Translate this page into:
Nailfold capillaroscopy as a prognostic marker for connective tissue diseases: An observational clinico-epidemiological study
Corresponding author: Dr. Chitra S. Nayak, Department of Skin and V.D., TNMC & BYL Nair Ch. Hospital, Mumbai, Maharashtra, India. chitra212@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Desai SA, Nayak CS. Nailfold capillaroscopy as a prognostic marker for connective tissue diseases: An observational clinico-epidemiological study. Indian J Dermatol Venereol Leprol. 2024;90:283-90. doi: 10.25259/IJDVL_205_2022
Abstract
Background
Nailfold capillaroscopy (NFC) is useful in the diagnosis and assessment of various connective tissue diseases. In this study, NFC findings were studied in patients of systemic sclerosis (SS), systemic lupus erythematosus (SLE) and dermatomyositis.
Aims
To study the nailfold capillaroscopic findings in patients with connective tissue disorders, their correlation with disease severity, and changes in findings following treatment or disease progression.
Methods
This observational prospective time-bound clinico-epidemiological study was conducted in 43 patients over 20 months at Topiwala National Medical College and BYL Nair Ch. Hospital, Mumbai. NFC was performed using the polarising mode of a USB 2.0 video-dermatoscope in all 10 fingernails at 50X and 200X. It was repeated at three follow-up visits to look for changes in findings.
Results
Among SLE patients, eleven (52.4%) had non-specific NFC patterns and eight (38.1%) had SLE patterns. Among systemic sclerosis patients, eight (42.1%) cases had active and late SS patterns respectively, while one (5.3%) each had SLE, non-specific and early SS patterns. After three follow-ups, 10 out of 11 (90.9%) cases with improvement in NFC also showed clinical improvement; this figure was significantly more than 11 out of 23 (47.8%) cases who had no change in NFC but showed clinical improvement. Two of the three dermatomyositis patients showed a non-specific pattern while one showed a late SS pattern at baseline.
Limitations
A larger sample size would have yielded results with more validity. Standardisation of the interval between baseline and last follow-up to equal to or more than six months would have yielded results with more accuracy.
Conclusion
Capillary findings change significantly over time and reflect changes in the clinical status of patients of both SLE and systemic sclerosis, and hence are an important prognostic marker. Rather than an overt change in NFC pattern, reduction or increase in abnormal capillaries is a better predictor of change in disease activity.
Keywords
Nailfold
capillaroscopy
scleroderma
Plain Language Summary
Autoimmunity is a phenomenon where the immune system reacts against cells of the body. Connective tissue disorders include an enormous spectrum of diseases caused due to autoimmunity. Some of the common heritable connective tissue disorders are systemic sclerosis, lupus erythematosus and dermatomyositis. Nailfold capillaroscopy (NFC) is a technique used in the diagnosis and assessment of these patients. A dermatoscope is a handheld instrument used for magnification (10X to 500 X) of subsurface structures. While performing NFC, this instrument is used to observe morphology of blood vessels at the proximal nailfold. These blood vessels are representative of the microvasculature elsewhere in the body and hence are altered in connective tissue disorders. This study was carried out to determine whether capillary findings change over time with clinical improvement or deterioration. Forty-three patients were included in this study and were followed up for a mean duration of six months. It was found that NFC findings change significantly over time and reflect changes in the clinical status of patients. Clinicians may perform NFC for diagnosis and at follow-up visits in patients with connective tissue disorders.
Introduction
Nailfold capillaroscopy (NFC), first performed by Sir Johan Christophorus Kolhaus using a rudimentary microscope, is an inexpensive, non-invasive and painless technique for studying proximal nailfold capillaries. The digital video capillaroscope represents the gold standard for assessing nailfold capillaries.1
NFC is useful to differentiate between the various connective tissue diseases as well as for their early diagnosis. The best-defined and most studied abnormalities are reported in patients with systemic sclerosis. However, there is a notable paucity of follow-up studies wherein changes in NFC findings were recorded over time.
For the purpose of this study, NFC patterns were studied in patients with systemic sclerosis, systemic lupus erythematosus and dermatomyositis. These were correlated with the clinical status of patients.
The aim was to study the NFC findings in patients with connective tissue disorders and their correlation with disease severity as follows:
To find the proportion of abnormal NFC findings in patients with systemic sclerosis, lupus erythematosus and dermatomyositis.
To study the NFC findings and correlate them with systemic manifestations of the disease.
To repeat NFC at follow-up visits to look for changes in findings with disease progression or response to treatment.
Methods
This observational prospective time-bound clinico-epidemiological study was conducted at the Department of Dermatology at Topiwala National College and BYL Nair Hospital, Mumbai, after taking approval from the institutional Ethics Committee. The study duration was 20 months and 43 patients were included.
Participants between the ages of 0 –70 years who fulfilled the 2013 American College of Rheumatology/ European League Against Rheumatism (ACR/EULAR) classification criteria for the diagnosis of Systemic sclerosis, the 2012 Systemic Lupus International Collaborating Clinics (SLICC) criteria for the diagnosis of SLE, or the Bohan and Peter criteria for the diagnosis of dermatomyositis were included. Patients who were not willing to give written informed consent were excluded.
A detailed history was taken and clinical examination was performed. Digital photographs were taken at baseline. Investigations necessary for the diagnosis and management of individual patients including serological tests were advised. In the case of already diagnosed cases, the pre-existing findings were recorded. Nailfold dermoscopy was performed using the polarising mode of a USB 2.0 video–dermatoscope (Dinolite AM4132T, 20–220X; 1.3MP) in all 10 fingernails with liquid paraffin as linkage fluid and images were taken using the computer software. Capillary changes were first observed at 50X and then at 200X. Images were stored, and interpreted by two independent observers. NFC was repeated at three follow-up visits to look for changes in findings. The frequency of follow-up visits was monthly, which is the standard for follow-up. However, if some patients defaulted, NFC was performed at the next visit.
At each visit including baseline, patients were grouped into four categories (1) Active, treatment naïve, (2) Active on treatment, (3) Stable on treatment, (4) Burnt out, not on treatment. Changes in disease activity were correlated with changes in nailfold capillaroscopy findings. Statistical analysis was carried out using the statistical package for social sciences version 20. The age and sex distribution of patients were studied. The most common capillary abnormalities overall as well as in SLE and systemic sclerosis patients separately were determined. The association of change in NFC abnormalities at the third follow-up with concomitant clinical changes was determined by Fisher Exact test and P-value <0.05 was considered significant. Similarly, the association of change in NFC pattern at the third follow-up with congruent clinical change was determined using Fisher Exact test.
Results
The mean age of patients was 33 years. Out of 43, only two were males while 41 were females. Out of the 21 patients with SLE, 11 (52.4%) had non-specific NFC patterns and eight (38.1%) had SLE NFC patterns. Among the systemic sclerosis patients, eight (42.1%) had active and late SS patterns each, while one (5.3%) each had SLE, non-specific and early SS patterns. Overall, the most common capillary abnormality was dilated capillaries seen in 301 (70%) of the examined nails, followed by avascular areas in 189 (44%), and tortuous capillaries in 138 (32.1%). The association of clinical improvement with improvement in NFC was studied. Out of the 11 cases that had improvement in NFC, 10 (90.9%) also showed clinical improvement while out of the 23 cases that had no improvement in NFC, only 11 (47.8%) showed clinical improvement [Figure 1]. This difference was statistically significant (P = 0.02). The association between clinical changes and changes in NFC patterns was also studied. Among the eight cases that showed a change in NFC pattern, seven (87.5%) cases showed clinical improvement, while out of the 35 patients who had no change in the pattern of NFC, 22 (62.9%) showed clinical improvement [Figure 2]. The difference was not statistically significant.
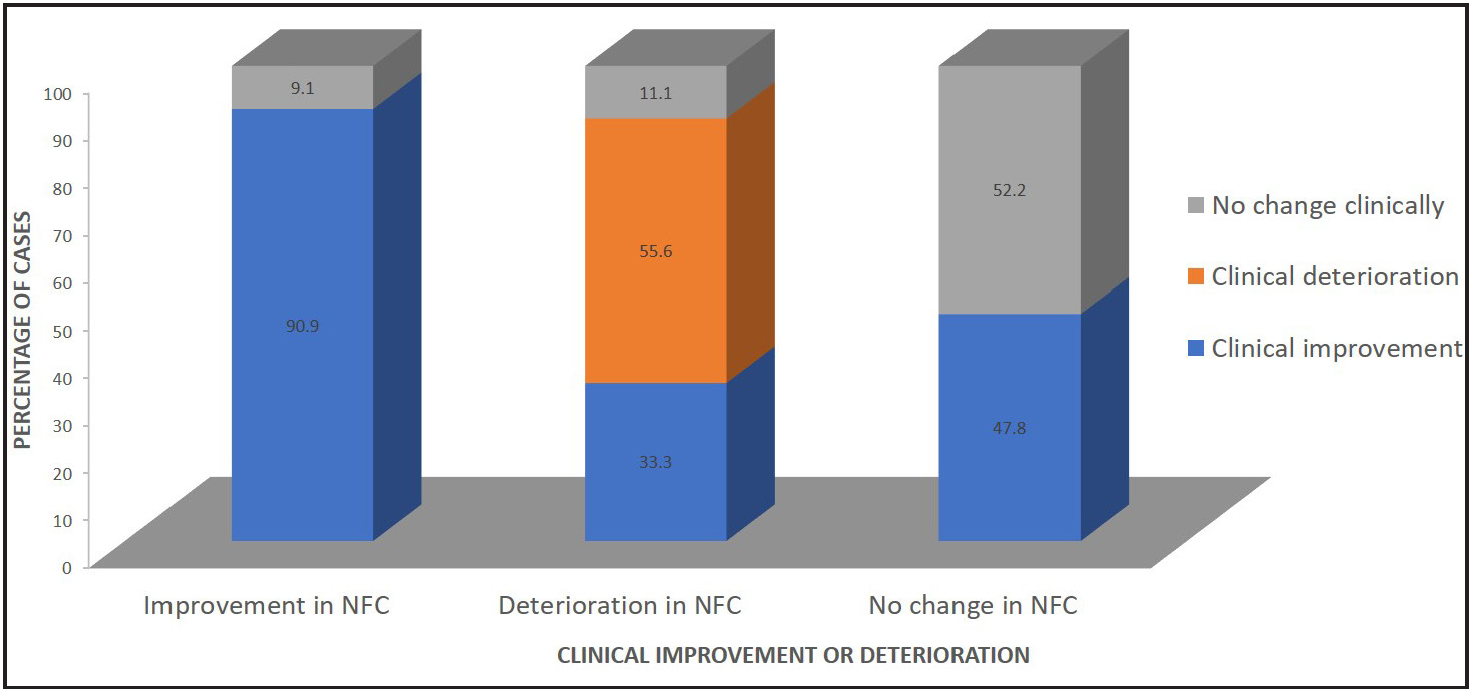
- Association of clinical improvement or deterioration at third follow-up with NFC findings in all patients
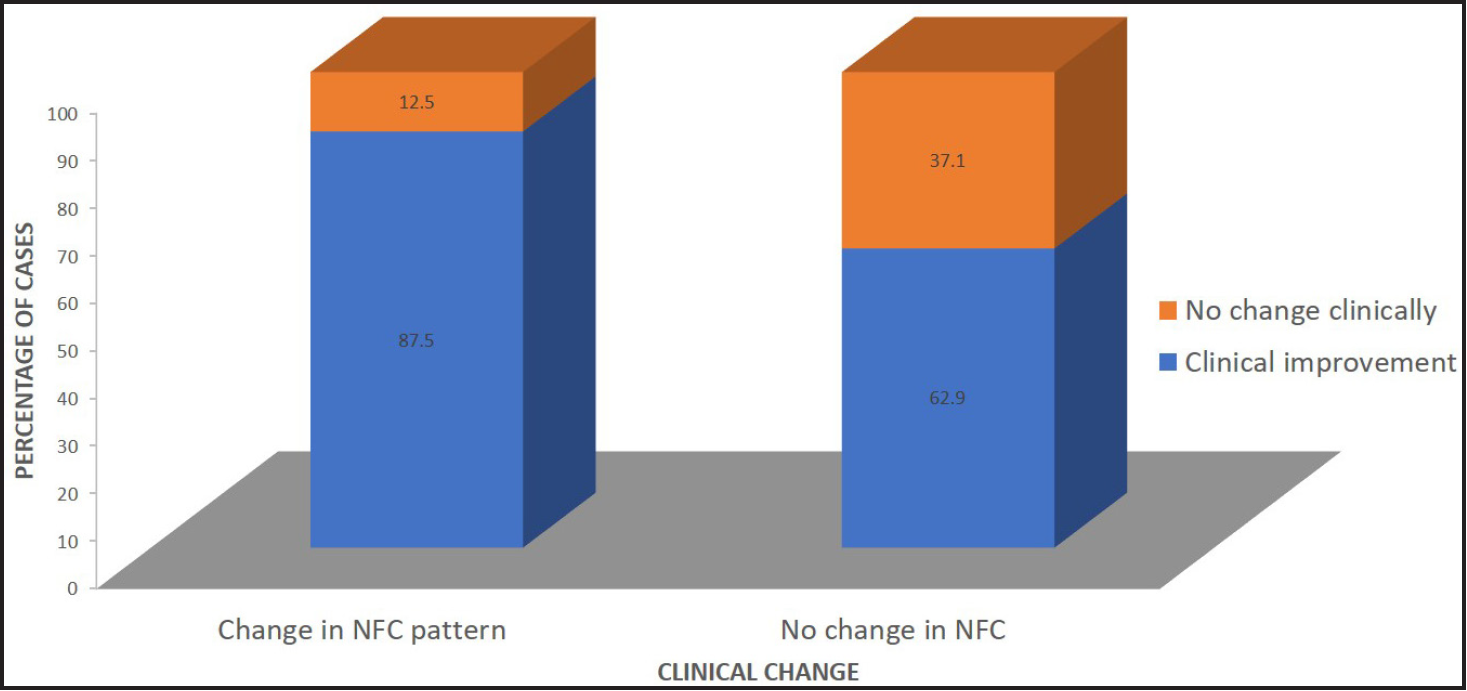
- Association of change in NFC pattern with concomitant clinical change
There were only three patients with dermatomyositis in our study. Two of them showed a non-specific pattern while one showed a late SS pattern at baseline. We could not perform statistical analysis on these patients due to the small sample size.
Discussion
Nailfold capillaroscopy (NFC) is an inexpensive, non-invasive, and safe technique for studying proximal nailfold capillaries. The special morphologic feature of the nailfold distal capillary row is that dermal papillae run parallel to the surface of the nail. Hence, the capillaries of the distal row are visible throughout their whole length.2,3 The digital video capillaroscope is the gold standard for assessing capillary morphology.2
NFC is being recognised not just as a diagnostic marker but also for its prognostic value and utility in therapeutic follow-up of patients with scleroderma. Capillaroscopy is now officially considered by the EULAR and ACR guidelines as an essential and mandatory diagnostic tool. This is after the study by Lonzetti et al. which proved that NFC improved the sensitivity of ACR criteria for the diagnosis of systemic sclerosis from 67 to 99%.4
The third or fourth finger is preferred for NFC due to the high transparency of the skin. Cedarwood oil, liquid paraffin or even ultrasound gel can be used as a medium in the polarised method. The whole surface of the nail is visible at 10X magnification, but higher magnifications provide better visualisation.5 We studied nailfold capillaries using 50X and 200X magnifications. A normal capillaroscopic pattern is characterised by the homogenous distribution of hairpin-shaped capillaries in a comb-like pattern, with a density of 9–14 per mm.6–9 However, there is a wide intra- and inter-individual variability within the normal population, and even 6–9 capillaries is considered normal in Indians as darkly pigmented skin impairs the visibility of capillaries.10,11
Many previous studies have been conducted to define nailfold capillary abnormalities in connective tissue disorders.11–13 Those observed by us in the studied population included tortuous, meandering, dilated and giant capillaries as well as capillary dropouts, avascular areas and microhaemorrhages.
A capillaroscopic feature is generally considered abnormal if changes are observed in at least two fingers.14 Tortuosity and microhaemorrhages are seen even in the normal populations, in about 22% and 14%, respectively.11 Dilated and giant capillaries, however, are suggestive of early microvascular injury and should alert the physician.
NFC patterns were first defined for scleroderma by Cutolo et al.15 The capillaroscopic findings in our study were studied and categorised into one out of six existing patterns at each visit:
Normal pattern - homogeneously aligned capillary plexus with 30 capillaries per 5 mm, no morphological alterations.
Early SS - limited number of giant capillaries, rare microhaemorrhages, with normal-shaped capillaries and relatively well-preserved capillary distribution, without loss of capillaries.
Active SS - numerous giant capillaries, frequent microhaemorrhages, moderate reduction in capillary density, mild disorganisation of architecture and no ramified capillaries.
Late SS - marked loss of capillaries, extensive avascular areas, ramified or bushy neo-angiogenesis, disorganised vascular array.
SLE pattern - tortuous loops, dilated capillaries, greater visibility of the sub-capillary venous plexus.5
Non-specific pattern.
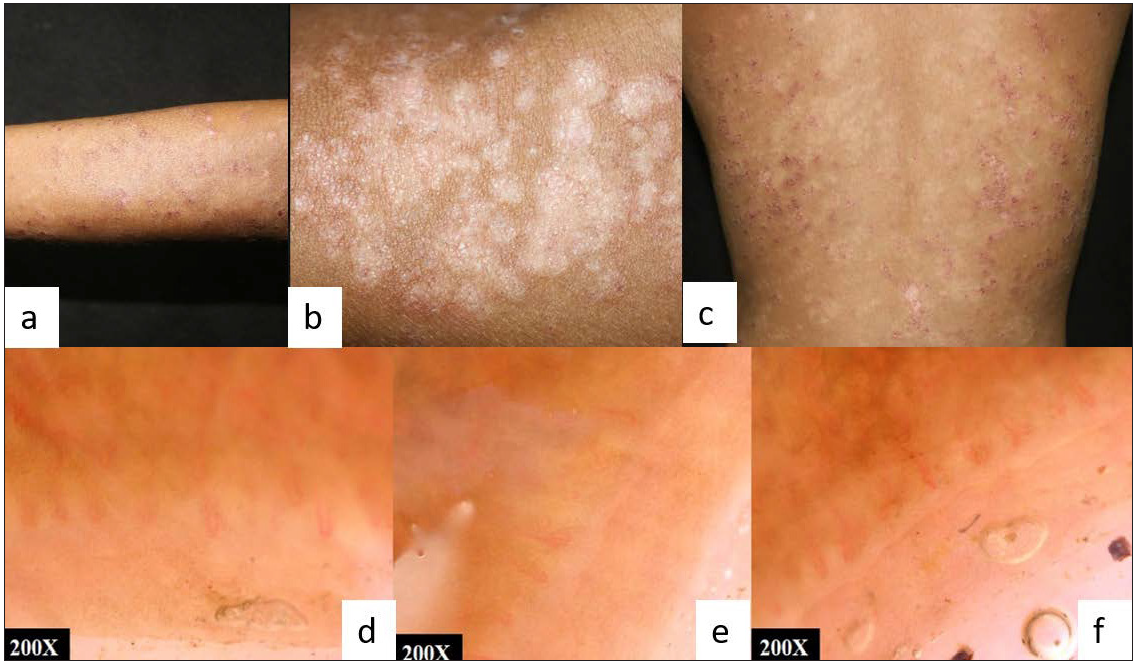
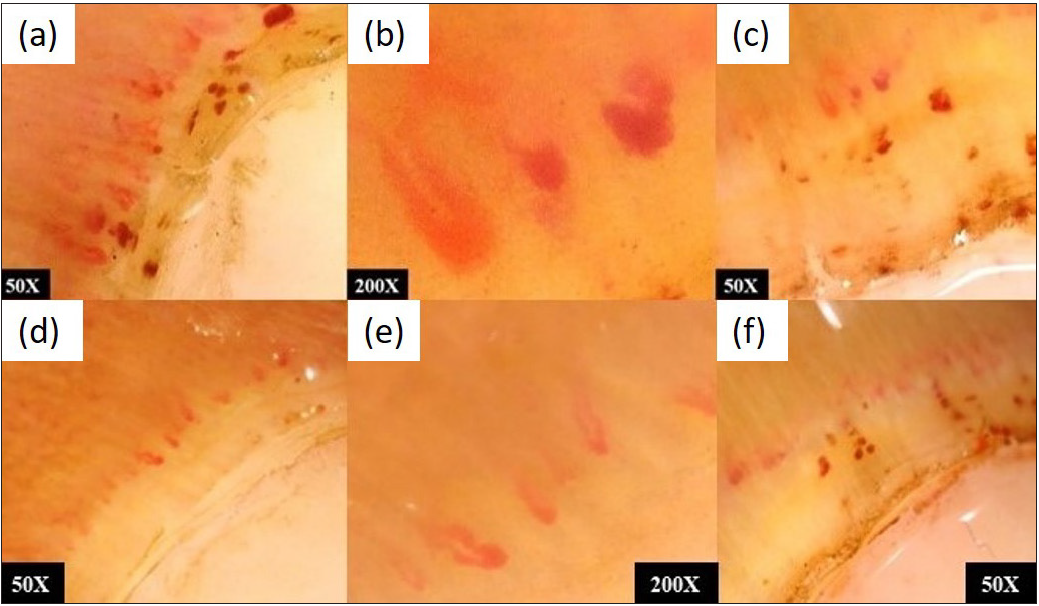
- (a,b,c) SLE with papulosquamous SCLE like lesions at baseline; (d,e,f) NFC showing few dilated capillaries and reduced capillary density in non-specific pattern
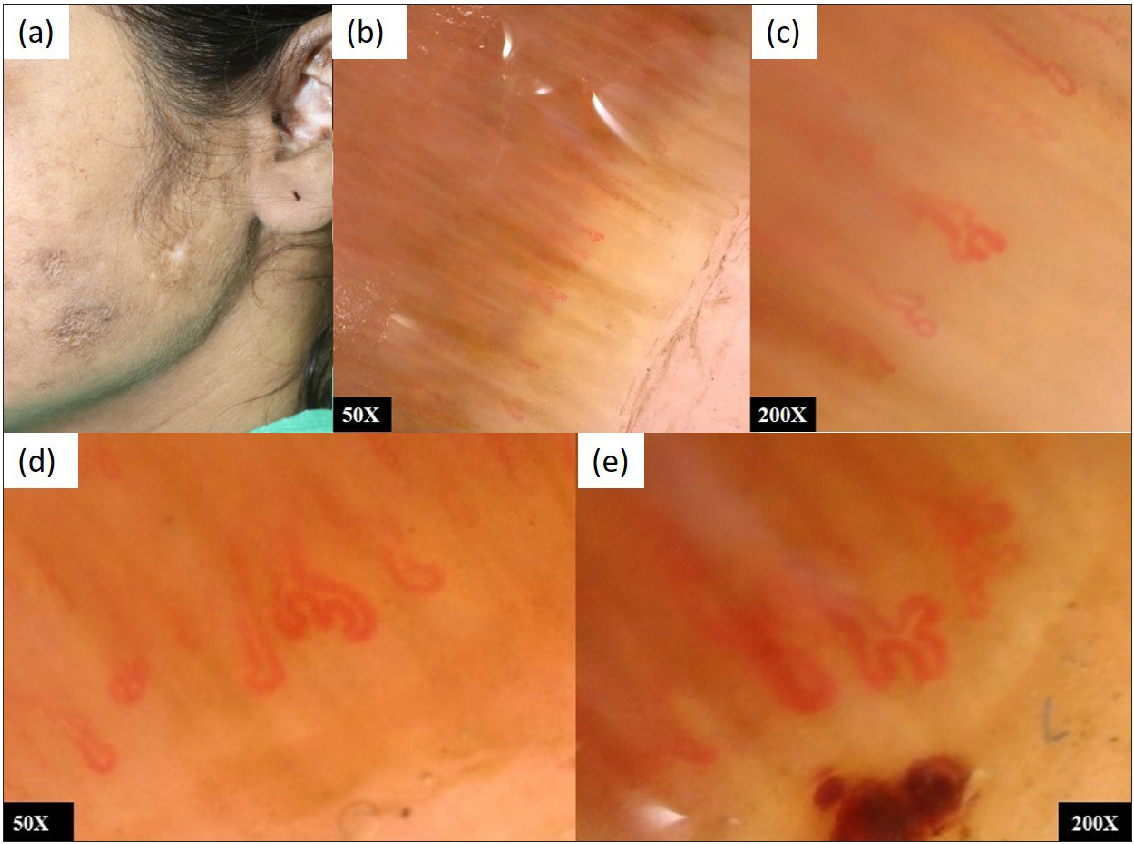
- (a) SLE with discoid lupus erythematosus (DLE); (b,c) NFC showing elongated, dilated, tortuous capillaries, suggestive of SLE pattern. (d,e) Increased dilatation and tortuosity of capillaries after 6 months with the progression of the disease
Nineteen patients with systemic sclerosis were included in our study; all had abnormalities on NFC. Many previous studies15,18,19 have estimated the prevalence of NFC abnormalities in systemic sclerosis patients to be above 90%. Eight (42.1%) of the cases in our study had active [Figure 5] and late SS [Figure 6] patterns while one (5.3%) each had non-specific and early SS patterns. These patterns were concomitant with the clinical picture of patients. In our study, the most common capillary abnormality detected was dilated capillaries seen in 301 (75.8%) nails, followed by avascular areas in 189 (56.8%) nails, tortuous capillaries in 138 (32.1%), capillary haemorrhages in 69 (31.6%) and capillary dropouts in 47 (22.1%).
- (a,b,c) A patient of diffuse cutaneous systemic sclerosis-NFC showing active pattern with capillary haemorrhages and giant capillaries. (d,e,f) Reduced number of giant and dilated capillaries, fewer microhemorrhages following treatment with methotrexate

- (a,b) Diffuse systemic sclerosis showing sclerodactyly, resorption of phalanges, Ingram’s sign, mat-like telangiectasias on face; (c,d) NFC showing few dilated tortuous capillaries and multiple avascular areas suggestive of late SS pattern. (e,f) NFC showing larger avascular areas and fewer dilated capillaries showing further deterioration without change in pattern
The NFC changes were recorded at three follow-ups. The interval between follow-ups was variable as patients often followed up late, but in 25 patients out of 43 (58.13%), the last follow-up was conducted at six months or later from baseline. A modified Rodnan scoring system was used for all systemic sclerosis patients at each visit.
In our study, patients were divided into four categories at each visit - treatment naïve active, active on treatment, stable on treatment and burnt-out. All were either on treatment with immunosuppressants, or treatment was started after baseline evaluation for new patients. All systemic sclerosis patients were given telmisartan, along with methotrexate in eight patients and cyclophosphamide in nine patients. Two patients were given azathioprine. Three patients on cyclophosphamide also received aspirin for impending digital gangrene. For SLE patients, hydroxychloroquine and azathioprine were used. Two patients had been administered rituximab. The treatment was given on a case-to-case basis and no specific protocol was followed. Thirty patients (69.76%) had active disease at baseline, while only 15 (37.2%) did at the end of the study (P = 0.008, chi-square test). Therefore, treatment with immunosuppressants improved the clinical status of the patients significantly. Clinical improvement was determined in terms of the resolution of skin lesions, symptomatic improvement and improvement of laboratory parameters.
The association between clinical change and change in NFC pattern was studied [Figure 1]. Seven out of eight patients who had changed in NFC pattern also showed concomitant clinical change. In thirty-five patients, the NFC pattern remained stable, but twenty-two of these showed clinical change (P = 0.24, Fisher’s exact test). Therefore the variation between NFC pattern changes and clinical parameters was not significant.
Figure 7 shows a case of diffuse systemic sclerosis with salt and pepper pigmentation, NFC showing dilated capillaries and haemorrhage suggestive of active SS pattern at baseline, while NFC at the third follow-up shows dilated capillaries and large avascular areas suggestive of late SS pattern.

- (a,b) Diffuse systemic sclerosis with salt and pepper pigmentation; (c,d) NFC at baseline showing dilated capillaries and haemorrhage suggestive of active SS pattern; (e,f) NFC of the same patient at third follow-up showing fewer dilated capillaries and large avascular areas suggestive of late SS pattern
However, NFC findings were also evaluated based on subjective assessment of increase or decrease in abnormal capillaries without obvious change in pattern, recorded by the same clinicians at follow-up visits. Out of 11 patients who had improvement in NFC, 10 (90.9%) showed clinical improvement in terms of reduced symptoms, improved laboratory parameters, reduced frequency of Raynaud’s attacks, and improved modified Rodnan skin score (mRSS) in cases of systemic sclerosis. One patient remained clinically stable. Out of 23 patients who had no significant change in NFC findings, only 11 (47.8%) showed clinical improvement [Figure 2]. Fisher exact test was applied to find an association between improvement in NFC findings and clinical findings, and P-value was found to be 0.023, i.e., significant. Nine patients showed deterioration in NFC, and five of these had recalcitrant disease despite treatment.
Thus, there were ten patients who improved clinically with immunosuppressant therapy and also showed a reduction in dilated capillaries, capillary haemorrhages and tortuous capillaries on NFC. These parameters were recorded quantitatively. NFC patterns are, as of now, defined qualitatively by the type of capillary abnormalities. So, not all patients with quantitative changes on NFC demonstrated an overt change in pattern.
The nine patients whose NFC findings worsened over time showed an increase in the number of dilated capillaries, capillary haemorrhages, tortuous capillaries or capillary dropouts and avascular areas. None of the patients with late SS patterns at baseline could be seen reverting back to active, early or normal patterns even after clinical improvement. However, some of them did show new capillaries at previously avascular areas over one year. This implies that capillary regeneration is possible even in advanced cases of systemic sclerosis, but the process takes long.
Figure 8a shows a case of SLE with NFC showing SLE pattern at baseline. Figure 8b shows clinical improvement at one-year follow-up, with NFC showing a reduction in abnormal capillaries and avascular areas.
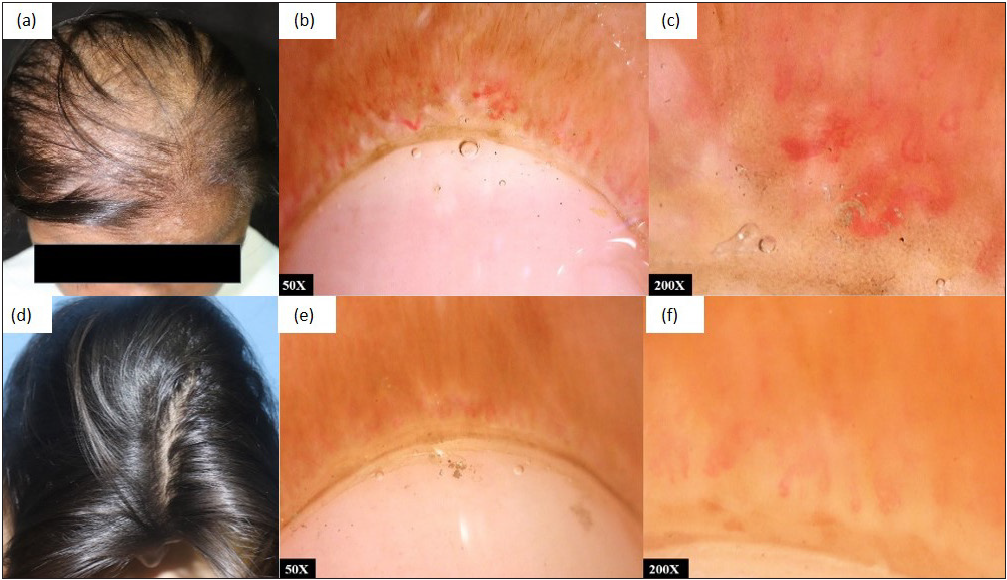
- (a) SLE with diffuse alopecia, (b,c) NFC showing dilated tortuous vessels and avascular areas suggestive of SLE pattern at baseline; (d) Clinical improvement at 1 year follow-up, (e,f) NFC showing reduction in abnormal capillaries and avascular areas
This implies that clinical improvement also reflects in NFC findings, and NFC may be used as an important prognostic indicator, not just for systemic sclerosis but also for SLE. Rather than an overt change in NFC pattern, a reduction or increase in the number of abnormal capillaries is a better predictor of change in disease activity.
However, this being a subjective assessment, there is considerable inter-personal variation and NFC should be performed by the same clinician at each visit. Thus, there is a need to develop a simple NFC scoring system. The only present score is the one suggested by Cutolo et al. [Table 1]19 This scoring system was used by Sully et al.20 in 90 systemic sclerosis patients, following them up over a period of 72 months. At the end of the follow-ups, the score for each capillary abnormality changed significantly despite no change in NFC patterns. The mean score for each capillaroscopic parameter is calculated from the analysis of four consecutive fields (each of 1 linear millimetre) in the middle of the nail fold in each digit; the average scores from the eight digits are added together, and the final value divided by eight
Score
Morphology
0
No changes
1
<33% capillary alterations/reduction
2
33–66% capillary alterations/reduction
3
33–66% capillary alterations/reduction
Owing to the complexity of this system, there is a dire need to employ a simple and more reproducible scoring system for NFC, not just for systemic sclerosis but also for SLE.
The fact that microangiopathy in systemic sclerosis is an evolving process and is quantifiable by NFC has been proven in multiple studies.15,21 However, there are still lacunae in our knowledge about its correlation with clinical parameters. Long-term follow-up studies are required in this regard. Though there is a dearth of follow-up studies evaluating NFC findings in SLE, there are multiple cross-sectional studies assessing the correlation of active disease with higher NFC scores.22,23 Regular and meticulous documentation of NFC at follow-up visits should be incorporated into routine practice.
Limitations of the study included small sample size and lack of standardisation of the interval between baseline and last follow up.
To conclude, NFC findings change significantly over time and reflect a change in the clinical status of patients with systemic sclerosis and SLE. Hence they are an important prognostic marker and should be monitored regularly, at least every six months.
Rather than an overt change in pattern, a reduction or increase in abnormal capillaries is a better marker for disease activity. Here, a simple NFC score to monitor over time will be valuable. It will also allow for NFC to be performed by different clinicians at follow-up visits.
NFC is being used commonly as a diagnostic marker for connective tissue disorders. But our study prompts clinicians to inculcate the practice of performing and recording NFC at follow-up visits, and thus demonstrates its prognostic utility. There is a need to conduct long-term follow-up studies correlating changes in NFC with clinical changes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical and autoimmune profile of scleroderma patients from Western India. Int J Rheumatol. 2014;2014:983781.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Capillaroscopy and the measurement of capillary pressure. Br J Clin Pharmacol. 2000;50:501-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- How to perform and interpret capillaroscopy. Best Pract Res Clin Rheumatol. 2013;27:237-48.
- [CrossRef] [PubMed] [Google Scholar]
- Updating the American College of Rheumatology preliminary classification criteria for systemic sclerosis: Addition of severe nailfold capillaroscopy abnormalities markedly increases the sensitivity for limited scleroderma. Arthritis Rheum. 2001;44:735-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy in the evaluation of nail disorders. Skin Appendage Disord. 2017;3:70-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quantitative nailfold capillaroscopy findings in a population with connective tissue disease and in normal healthy controls. Ann Rheum Dis. 1996;55:507-12.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillaroscopy by digital microscope in an Indian population with systemic sclerosis. Int J Rheum Dis. 2012;15:95-101.
- [CrossRef] [PubMed] [Google Scholar]
- Panoramic nailfold capillaroscopy: A new reading method and normal range. Semin Arthritis Rheum. 1990;20:21-31.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative and quantitative assessment of nailfold capillaries by capillaroscopy in healthy volunteers. Vasa. 2012;41:19-26.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2002;16:847-58.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillaroscopy with USB dermatoscope: A cross-sectional study in healthy adults. Indian J Dermatol Venereol Leprol. 2020;86:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillary microscopy in the connective tissue diseases: A semiquantitative assessment. J Rheumatol. 1983;10:930-8.
- [PubMed] [Google Scholar]
- Nailfold capillaroscopy in rheumatic diseases: Which parameters should be evaluated. BioMed Res Int. 2015;2015:974530.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of nail video-capillaroscopy in early diagnosis of scleroderma. Autoimmun Rev. 2013;12:821-5.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold video-capillaroscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol. 2000;27:155-60.
- [PubMed] [Google Scholar]
- Capillaroscopy findings in lupus erythematosus. Anais brasileiros de dermatologia. 2006;81:523-28.
- [Google Scholar]
- Nailfold capillaroscopic changes in patients with systemic lupus erythematosus: Correlations with disease activity, skin manifestation and nephritis. Lupus. 2017;26:959-66.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of nailfold capillaroscopy in the diagnosis of connective tissue diseases. Clin Rheumatol. 1996;15:148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Scoring the nailfold microvascular changes during the capillaroscopic analysis in systemic sclerosis patients. Ann Rheum Dis. 2008;67:885-7.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term follow-up of nailfold videocapillaroscopic changes in dermatomyositis versus systemic sclerosis patients. Clin Rheumatol. 2018;37:2723-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular endothelial growth factor in systemic lupus erythematosus in correlations with disease activity and nailfold capillaroscopic changes. Egypt J Intern Med. 2019;31:943-50.
- [Google Scholar]
- Evaluation of nailfold videocapillaroscopic abnormalities in patients with systemic lupus erythematosus. JCR. J Clin Rheumatol. 2005;11:295-8.
- [CrossRef] [PubMed] [Google Scholar]






