Translate this page into:
Contact hypersensitivity to Indian standard patch test series correlates with disease severity among children with atopic dermatitis
Corresponding author: Dr. Rajsmita Bhattacharjee, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh, India. rajsmita.bee@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Handa S, Bhattacharjee R, Thakur V, De D, Mahajan R. Contact hypersensitivity to Indian standard patch test series correlates with disease severity among children with atopic dermatitis. Indian J Dermatol Venereol Leprol. 2024;90:46-51. doi: 10.25259/IJDVL_492_2022
Abstract
Background
There is emerging evidence of a relationship between atopic dermatitis (AD) and allergic contact dermatitis (ACD), though the data available are scarce with conflicting viewpoints. We explored the occurrence of contact hypersensitivity among children with atopic dermatitis by patch testing them with the Indian standard series and tried to correlate the presence of contact hypersensitivity with the clinical severity of AD in these children.
Methods
In this single-centre, cross-sectional study, children between 6 months and 12 years diagnosed with atopic dermatitis were included and patch tested with the Indian standard series. Outcome parameters were the proportion of patients having positive patch-test reactions, the proportion of positive patch-test reactions for each allergen and factors associated with patch test positivity in atopic dermatitis.
Results
Of the 136 patients, 80 were boys. The mean age of the study population was 5.6 ± 3.2 years. Twenty-eight (20.6%) patients had patch test positivity at 96 h. Fragrance mix was the commonest allergen, followed by potassium dichromate, cobalt chloride hexahydrate and nickel. SCORing atopic dermatitis (SCORAD) was significantly higher in patients with positive patch tests as compared to patients with negative patch tests (P = 0.009).
Conclusion
Greater disease severity in atopic dermatitis was found to be associated with patch test positivity.
Limitations
Inability to establish relevance in about 50% of the patients was a limitation of our study. Follow-up data regarding the impact of allergen avoidance is not available.
Keywords
Atopic dermatitis
contact dermatitis
paediatric
patch test
Key Message
In this study, nearly one-fifth (20.6%) of children with atopic dermatitis had a positive patch test. The most common allergens were fragrance mix, potassium dichromate, cobalt and nickel. Greater disease severity was associated with patch test positivity.
Plain Language Summary
In this study, we tried to analyse the association between eczema in children and certain common allergy inducing chemicals present in various items of daily life, by means of a simple, non-invasive office-based patch test. We found that nearly one-fifth (20.6%) of children with eczema had a positive result. The most common allergens were those found in fragrances and cement as well as metals such as nickel and cobalt.
Introduction
There is a complex, though yet not fully understood relationship between atopic dermatitis (AD) and allergic contact dermatitis (ACD). Immunologic pathways, influenced by both genetic and environmental triggers, contribute to the development of both conditions. There is emerging evidence supporting the existence of a substantial relationship between them, though the data available are scarce with conflicting viewpoints. Predisposing factors such as deficiency in filaggrin, altered pH, the cutaneous acid mantle, microbial colonisation by Staphylococcus aureus and low vitamin D levels contribute to the immunopathogenesis and elicitation of both atopic dermatitis and allergic contact dermatitis. It is important to diagnose contact dermatitis (CD) in patients with atopic dermatitis as atopy amplifies the effects of contact irritants and allergens on the skin. This is seen with hand eczema in adult patients with atopic dermatitis in certain occupations (hairdressers, cleaners, metalworkers, mechanics and nurses). Contact sensitization may negatively influence the skin of atopic dermatitis patients; therefore, identifying an aggravating factor, such as a contact allergen, and avoidance of the allergen can lead to the improvement of dermatitis.1
Contact allergy is common in both children and adults and may affect up to 20% of the general population.2 Among the commonly implicated contact allergens, metals, fragrance materials and preservatives are found in commonly used products such as cosmetics and jewellery. Another important consideration in atopic individuals is that topical therapy is inevitably prescribed, often for longer periods to inflamed skin resulting in near continuous exposure. While experimental models provide some insights into a possible interplay between contact allergy and atopic dermatitis, they do not and cannot simulate real-time human exposure. Hence, epidemiological studies have so far been unable to provide definitive conclusions on the possible relationship between atopic dermatitis and contact allergy.
Thus, this study was conducted to detect the frequency of contact hypersensitivity to Indian standard series among children with atopic dermatitis by patch testing and to correlate the clinical disease severity with the contact hypersensitivity observed in these children.
Methods
This was a single-centre, cross-sectional study conducted in the Paediatric Dermatology clinic of the Postgraduate Institute of Medical education and Research (PGIMER) in Chandigarh, North India, between April 2017 and September 2018 after obtaining approval from the institute’s ethics committee. Written informed consent was taken from the parents. Children aged between 6 months and 12 years diagnosed with atopic dermatitis according to Hanifin and Rajka criteria were included. These children did not have any contraindication to patch testing and had controlled disease, such that the back and the forearms were free from active dermatitis and suitable for application of test patches. Children aged < 6 months and > 12 years; immunocompromised children; those with severe exacerbation of the disease and active dermatitis; patients on oral corticosteroid equivalent to or more than 15 mg of prednisolone (arbitrarily defined as 0.25 mg/kg/day) or equivalent doses of steroid-sparing adjuvant drugs; those with dermatitis at the test site, i.e., upper back; inability to adhere to instructions including three visits over 1-week period and to keep patch test in place till last reading is taken; and those whose parents did not consent to their child’s inclusion in the study were excluded. Detailed history was recorded regarding the duration of symptoms, extent of symptoms, aggravating and relieving factors, treatment and family history. Clinical examination was performed inclusive of severity grading using SCORAD scores for all patients at the time of recruitment. The severity of eczema was graded according to the SCORAD index as mild (<25), moderate (26–50) and severe (>50) atopic dermatitis. Serum IgE levels were also measured before patch testing in all patients.
Methodology of patch testing
Aluminium chambers filled with allergens of the Indian standard series (ISS) were applied over the upper back. The patches were kept in place undisturbed for at least 48 h. Patients and their caregivers were instructed to avoid vigorous movements, stretching, shower and sunlight exposure. Patches were removed after 48 h, and the patch test sites were marked with gentian violet with the help of an applicator and a preliminary reading at 48 h was done. One more reading was taken at 96 h. Long- and short-acting anti-histamines or other immunosuppressive medications were discontinued for at least a fortnight before patch testing and withheld till 96 h after the test.
Outcome parameters
The primary objective was to detect the presence of contact hypersensitivity to allergens of the Indian standard series among children with atopic dermatitis by patch testing and to study the clinical settings in which contact hypersensitivity is seen in these children. Positive patch-test (PPT) reactions included any reaction from macular erythema to a 3+ reaction as defined by the International Contact Dermatitis Research Group. Percentage of positive patch test (PPT %) reactions were defined for each allergen as the sum of patients who have a positive reaction divided by the total number of patients patch tested for that specific allergen.
Interpretation of the results or definition of hypersensitivity based on patch reading
The results (days 2 and 4 readings) for each test site were recorded according to International Contact Dermatitis Research Group criteria, viz. (−) negative, (?) doubtful reaction, faint erythema only, (+) weak positive reaction; palpable erythema, infiltration possibly papules (non-vesicular), (++) strong positive reaction; erythema, infiltration, papules and vesicles (oedematous or vesicular), (+++) extreme reaction; intense erythema infiltration and coalescing vesicles (bullae or ulceration) and IR - irritant reaction of various types. The patch test was considered to be positive if any one reading was recorded as 1+ or higher. The relationship between patch test positivity and severity of atopic dermatitis was assessed.
Statistical analysis
Statistical analysis was carried out using Statistical Package for Social Sciences (SPSS version 25.0, IBM Corp., Armonk, NY, U.S.A.). The normalcy of continuous data was checked using the Kolmogorov–Smirnov Test. Mean and standard deviation (SD) were calculated for all normally distributed continuous variables. For non-normally distributed continuous variables, median was calculated. Qualitative or categorical variables were described as frequencies and proportions. ANOVA test was applied to compare the mean of continuous data. Categorical or qualitative variables were analysed using a chi-square test between individual groups.
Results
Out of totally 136 patients, 80 were boys. The mean age of the study population was 5.6 + 3.2 years. The youngest child was 11-months old, and 18 children were aged 2 years or less. The mean duration of disease was 33.6 + 28.5 months. The mean SCORAD of the study population was 21.6 + 11.6. According to SCORAD, the severity of atopic dermatitis was mild in 71, moderate in 54 and severe in 11 patients. Atopy was seen in 32 (23.5%) patients. Topical corticosteroids were prescribed in 111 (81.6%) patients and topical tacrolimus in 85 (59.6%). Systemic therapy including oral corticosteroids, cyclosporine and azathioprine was given to only six (4.4%) patients. Raised serum IgE was observed in 104 (76.5%) patients, and the mean serum IgE of the study population was 1395.2 + 3257.7 IU/mL. Clinicodemographic characteristics of the study population are summarised in Table 1.
| Parameter | Number of patients (n) = 136 |
|---|---|
| Age; in years (Mean + SD) | 5.6 + 3.2 |
| Gender (M: F) | 80:56 |
| Duration of disease; in months (Mean + SD) | 33.6 + 28.5 |
| SCORAD (Mean + SD) | 21.6 + 11.6 |
| SCORAD severity | |
| Mild | 71 |
| Moderate | 54 |
| Severe | 11 |
| Atopy; number of patients (%) | 32 (23.5) |
| History of allergy; number of patients (%) | 3 (2.2) |
| Medications; number of patients (%) | |
| Topical corticosteroids | 111 (81.6) |
| Topical tacrolimus | 85 (59.6) |
| Systemic therapy (steroids, cyclosporine, azathioprine) | 6 (4.4) |
| Emollients only | 5 (3.7) |
| Serum IgE (Mean + SD), IU/ml | 1395.2 + 3257.7 |
| Raised serum IgE; number of patients (%) | 104 (76.5) |
SCORAD: SCORing atopic dermatitis
Of the 136 patients, 24 (17.6%) patients had positive patch tests at 48 h while 28 (20.6%) patients had patch test positivity at 96 h. Eleven (8.1%) patients had positive patch tests with > 2 allergens. Among patients with patch test positivity at 48 h, fragrance mix was the commonest allergen (7 of 24 patients, 29.2%) while potassium dichromate, cobalt chloride hexahydrate and nickel positivity were observed in five patients each [Figure 1]. Similarly, at 96 h, fragrance mix and cobalt chloride hexahydrate were positive in seven patients each, and potassium dichromate and nickel positivity were seen in five patients each [Figure 2]. Gentamicin sulphate was found positive in four patients. Table 2 describes the patch test positivity with Indian standard series components in detail with the grading of positive reactions. On comparing patients having a positive patch test with those having negative patch tests, no significant difference was observed for age, sex, disease duration, presence of atopy and mean serum IgE levels [Table 3]. However, SCORAD was significantly higher in patients with positive patch tests as compared to patients with negative patch tests (27.4 ± 13.3 vs 20.5 ± 11.0, respectively; P = 0.009). Raised IgE levels were observed in 25/28 (89.3%) patients with positive patch tests as compared to 79/104 (75.9%) patients with negative patch tests (P = 0.08).
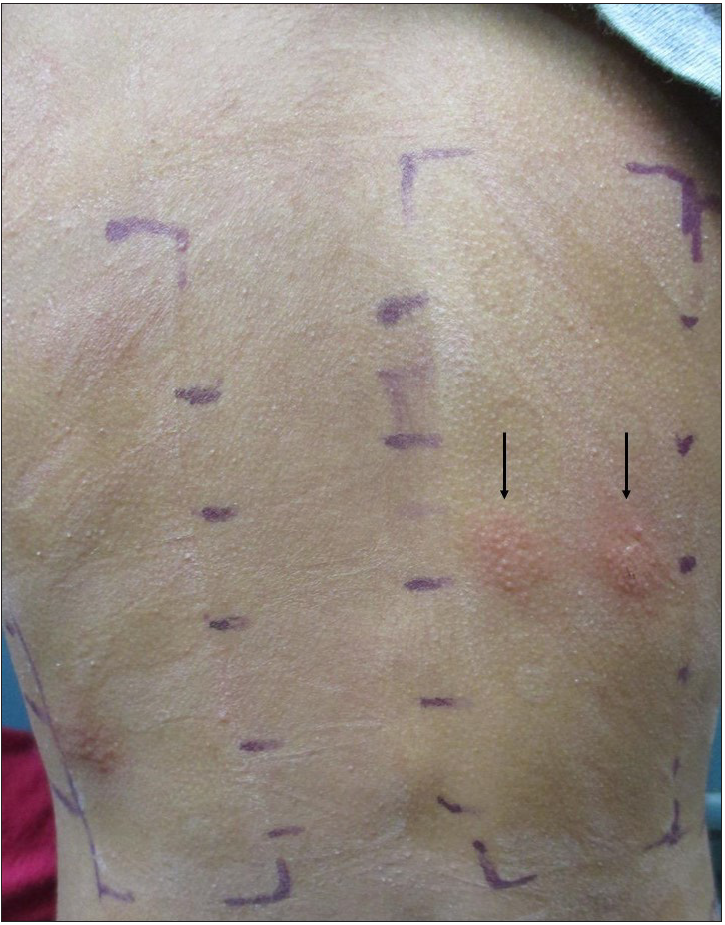
- Patch test positivity (2+) to both parthenium and thiuram mix at 96 h.
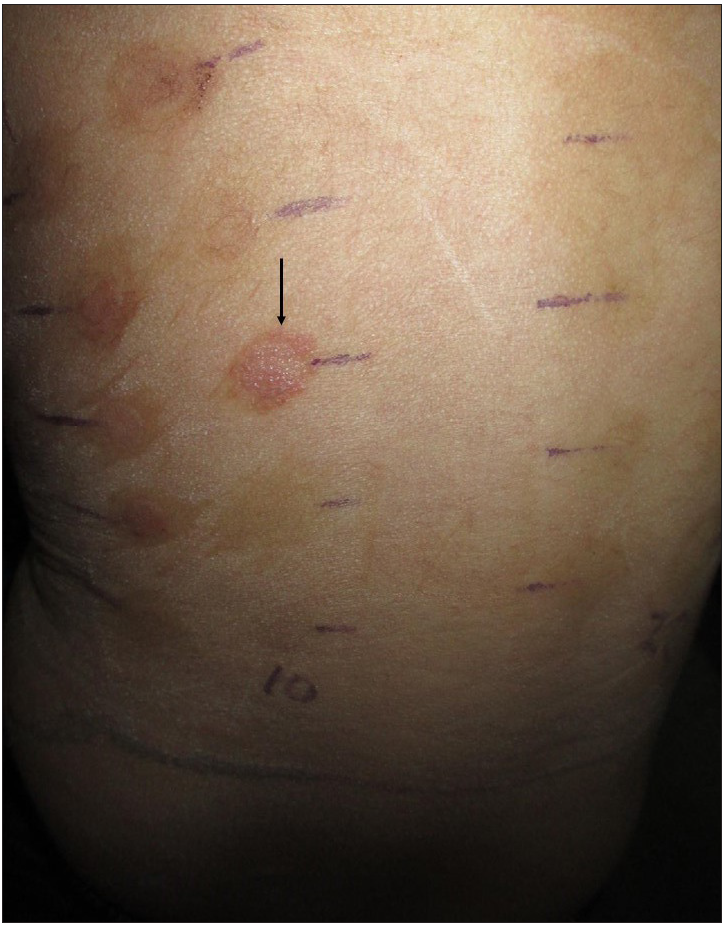
- Patch test positivity (2+) to cobalt sulphate at 96 h.
| ISS component | Number of patients with positive patch test at 48 h, n = 24* | Number of patients with positive patch test at 96 h, n = 28* | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | 1+ | 2+ | 3+ | Total | 1+ | 2+ | 3+ | |
| Potassium dichromate | 5 (20.8%) | 4 (16.7%) | 1 (4.2%) | 0 (0.0%) | 5 (20.8%) | 4 (16.7%) | 1 (4.2%) | 0 (0.0%) |
| Cobalt (II) chloride hexahydrate | 5 (20.8%) | 3 (12.5%) | 2 (8.3%) | 0 (0.0%) | 7 (29.2%) | 5 (20.8%) | 2 (8.3%) | 0 (0.0%) |
| Benzocaine | 2 (8.3%) | 2 (8.3%) | 0 (0.0%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) |
| Paraben mix | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) |
| Nickel sulphate hexahydrate | 5 (20.8%) | 4 (16.7%) | 1 (4.2%) | 0 (0.0%) | 5 (20.8%) | 4 (16.7%) | 1 (4.2%) | 0 (0.0%) |
| Colophony | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) |
| Gentamycin sulphate | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) | 4 (16.7%) | 4 (16.7%) | 0 (0.0%) | 0 (0.0%) |
| Mercapto mix | 2 (8.3%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 1 (4.2%) | 0 (0.0%) | 1 (4.2%) | 0 (0.0%) |
| Fragrance mix | 7 (29.2%) | 5 (20.8%) | 2 (8.3%) | 0 (0.0%) | 7 (29.2%) | 5 (20.8%) | 2 (8.3%) | 0 (0.0%) |
| Wood alcohol | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (4.2%) | 0 (0.0%) | 1 (4.2%) | 0 (0.0%) |
| Balsam of Peru | 2 (8.3%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) | 2 (8.3%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) |
| Black rubber mix | 1 (4.2%) | 0 (0.0%) | 1 (4.2%) | 0 (0.0%) | 2 (8.3%) | 0 (0.0%) | 2 (8.3%) | 0 (0.0%) |
| 4-Butylphenolformaldehyde resin | 2 (8.3%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 2 (8.3%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) |
| Polyethylene glycol(PEG 400) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) | 1 (4.2%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) |
| Parthenolide | 1 (4.%) | 1 (4.2%) | 0 (0.0%) | 0 (0.0%) | 2 (8.3%) | 2 (8.3%) | 0 (0.0%) | 0 (0.0%) |
ISS: Indian Standard Series
| Feature | Patients with a positive patch test | Patients with a negative patch test | P |
|---|---|---|---|
| Age (years); mean ± SD | 5.0 ± 3.2 | 5.8 ± 3.3 | 0.2 |
| Number of males (%) | 20/28 (71.4) | 60/108 (55.5) | 0.13 |
| Duration (months); mean ± SD | 38.4 ± 33.9 | 33.3 ± 27.3 | 0.43 |
| Number of patients with atopy (%) | 7/28 (25) | 25/108 (23.1) | 0.84 |
| SCORAD; mean ± SD | 27.35 ± 13.25 | 20.54 ± 10.93 | 0.009 |
| S. IgE, mean ± SD | 1215.7 ± 2251.7 | 1457.6 ± 3492.7 | 0.74 |
Discussion
It continues to be a matter of debate whether or not atopic dermatitis increases the risk of contact allergy. Clinically, it is difficult to differentiate contact dermatitis from atopic dermatitis, especially in the common areas of involvement, such as the eyelids, lips, hands and flexural areas of the neck, and also when there is dermatitis with a scattered generalised distribution. A patch test is useful in this regard to determine sensitisation to specific allergens. However, the clinical relevance of positive patch test reactions should be established by carefully correlating the patient’s history including details regarding possible exposure to the allergen, site and type of exposure, with the test results. It is the role of the clinician to determine if a positive patch test result is relevant or not, and this is often one of the most difficult aspects of patch testing. Reported relevance in published studies is determined by standards used by the North American Contact Dermatitis Group (NACDG).3 NACDG defines current relevance as definite if there is a positive patch test or provocative use test of an article belonging the patient known to contain the allergen, probable if the antigen is present in known skin contactants and the clinical presentation is consistent with that exposure, or possible if skin contact with materials known to contain the allergen is likely. The most concrete proof of relevance is the improvement or resolution of dermatitis after avoidance of the allergen.4 Past relevance is considered if the patch test is positive, but Table 3 exposure was in the past and the patient is not currently exposed to that allergen.5
A limited number of studies have investigated the overlap of atopic dermatitis and allergic contact dermatitis in children. A systematic review of patch test results in children found studies both revealing and refuting a statistical difference between patients with and without atopic dermatitis.6 In addition, uncovering any allergic contact dermatitis and subsequent avoidance of allergens could lead to improvement in the patient’s atopic dermatitis symptoms. Patch test positivity in children ranges from 20 to 95.6%.6–8 In a cross-sectional survey of 82 children with atopic dermatitis who were patch tested with the children’s baseline series and a corticosteroid series, positive reactions were seen in 26.8%.9 In a recent review of contact allergy in children, the prevalence of positive patch test results in selected populations (children with suspected allergic contact dermatitis, recalcitrant atopic dermatitis or eczema) ranged from 27 to 96%, with relevance established in 52–100%.10 In a study from north India, patch test positivity was found in 33% of atopic dermatitis patients with common allergens being nickel, cobalt chloride, neomycin sulphate, fragrance mix, potassium dichromate and paraphenylenediamine.11 In another north Indian study, patch test positivity was high with 54.3% of patients being positive for one or more allergens, and nickel sulphate was the most common allergen.12 In our study, 20.6% of children were positive for various allergens of Indian standard series at 96 h. Multiple studies have found increased sensitisation rates to various allergens among children with atopic dermatitis, including potassium dichromate, compositae mix, disperse blue, balsam of Peru, fragrance mix, nickel, cobalt, wool alcohols, neomycin, colophony, thiomersal and lanolin.7,9,13 Similarly, the most common allergens in our study were fragrance mix, potassium dichromate, cobalt chloride and nickel sulphate. The relevance of positive patch tests was difficult to be established in our cohort. Due to the ubiquitous nature of the allergens, especially fragrance, metals and rubber chemicals, they were deemed relevant. We could not establish relevance in children positive for the other allergens. The majority of patients in our study with positive patch tests were boys in contrast to the previous study on contact sensitisation in a paediatric atopic dermatitis population in Laos.8 A retrospective analysis showed that eczema area and severity index scores greater than 10 correlated with a higher probability of more than three positive patch tests.7 In our study, higher SCORAD was found to be associated with patch test positivity. Similarly, a prospective study from Tunisia of 89 children and adults with atopic dermatitis found that the more severe the atopic dermatitis, the more frequent was the patch test positivity.14
In a retrospective case review of 1142 children patch tested by 84 health care providers from across the United States,15 patch-tested patients with atopic dermatitis were found to be significantly younger with more generalised and a longer history of dermatitis compared with those without atopic dermatitis. In our study, no difference in age and duration of disease was found between patch-test positive and -negative patients.
Inability to establish relevance in about 50% of the patients was a limitation of our study. Participants and their parents were advised to avoid the allergens which they had tested positive for. Follow-up data regarding assessment of the impact of allergens avoidance was not available and hence are not included in this study.
Conclusion
In the present study, approximately one-fifth of the atopic dermatitis patients were found to have a positive patch test. The most common allergens resulting in positive patch tests were fragrance mix, potassium dichromate, cobalt chloride hexahydrate and nickel. High SCORAD, i.e., higher disease severity was found to be associated with patch test positivity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Basis for the barrier abnormality in atopic dermatitis: Outside-inside-outside pathogenic mechanisms. J Allergy Clin Immunol. 2008;121:1337-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The epidemiology of contact allergy in the general population—Prevalence and main findings. Contact Dermatitis. 2007;57:287-99.
- [CrossRef] [PubMed] [Google Scholar]
- North American contact dermatitis group patch test results for 2007–2008. Dermatitis. 2013;24:10-21.
- [CrossRef] [PubMed] [Google Scholar]
- Patch testing in children from 2005 to 2012: Results from the North American contact dermatitis group. Dermatitis. 2014;25:345-55.
- [CrossRef] [PubMed] [Google Scholar]
- North American Contact Dermatitis Group patch test results: 2009 to 2010. Dermatitis. 2013;24:50-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patch-test results in children and adolescents: Systematic review of a 15-year period. An Bras Dermatol. 2016;91:64-72.
- [Google Scholar]
- Frequency of contact allergens in pediatric patients with atopic dermatitis. J Clin Aesthet Dermatol. 2011;4:39-41.
- [Google Scholar]
- Patch test results in pediatric patients with atopic dermatitis in Laos. PLoS One. 2020;15:e0231455.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Children with atopic dermatitis should always be patch-tested if they have hand or foot dermatitis. Acta Derm Venereol. 2015;95:583-6.
- [CrossRef] [PubMed] [Google Scholar]
- Contact allergy and allergic contact dermatitis in children—A review of current data. Contact Dermatitis. 2011;65:254-65.
- [CrossRef] [PubMed] [Google Scholar]
- Patch testing in children: An experience from Kashmir. Indian J Dermatol Venereol Leprol. 2016;82:186-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patch testing in children and adolescents with suspected allergic contact dermatitis. Skinmed. 2016;14:253-8.
- [PubMed] [Google Scholar]
- Contact sensitization in children: A retrospective study of 2,614 children from a single center. Pediatr Dermatol. 2016;33:399-404.
- [CrossRef] [PubMed] [Google Scholar]
- Contact sensitization in atopic dermatitis: Results of a prospective study of 89 cases in Tunisia. Contact Dermatitis. 2008;58:188-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric contact dermatitis registry data on contact allergy in children with atopic dermatitis. JAMA Dermatol. 2017;153:765-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






