Translate this page into:
Dermoscopy of nevus sebaceus: A cross-sectional study of 22 cases
Corresponding author: Dr. Shekhar Neema, Department of Dermatology, Armed Forces Medical College Pune, Pune, Maharashtra, India. shekharadvait@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sandhu S, Neema S, Singh PY, Dangwal V, Kothari R. Dermoscopy of nevus sebaceus: A cross-sectional observational study of 22 cases. Indian J Dermatol Venereol Leprol. 2024;90:367-72. doi: 10.25259/IJDVL_629_2022
Dear Editor,
Nevus sebaceus of Jadassohn (NS) is a cutaneous hamartoma classically evolving from an alopecic yellowish patch during infantile stage to verrucous in adulthood with yellow lobular appearance, and finally to nodular or tumoral appearance with peripheral telangiectasias.1 Multiple tumors, both benign and malignant, such as trichoblastoma, syringocystadenoma papilleferum and basal cell carcinoma may develop secondarily over nevus sebaceus . Benign tumours and malignant growth are seen in 13.6% and 1– 2.5% of nevus sebaceus cases, respectively.2 The risk of malignant transformation increases with age.3 Hence, regular follow-up is needed for early detection of neoplasms. Dermoscopy, a non-invasive modality, can be utilised for its early diagnosis and follow-up. We aim to describe different dermoscopic patterns of nevus sebaceus according to its evolutionary stages.
We conducted a cross-sectional study from Jun 2019 to May 2021 in an Indian tertiary care center. A total of 22 patients with clinico-histopathological diagnosis of nevus sebaceus at various evolutionary stages were enrolled in the study, and the mean age was 27.14 years (range: 3–65 years). There was male preponderance (M:F = 18:4). Nevus sebaceus was located on scalp in 15 (68.1%) and on face in 7 (31.8%) patients. Alopecic patch was present in two (9%) patients, slightly elevated plaque in nine (40.9%), verrucous plaque in eight (36.3%) and verrucous plaque with nodules in three (13.6%). All patients underwent histopathology using 4 mm punch. It was consistent with nevus sebaceus alone in 19 (86.3%) patients, while features suggestive of syringocystadenoma papilleferum were reported in 3 (13.8%) patients. It showed three patterns (1) Patch stage revealed normal epidermis with numerous sebaceous glands which were hyperplastic and small primordial hair follicles [Figure 1a]; (2) Plaque stage showed papillomatosis and acanthosis with sebaceous gland hyperplasia, ectopic apocrine glands and primordial hair follicles [Figure 1b]; and (3) nevus sebaceus with syringocystadenoma papilleferum revealed papillomatosis with several cystic invaginations extending into the dermis, forming small cystic areas lined by double layer of cuboidal to columnar epithelial cells with pale eosinophilic cytoplasm. Some of these cells showed decapitation secretion. The stroma contained a dense mononuclear cell infiltrate, comprising predominantly of plasma cells. Hyperplastic sebaceous glands were also noted. [Figure 1c].
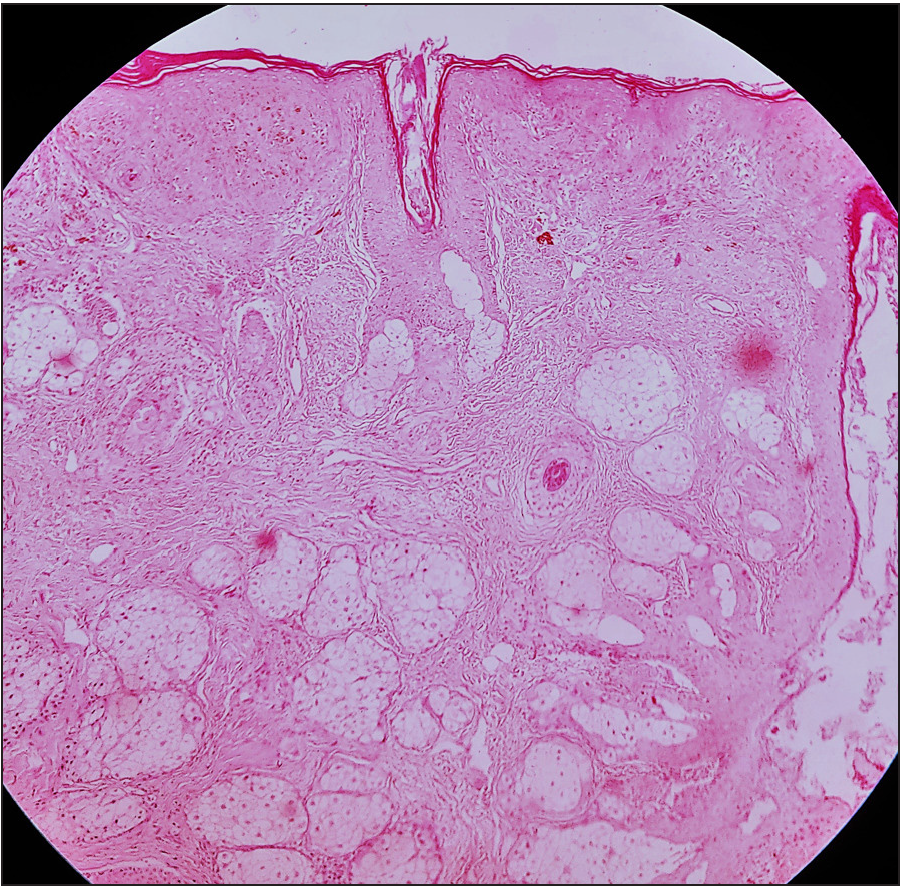
- Patch stage of nevus sebaceus showing normal epidermis with numerous, hyperplastic sebaceous glands and small, primordial hair follicles (H & E, 40x)
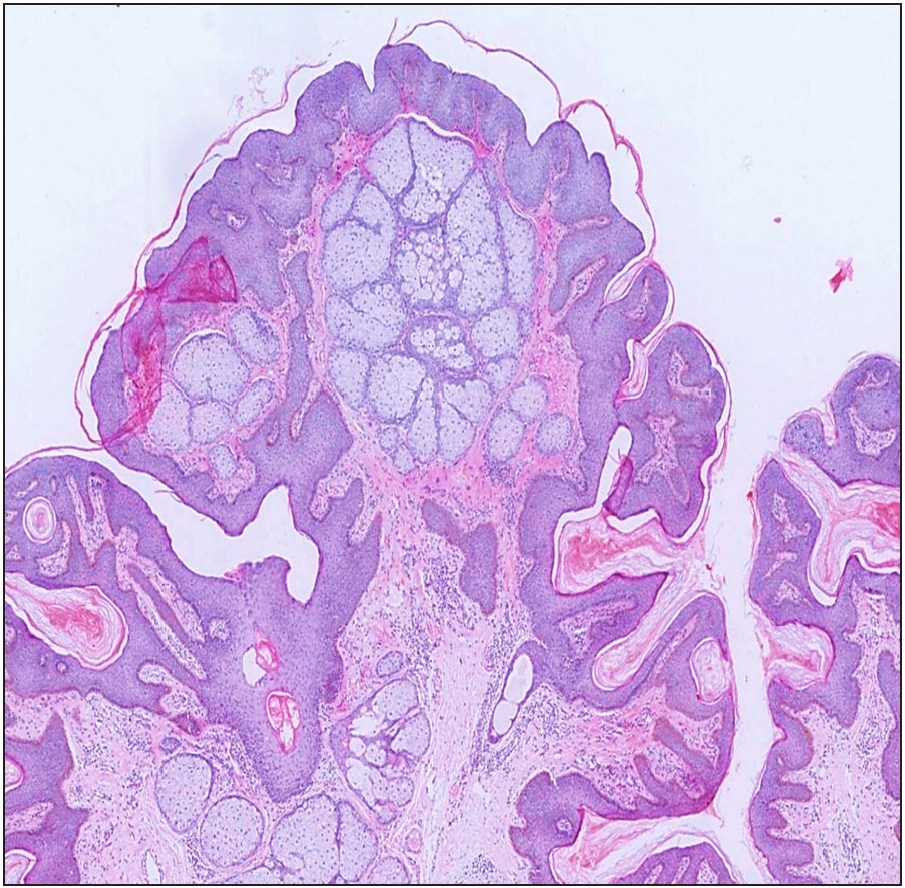
- Plaque stage of nevus sebaceus revealing papillomatosis and epithelial hyperplasia with sebaceous gland hyperplasia, ectopic apocrine glands and primordial hair follicles (H & E, 40x)
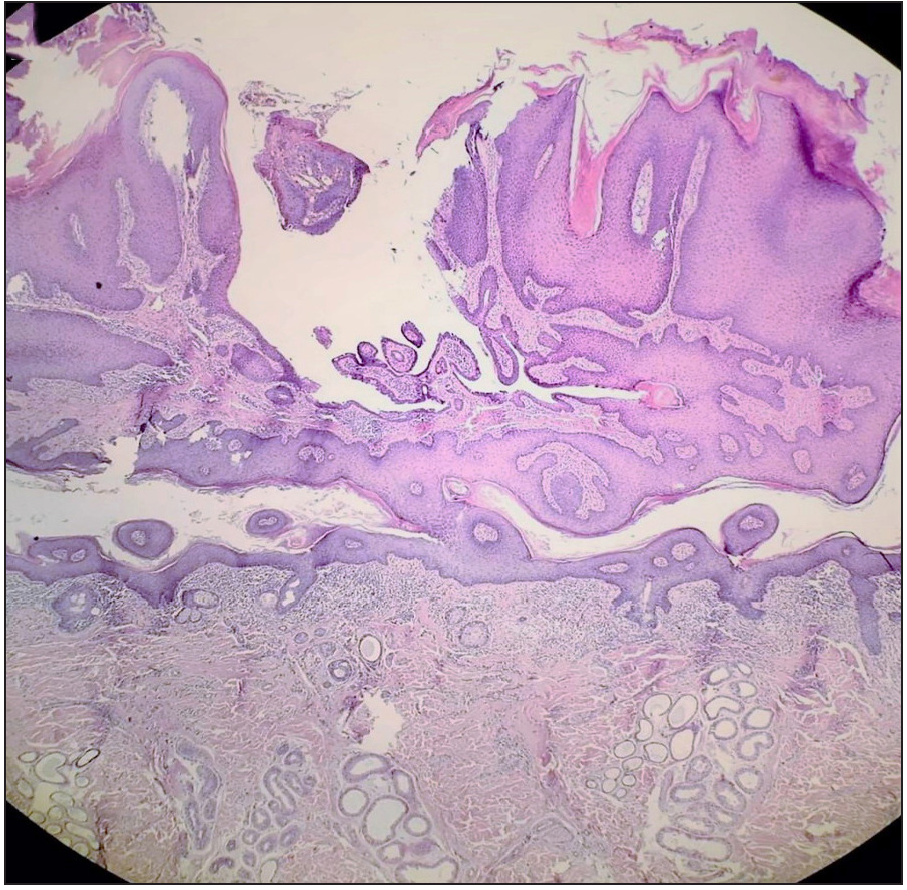
- Histopathology of nevus sebaceus with syringocystadenoma papilleferum showing papillomatosis with several cystic invaginations forming small cystic areas lined by double layer of cuboidal to columnar epithelial cells. Few decapitation secretions seen. Dense mononuclear cell infiltrate in the papillary dermis and numerous ectopic apocrine glands are seen (H & E, 40x)
Dermoscopic features are shown in Tables 1 and 2. Patch stage (n = 2) showed yellow globules (YG) arranged in clusters on a yellowish to pinkish yellow background [Figure 2a]. Slightly elevated plaque (n = 9) showed two patterns: (1) brown globules (BG) in crateriform pattern in six (66.6%) patients [Figure 2b] and (2) brown and orange globules (OG) in cobblestone pattern in three (33.3%) patients, which was suggestive of transition phase [Figure 2c]. Verrucous plaque with histology of nevus sebaceus alone (n = 8) showed three patterns: (1) only brown globules in cerebriform pattern in two (25%) patients [Figure 3a]; (2) brown globules in cerebriform pattern along with greyish to white exophytic papillary projections (EPP) at places, dotted to polymorphous vessels and yellow to white scales among three (37.5%) patients and crusted erosions among two (25%) patients [Figure 3b]; and (3) brown globules in cerebriform pattern with homogenous yellow globules in three (37.5%) patients with morphology of verrucous plaques with nodules [Figure 3c]. Verrucous plaque of nevus sebaceus in all these eight patients showed evolution from crateriform to cerebriform pattern and to homogenous yellow globules from periphery towards the centre. [Figure 3d].
| Case number | Age (years) | Sex | Location | Clinical Morphology | Histopathological diagnosis | Dermoscopic features |
|---|---|---|---|---|---|---|
| 1 | 32 | M | Face | Plaque | NS |
BG in cerebriform pattern at plaques. YG aggregated in clusters over yellow background at slightly elevated plaque |
| 2 | 13 | F | Temporal | Plaque | NS | BG with central crater pattern |
| 3 | 55 | M | Vertex | Patch | NS | YG arranged in clusters on a yellow background |
| 4 | 22 | F | Parietal | Plaque | NS | BG with central crater |
| 5 | 7 | M | Frontal | Plaque | NS | Orange globules and BG in cobblestone pattern (Transition phase), Greyish EPP at places, yellow white scales, linear vessels |
| 6 | 65 | M | Vertex | Verrucous plaque | NS with SCAP | BG at places, EPP, crust, erosion, dotted vessels, yellow white scales |
| 7 | 24 | M | Vertex | Alopecic Plaque | NS | BG and orange globules in cerebriform pattern (Transition phase) |
| 8 | 24 | M | Vertex | Patch | NS | YG aggregated on a pinkish yellow background |
| 9 | 18 | M | Vertex | Verrucous plaque | NS with SCAP | BG at places, EPP, dotted and polymorphous vessels, erosions, white scales |
| 10 | 24 | M | Forehead | Verrucous Plaque | NS | BG in cerebriform pattern, whitish EPP, dotted and linear vessels, white scales |
| 11 | 25 | M | Temporal | Plaque with nodules | NS | BG in cerebriform pattern, yellow homogenous structures |
| 12 | 52 | M | Face | Verrucous plaque | NS | BG in cerebriform pattern, erosion, crust, polymorphic vessels, white scales |
| 13 | 50 | M | Temporal | Plaque | NS | Brown yellow globules with central crater |
| 14 | 26 | M | Vertex | Verrucous plaque | NS with SCAP | BG at places, pinkish yellow EPP, linear vessels, yellow scales, crust |
| 15 | 16 | F | Face | Slightly elevated plaque | NS | BG in crater pattern |
| 16 | 26 | M | Temporal | Nodules to verrucous plaque | NS | Yellow homogenous globules to BG in cerebriform pattern, dotted vessel |
| 17 | 24 | M | Preauricular | Plaque with nodules | NS | Brown-yellow globules in cerebriform pattern, yellow homogenous structures |
| 18 | 14 | M | Face | Verrucous plaque | NS | Grayish EPP, BG in cerebriform pattern |
| 19 | 26 | M | Parietal | Verrucous plaque | NS | BG in cerebriform pattern and crater pattern with peripheral striations, erosion (edge) |
| 20 | 26 | M | Vertex | Verrucous plaque | NS | EPP, linear vessels, yellow scales, BG in cerebriform pattern |
| 21 | 25 | F | Vertex | Plaque | NS | BG and orange globules in cerebriform pattern (Transition phase) |
| 22 | 3 | M | Face (cheek) | Plaque | NS | BG with central crateriform pattern |
BG: Brown globules; EPP: Exophytic papillary projections; F: Female; M: Male; NS: Nevus sebaceus; SCAP: Syringocystadenoma papilleferum; YG: Yellow globules
| Morphology of NS | Histopathological diagnosis | Number of cases | Dermoscopic finding with frequency (in numbers) |
|---|---|---|---|
| Patch | NS | 2 | YG arranged in clusters on a yellow or pinkish yellow background (2) |
| Plaque | NS | 9 |
BG with central crater pattern (6) BG and orange globules in cobblestone pattern: Transition phase (3) |
| Verrucous plaque | NS | 5 |
BG in cerebriform pattern (5) EPP [at places] (3) Dotted or polymorphous vessels [at places] (3) Scales [white or yellow at places] (3) Erosions or crust [at places] (2) |
| NS with SCAP | 3 |
BG at places (3) Predominant EPP (3) Dotted, linear or polymorphous vessels (3) Erosions or crust (3) Scales (white or yellow) (3) |
|
| Verrucous plaque with nodules | NS | 3 |
Yellow homogenous globules or structures (3) BG in cerebriform pattern (3) |
BG: Brown globules; YG: Yellow globules; EPP: Exophytic papillary projections; NS: Nevus sebaceus; SCAP: Syringocystadenoma papilleferum
![Yellow globules (yellow stars) arranged in clusters over a yellow background seen in dermoscopy of patch stage of nevus sebaceus (Dermlite DL4, 10X polarised). [Inset: Clinical alopecic patch in childhood stage of NS over vertex of scalp in an adult]](/content/126/2024/90/3/img/IJDVL-90-3-367-g4.png)
- Yellow globules (yellow stars) arranged in clusters over a yellow background seen in dermoscopy of patch stage of nevus sebaceus (Dermlite DL4, 10X polarised). [Inset: Clinical alopecic patch in childhood stage of NS over vertex of scalp in an adult]
![Brown globules in crateriform pattern (yellow arrows) seen in dermoscopy of slightly elevated plaque (Dermlite DL4, 10X polarised). [Inset: Slightly elevated plaque located over temporo-parietal region of scalp]](/content/126/2024/90/3/img/IJDVL-90-3-367-g5.png)
- Brown globules in crateriform pattern (yellow arrows) seen in dermoscopy of slightly elevated plaque (Dermlite DL4, 10X polarised). [Inset: Slightly elevated plaque located over temporo-parietal region of scalp]
![Dermoscopy showing brown and orange globules in cobblestone pattern (blue star) suggestive of transition phase (Dermlite DL4, 10X polarised). [Inset: Elevated hyperpigmented plaque over vertex of scalp in an adult]](/content/126/2024/90/3/img/IJDVL-90-3-367-g6.png)
- Dermoscopy showing brown and orange globules in cobblestone pattern (blue star) suggestive of transition phase (Dermlite DL4, 10X polarised). [Inset: Elevated hyperpigmented plaque over vertex of scalp in an adult]
![Dermoscopy of an evolving verrucous plaque alone showing brown globules in cerebriform pattern (red star) (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque in adulthood stage of NS]](/content/126/2024/90/3/img/IJDVL-90-3-367-g7.png)
- Dermoscopy of an evolving verrucous plaque alone showing brown globules in cerebriform pattern (red star) (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque in adulthood stage of NS]
![Dermoscopy of an evolving verrucous plaque showing brown globules in cerebriform pattern (yellow star) along with at places, greyish to white exophytic papillary projections with linear vessels and white scales (yellow circles) (Dermlite DL4, 10X polarised). [Inset: Hyperpigmented verrucous plaque over forehead]](/content/126/2024/90/3/img/IJDVL-90-3-367-g8.png)
- Dermoscopy of an evolving verrucous plaque showing brown globules in cerebriform pattern (yellow star) along with at places, greyish to white exophytic papillary projections with linear vessels and white scales (yellow circles) (Dermlite DL4, 10X polarised). [Inset: Hyperpigmented verrucous plaque over forehead]
![Dermoscopy of verrucous plaque with nodules showing predominant yellow homogenous globules (red circle) along with brown globules (blue star) in cerebriform pattern (Dermlite DL4, 10X polarised). [Inset: Plaque with verrucous surface and yellow nodules over temporal region of scalp]](/content/126/2024/90/3/img/IJDVL-90-3-367-g9.png)
- Dermoscopy of verrucous plaque with nodules showing predominant yellow homogenous globules (red circle) along with brown globules (blue star) in cerebriform pattern (Dermlite DL4, 10X polarised). [Inset: Plaque with verrucous surface and yellow nodules over temporal region of scalp]
![Dermoscopy of an evolved verrucous plaque showing crateriform pattern (red arrow) at periphery to cerebriform pattern (yellow star) to yellow homogenous globules (blue star) towards centre of NS (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque over temporal region of scalp]](/content/126/2024/90/3/img/IJDVL-90-3-367-g10.png)
- Dermoscopy of an evolved verrucous plaque showing crateriform pattern (red arrow) at periphery to cerebriform pattern (yellow star) to yellow homogenous globules (blue star) towards centre of NS (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque over temporal region of scalp]
All three patients with histopathological diagnosis of nevus sebaceus with syringocystadenoma papilleferum showed predominantly greyish white exophytic papillary projections with dotted, linear or polymorphous vessels, erosions or crust and scales (white or yellow) with brown globules in cerebriform pattern at places [Figures 4a and 4b].
![Dermoscopy of nevus sebaceus with syringocystadenoma papilleferum depicting predominantly greyish white exophytic papillary projections (blue stars) with linear and polymorphous vessels and white scales with brown globules (yellow circle) in cerebriform pattern at places (Dermlite DL4, 10X polarised). [Inset: Plaque over vertex with verrucous surface and papillary projections]](/content/126/2024/90/3/img/IJDVL-90-3-367-g11.png)
- Dermoscopy of nevus sebaceus with syringocystadenoma papilleferum depicting predominantly greyish white exophytic papillary projections (blue stars) with linear and polymorphous vessels and white scales with brown globules (yellow circle) in cerebriform pattern at places (Dermlite DL4, 10X polarised). [Inset: Plaque over vertex with verrucous surface and papillary projections]
![Dermoscopy of nevus sebaceus with syringocystadenoma papilleferum showing greyish exophytic papillary projections with polymorphous vessels and white scales, predominant erosions, crust and yellow white scales (yellow star) (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque of nevus sebaceus over vertex]](/content/126/2024/90/3/img/IJDVL-90-3-367-g12.png)
- Dermoscopy of nevus sebaceus with syringocystadenoma papilleferum showing greyish exophytic papillary projections with polymorphous vessels and white scales, predominant erosions, crust and yellow white scales (yellow star) (Dermlite DL4, 10X polarised). [Inset: Verrucous plaque of nevus sebaceus over vertex]
Discussion
Clinically, it is difficult to differentiate nevus sebaceus from aplasia cutis congenita (ACC) in an infant. The infantile stage of this condition is characterised by clustered yellow globules on a yellow background or bright yellow dots not associated with hair follicles. Dermoscopy in aplasia cutis congenita reveals absence of follicular ostia at the centre with radially arranged hair follicles at hair bearing margin forming a ring of hypertrichosis or starburst pattern with dark pigmented ends of these elongated hair bulbs visible through the translucent epidermis. Some telangiectasia are visible over the patch.4
In the childhood stage, lesions evolve from patches to slightly elevated plaques. Yellow globules in cobblestone pattern are seen corresponding to numerous hyperplastic sebaceous glands.3,5 However, we observed unique orange–brown globules in cobblestone pattern suggestive of transition phase in slightly elevated plaques in three (33.3%) patients and brown globules in crateriform pattern in six (66.6%) patients in the elevated plaque lesions. Orange globules represent immature sebaceous glands, while brown globules correspond to hyperplastic, mature sebaceous glands.
In the adult stage with verrucous plaque to nodular lesions, brown gobules in cerebriform pattern with fissures and ridges to crateriform pattern with peripheral striations to whitish yellow lobular or yellow–greyish papillary structures, in verrucous plaque and homogenous yellow appearance in nodular lesions with linear irregular and arborescent vessels have been described previously.3,5 We observed brown gobules from crateriform pattern to cerebriform pattern in all eight (100%) patients with verrucous plaque of nevus sebaceus alone from periphery towards centre, and evolved yellow nodules at centre suggestive of maximum epithelial hyperplasia and papillomatosis in HPE at centre and decreasing towards periphery of lesion. This shows maximum evolution of nevus sebaceus at the centre with peripheral dispersion. We did not find any telangiectasia in these nodules.
Secondary syringocystadenoma papilleferum associated with nevus sebaceus is seen in 5.2–13% cases.2 We encountered three (13.6%) such cases. Dermoscopic features of all 3 cases were predominantly greyish white exophytic papillary projections with dotted, linear or polymorphous vessels, erosions or crust, white or yellow scales with brown globules in cerebriform pattern at places. Hence, replacement of majority of brown or yellow globules to exophytic papillary projections with vessels, erosions, crusts and scales suggested evolution of nevus sebaceus to syringocystadenoma papilleferum which was confirmed histopathologically. In a previous study, syringocystadenoma papilleferum was the second commonest benign neoplasia occurring in nevus sebaceus in 9 out of 23 (15.6%) cases. Dermoscopic features described were symmetric erythematous lesion with “exophytic papillary structures” (78% of cases; 7/9), central depression (66.7%; 6/9), erosions or crusts or ulceration (89%; 8/9) and vascular structures in 100% of cases.6 Central depression and ulceration in dermoscopy of syringocystadenoma papilleferum may correspond to invaginating cystic spaces opening to skin surface on histopathology. Papillomatosis and papillary projections into cystic space on histopathology represent exophytic papillary projections, while presence of vessels on dermoscopy might be explained by fibrovascular core supporting these projections. Dermoscopy of the entire lesion should be performed to look for development of secondary syringocystadenoma papilleferum within nevus sebaceus.
Conclusion
This is an analysis of the dermoscopic features of nevus sebaceus as per the evolutionary stages in 22 cases. Though, a correlation between dermoscopy and histopathology is always advocated, the above dermoscopic features can guide the clinician towards a diagnosis and its progression to neoplasm without undergoing invasive biopsy or excision especially over the face.
Limitations
The study is limited by small sample size and unavailability of tumours other than syringocystadenoma papilleferum in analysis.
Acknowledgements
The patients or guardians of minors enrolled in this study have given written informed consent for the publication of their case details.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Appendage tumours and hamartomas of the skin. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, eds. Fitzpatrick’s Dermatology in General Medicine (8th ed). New York: McGraw-Hill Companies, Inc; 2012. p. :1375-6.
- [Google Scholar]
- Secondary neoplasms associated with nevus sebaceus of Jadassohn: A study of 707 cases. J Am Acad Dermatol. 2014;70:332-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic analysis of nevus sebaceus of Jadassohn: A study of 13 cases. Ski Appendage Disord. 2017;3:83-91.
- [Google Scholar]
- Starburst hair follicles: A dermoscopic clue for aplasia cutis congenita. J Am Acad Dermatol. 2016;75:e141-2.
- [CrossRef] [PubMed] [Google Scholar]
- Trichoscopy: The best auxiliary tool in the evaluation of nevus sebaceous. Int J Trichology. 2016;8:5-10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy of tumours arising in naevus sebaceous: A morphological study of 58 cases. J Eur Acad Dermatology Venereol.. 2015;29:2231-7.
- [Google Scholar]





