Splendore-Hoeppli phenomenon) (H&E, ×400)

- Grocott Methenamine silver stain showed filamentous bacteria (H&E, ×400)

- Complete resolution of lesions after five months of treatment
Cervicofacial actinomycosis clinically manifests in three stages, initially presenting as soft swelling of the peri-mandibular area (stage 1), followed by woody hard induration and development of multiple sinus tracts and fistulas discharging purulent materials and sulphur granules (stage 2). Most patients with cervicofacial actinomycosis present in first or second stage. Later on, if left untreated, it can directly invade the cranium, or be disseminated hematogenously to involve the brain, lungs and abdominal cavity (stage 3).1 This classic presentation occurs in only 40% cases.2 Other presentations include chronic osteitis, osteolytic lesion, hard nodule on the tongue, lockjaw, para-apical or paradental abscess and tongue base ulcer.2,3 Rarely, they may spread from oral cavity to the tongue, larynx, trachea and salivary glands.4 In our case, the patient developed an atypical morphological presentation, mimicking “a bunch of grapes” without visible sinus or fistula. Reddy et al. described that discharging sinuses occur in 40% cases and suggested that they may be absent in patients with good host resistance, low virulence of the organism or subclinical disease.5 Kura et al. described a case of actinomycosis with multiple spongy papulo-vesicles and sessile nodules that mimicked lymphangioma circumscriptum due to a frog-spawn-like appearance.2
Tissue culture is the most accurate diagnostic modality, but is positive in only 30% cases. Histopathologically, diagnosis is based on the presence of suppurative and granulomatous infiltrates and granules, which is surrounded by eosinophilic areas. Sulphur granules are present in only 35–55% cases and are not pathognomic.1 Amoxicillin, clavulanic acid and minocycline are the first-line treatment options for penicillin-sensitive and penicillin-allergic patients, respectively. Carbapenems and tigecycline are used as second-line treatment options in severe cases. Treatment duration may range from 6 to 12 months.1 Our patient responded to the combination of amoxicillin/clavulanic acid and doxycycline with complete resolution in five months. The combination treatment was given to prevent resistance to amoxicillin.
We report this case due to its rare morphological presentation. A high degree of suspicion is needed to diagnose cervicofacial actinomycosis presenting as papulonodules in the absence of discharging sinuses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cervicofacial actinomycosis mimicking lymphangioma circumscriptum. Indian J Dermatol. 2011;56:321-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Atypical presentation of actinomycosis: A giant ulcer of the base of the tongue. Oper Tech Otolayngol Head Neck Surg. 2007;18:329-31.
- [Google Scholar]
- An atypical form of cervicofacial actinomycosis treated with short but intensive antibiotic regimen. BMJ Case Rep. 2013;2013:bcr2013008733.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A non-sinus forming mandibular actinomycotic osteomyelitis with a submandibular gland swelling–A case mimicking a periapical infection. J Evol Med Dent Sci. 2021;10:1741-6.
- [Google Scholar]





